Differentiating Diabetes insipidus from other diseases: Difference between revisions
Ahmed Younes (talk | contribs) No edit summary |
|||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
[[Image:Home_logo1.png|right|250px|link=https://www.wikidoc.org/index.php/Diabetes_insipidus]] | |||
{{CMG}}; {{AE}} {{DAMI}} | {{CMG}}; {{AE}} {{DAMI}} | ||
Latest revision as of 18:20, 25 February 2019

Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Omodamola Aje B.Sc, M.D. [2]
Overview
The most important differential diagnosis for diabetes insipidus include: Central diabetes insipidus, acquired, Trauma (surgery, deceleration injury), Vascular (cerebral hemorrhage, infarction, anterior communicating artery aneurysm or ligation, intra-hypothalamic hemorrhage), Neoplastic (craniopharyngioma, meningioma, germinoma, pituitary tumor or metastases), Granulomatous (histiocytosis, sarcoidosis), Infectious (meningitis, encephalitis), Inflammatory/autoimmune (lymphocytic infundibuloneurohypophysitis), Drug/toxin-induced (ethanol, diphenylhydantoin, snake venom), hydrocephalus, Idiopathic, congenital, Congenital malformations, nephrogenic diabetes insipidus: Acquired, drug-induced (demeclocycline, lithium, cisplatin, methoxyflurane, etc.), Hypercalcemia, hypokalemia, infiltrating lesions (sarcoidosis, amyloidosis, multiple myeloma, Sjogren's disease), Vascular (sickle cell disease), congenital, X-linked recessive, primary polydipsia,Psychogenic, dipsogenic (downward resetting of thirst threshold), gestational diabetes insipidus, Diabetes mellitus.
Differentiating diabetes insipidus based on the type of diabetes insipidus caused
The most important differential diagnosis for diabetes insipidus include:[1][2][3]
| Type of DI | Subclass | Disease | Defining signs and symptoms | Lab/Imaging findings |
|---|---|---|---|---|
| Central | Acquired | Histiocytosis |
|
 |
| Craniopharyngioma |
|
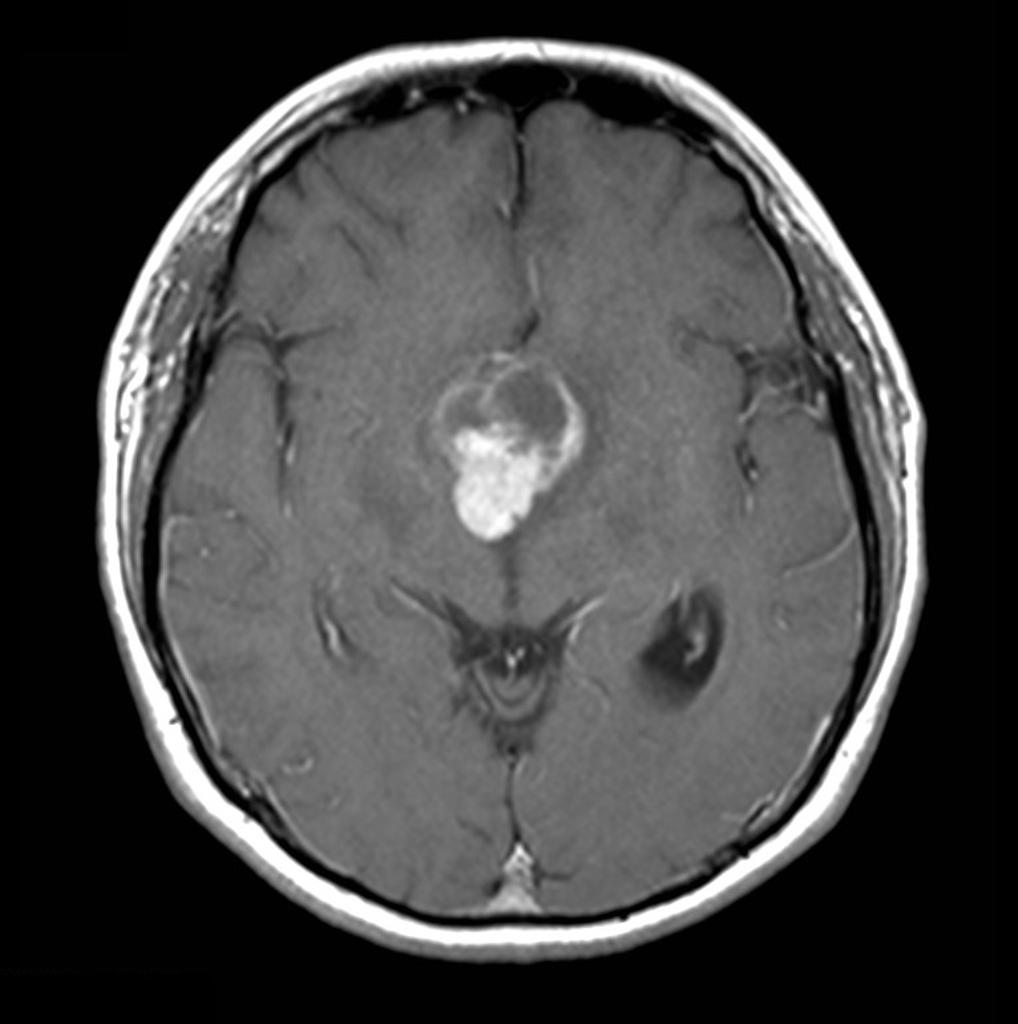 | ||
| Sarcoidosis |
|
 | ||
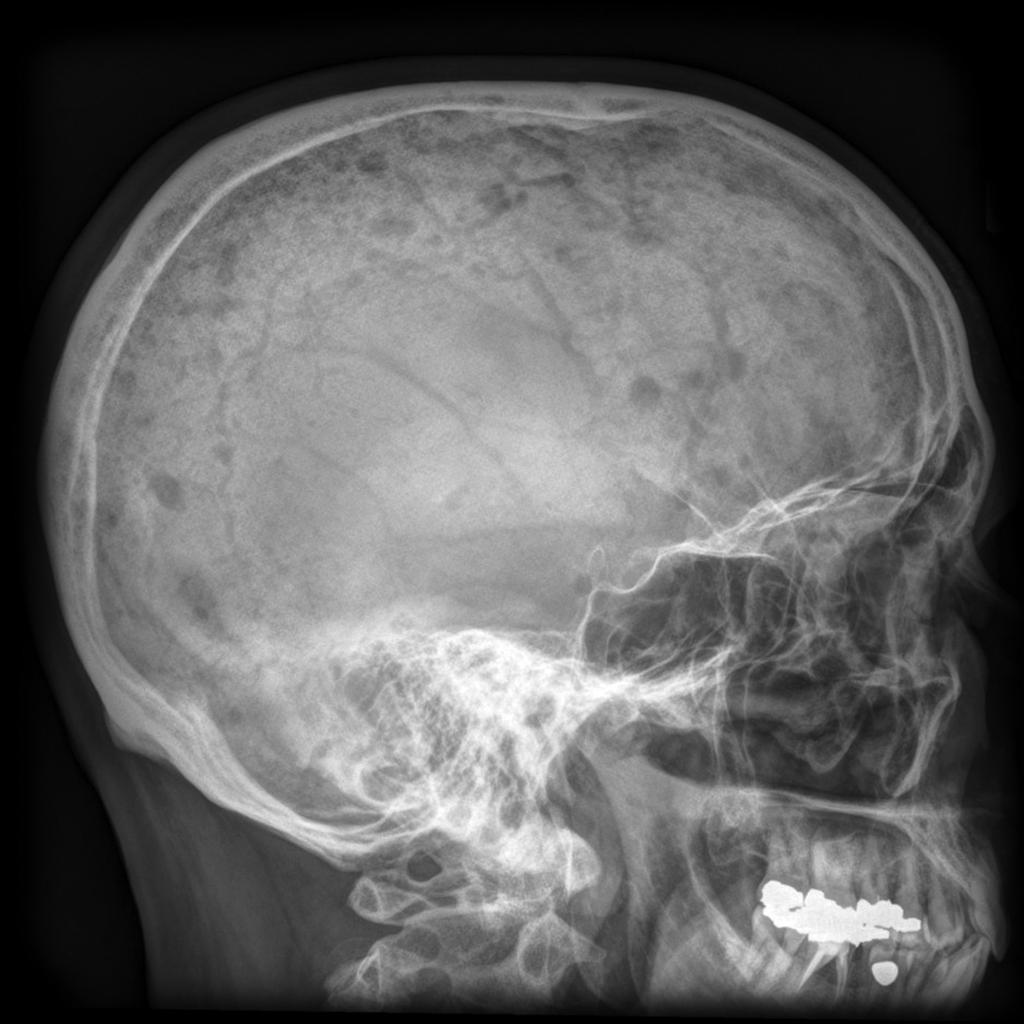
| Congenital | Hydrocephalus |
|
Dilated ventricles on CT and MRI
 | |
| Wolfram Syndrome (DIDMOAD) |
| |||
| Nephrogenic | Acquired | Drug-induced (demeclocycline, lithium) |
| |
| Hypercalcemia |
| |||
| Hypokalemia |
| |||
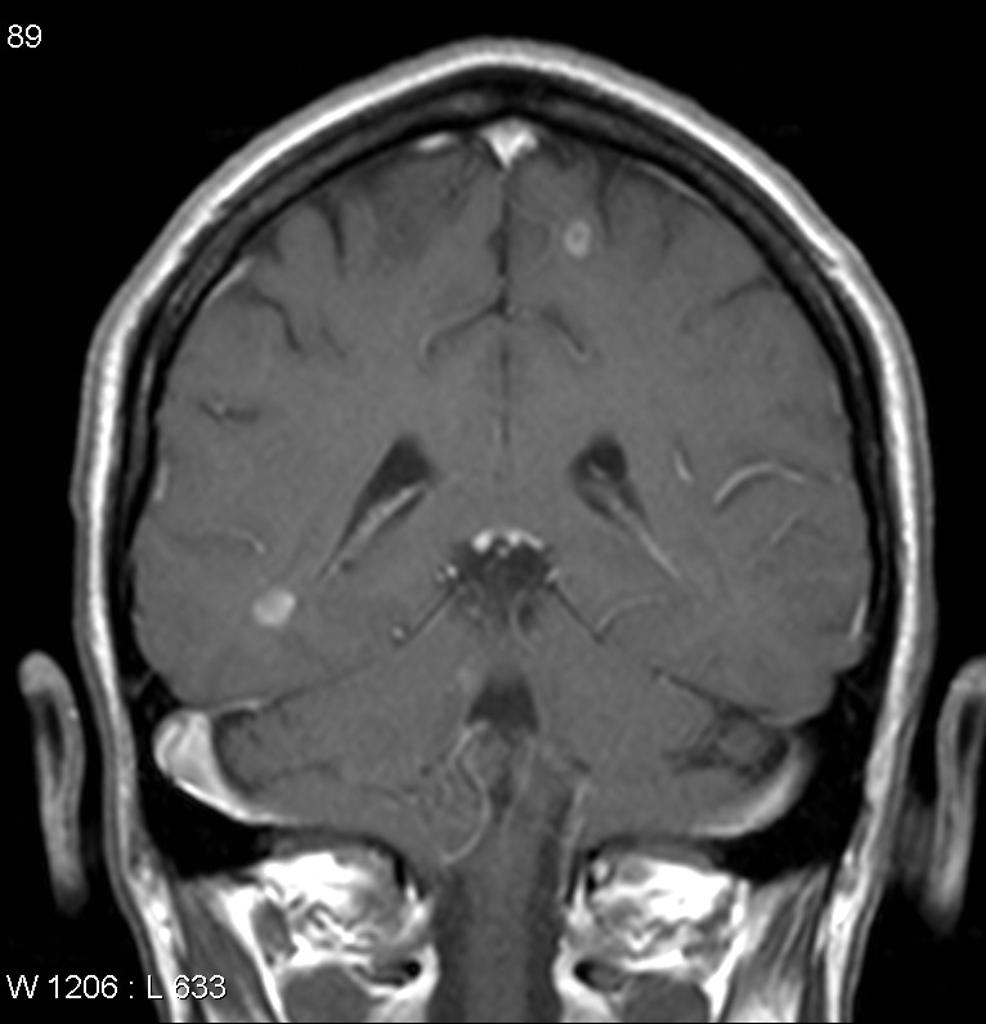
| Multiple myeloma |
|
 | ||
| Sickle cell disease |
|
 | ||
| Primary polydipsia | Psychogenic |
| ||
| Gestational diabetes insipidus |
| |||
| Diabetes mellitus |
| |||
References
- ↑ Willcutts MD, Felner E, White PC (1999). "Autosomal recessive familial neurohypophyseal diabetes insipidus with continued secretion of mutant weakly active vasopressin". Hum Mol Genet. 8 (7): 1303–7. PMID 10369876.
- ↑ Abu Libdeh A, Levy-Khademi F, Abdulhadi-Atwan M, Bosin E, Korner M, White PC; et al. (2010). "Autosomal recessive familial neurohypophyseal diabetes insipidus: onset in early infancy". Eur J Endocrinol. 162 (2): 221–6. doi:10.1530/EJE-09-0772. PMID 19897608.
- ↑ Barrett TG, Bundey SE (1997). "Wolfram (DIDMOAD) syndrome". J Med Genet. 34 (10): 838–41. PMC 1051091. PMID 9350817.
- ↑ Ghosh KN, Bhattacharya A (1992). "Gonotrophic nature of Phlebotomus argentipes (Diptera: Psychodidae) in the laboratory". Rev Inst Med Trop Sao Paulo. 34 (2): 181–2. PMID 1340034.