Cysticercosis differential diagnosis
|
Cysticercosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Cysticercosis differential diagnosis On the Web |
|
American Roentgen Ray Society Images of Cysticercosis differential diagnosis |
|
Risk calculators and risk factors for Cysticercosis differential diagnosis |
Overview
Cysticercosis must be differentiated from other diseases that cause brain cystic lesions (as brain abscess and brain tumors) or ocular lesions (as retinal detachment and coats disease).
Differentiating cysticercosis from other diseases
| Disease | Prominent clinical features | Lab findings | Radiological findings |
|---|---|---|---|
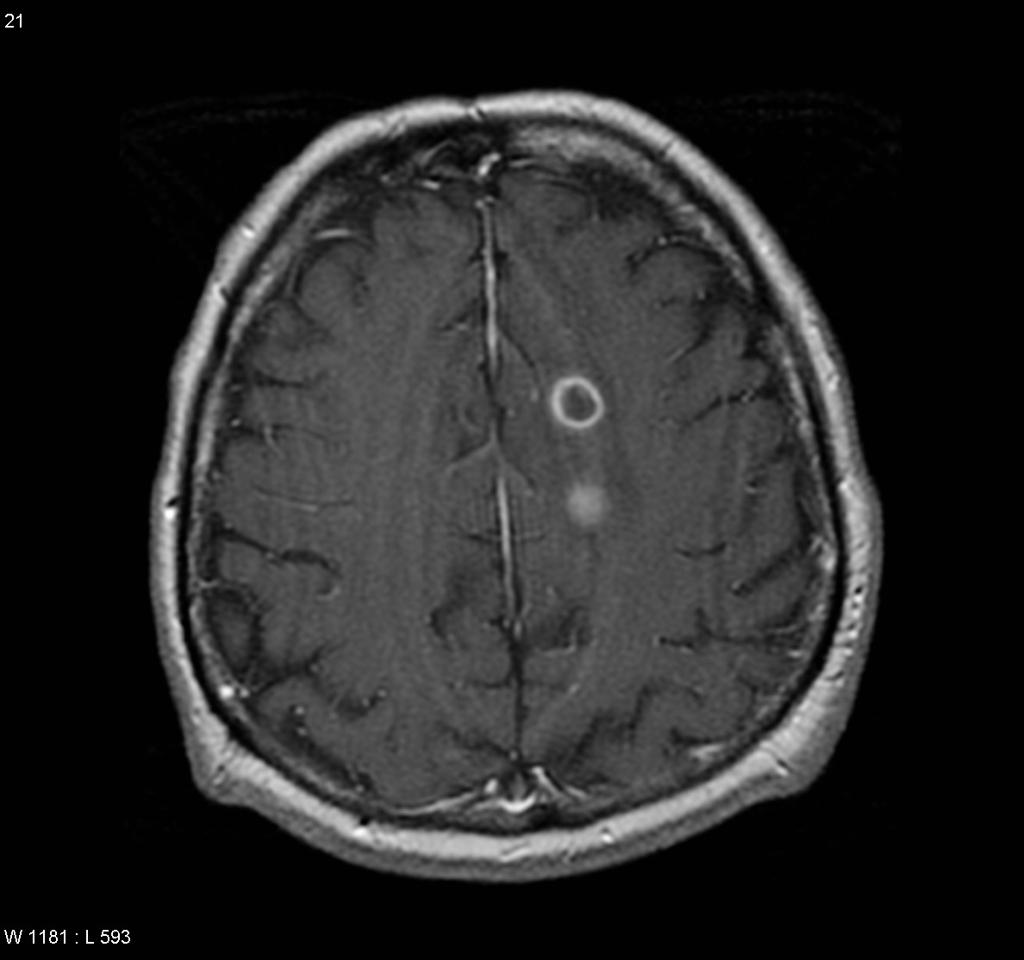
| Neurocysticercosis |
|
Lab findings are nonspecific. | |
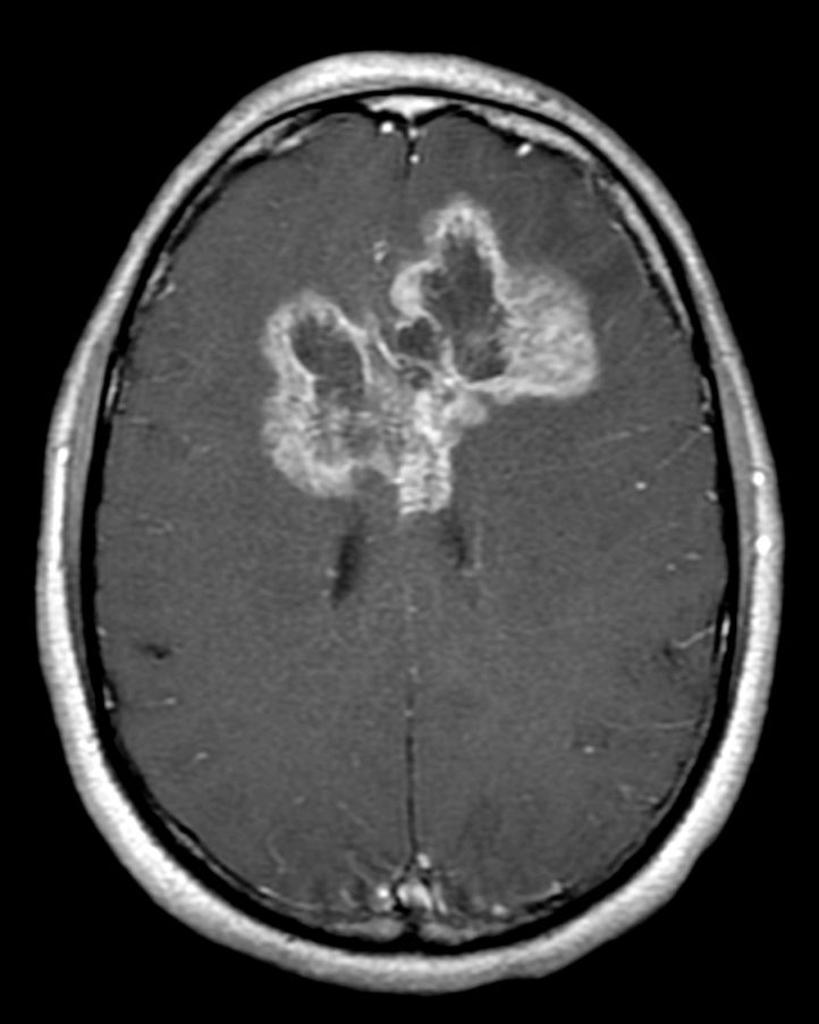
| Brain abscess |
|
|
|
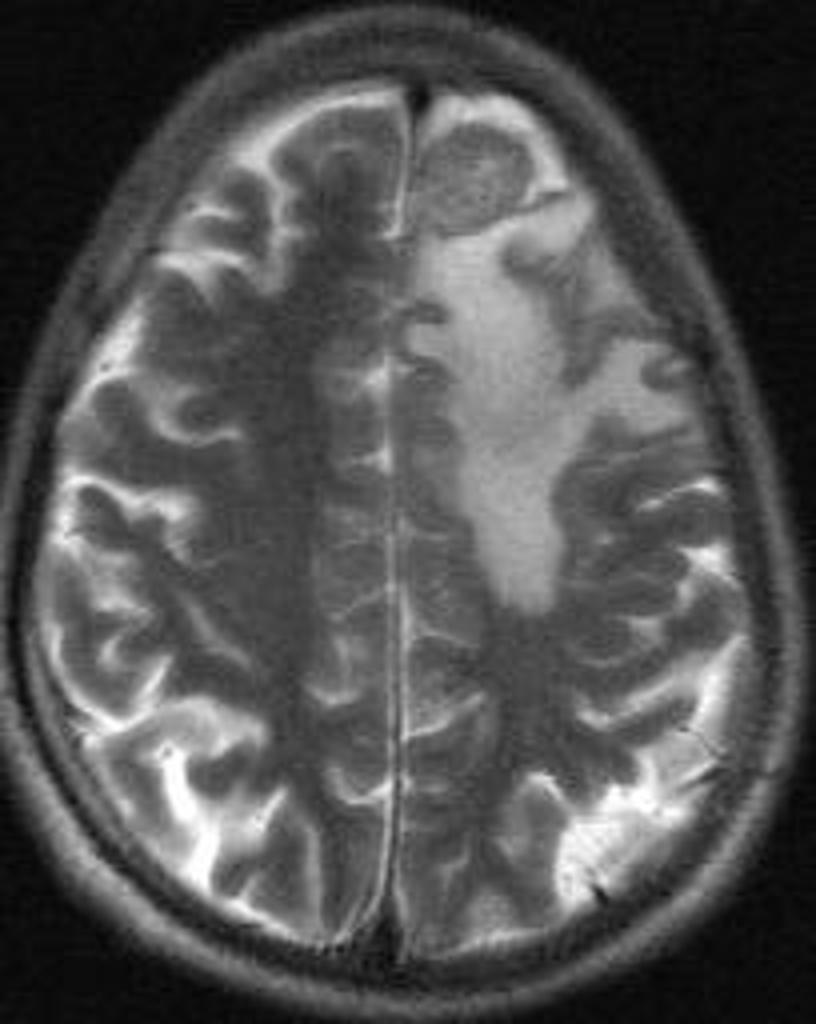
| Brain tumors |
|
| |
| Brain tuberculoma |
|
T.B. should be investigated everywhere else in the body (e.g. peripheral lymphadenopathy, sputum and blood culture) |
|
| Neurosarcoidosis | 70% of the patients present with the neurological symptoms rather than the presentation of systemic disease. Common presentations are:[5]
|
|
MRI with contrast shows enhancement of the inflamed areas (i.e. cranial nerves, meninges or HPO axis) |
 |
 |
 |
 |
|---|
| Disease | Prominent clinical feature | Radiological findings |
|---|---|---|
| Ocular cysticercosis | ||
| Coats disease |
|
|
| Retinal detachment |
|
|
| Thyroid Ophthalmopathy | The hallmark is Eye protrusion, photophobia, lacrimation and later in the disease, diminished eye motility.[8] |
|
| Retinoblastoma |
|
|
References
- ↑ Brouwer MC, Tunkel AR, McKhann GM, van de Beek D (2014). "Brain abscess". N. Engl. J. Med. 371 (5): 447–56. doi:10.1056/NEJMra1301635. PMID 25075836.
- ↑ "Brain Abscess — NEJM".
- ↑ 3.0 3.1 "Primary Brain Tumors in Adults - American Family Physician".
- ↑ "The Journal of Association of Chest Physicians - Tuberculoma of the brain - A diagnostic dilemma: Magnetic resonance spectroscopy a new ray of hope : Download PDF".
- ↑ 5.0 5.1 "Neurosarcoidosis".
- ↑ 6.0 6.1 "How to Diagnose and Manage Coats' Disease".
- ↑ 7.0 7.1 "Management of retinal detachment: a guide for non-ophthalmologists".
- ↑ 8.0 8.1 "Thyroid Ophthalmopathy - EyeWiki".
- ↑ 9.0 9.1 "c.ymcdn.com".