Cervical cancer pathophysiology: Difference between revisions
No edit summary |
m (Bot: Removing from Primary care) |
||
| (53 intermediate revisions by 3 users not shown) | |||
| Line 2: | Line 2: | ||
{{Cervical cancer}} | {{Cervical cancer}} | ||
{{CMG}} | {{CMG}}; {{AE}} {{Nnasiri}}, {{AIDA}} | ||
==Overview== | ==Overview== | ||
It is established that [[human papillomavirus]] ([[HPV]]) is the main cause of development of cervical neoplasia, only high risk strain of HPV can cause cervical cancer among women who are affected. This is because of [[HPV]] produced proteins E7 which alters [[epithelium]] of [[cervix]] mainly at junctional zone between the columnar [[epithelium]] of the [[endocervix]] and the [[squamous epithelium]] of the [[ectocervix]]. | |||
==Pathophysiology== | ==Pathophysiology== | ||
=== '''Pathogenesis | === '''Pathogenesis''' === | ||
High risk strains of [[HPV]], mainly [[HPV]] types 16 and 18 had been identified as a potent cause of cancer of cervix. [[HPV]] plays main role in [[pathogenesis]] of cervical cancer and it is widely related to disrupting [[cell cycle]] growth and regulations, summary of these include:<ref name="pmid12525422">{{cite journal |vauthors=Burd EM |title=Human papillomavirus and cervical cancer |journal=Clin. Microbiol. Rev. |volume=16 |issue=1 |pages=1–17 |date=January 2003 |pmid=12525422 |pmc=145302 |doi= |url=}}</ref> | |||
* | * The high risk [[HPV]] E6 and E7 [[gene]] products which are involved in [[viral replication]] and [[oncogenesis]] bind to [[p53]] and prevents its normal activities which is [[G1]] arrest, [[apoptosis]], and [[DNA repair]]. | ||
[[ | |||
* [[HPV]] enters the host cell which are [[Squamous epithelium|squamous cells of epithelium]] in [[cervix]], mainly in the junctional zone, between the [[columnar epithelium]] of the [[endocervix]] and the [[squamous epithelium]] of the [[ectocervix]] and that is how viral [[transcription]] and [[replication]] begins. | |||
* [[HPV]] infection of the basal layer of [[epithelium]] takes place by attachment via different mechanism of entry, this happens by cell surface [[heparan sulfate]], stabilizing [[proteoglycans]] and [[Integrin]]. | |||
There are other cofactors that cause progression of cervical neoplasia, some of these include:<ref name="pmid9602680">{{cite journal |vauthors=Arends MJ, Buckley CH, Wells M |title=Aetiology, pathogenesis, and pathology of cervical neoplasia |journal=J. Clin. Pathol. |volume=51 |issue=2 |pages=96–103 |date=February 1998 |pmid=9602680 |doi= |url=}}</ref><ref name="pmid6129466">{{cite journal |vauthors=zur Hausen H |title=Human genital cancer: synergism between two virus infections or synergism between a virus infection and initiating events? |journal=Lancet |volume=2 |issue=8312 |pages=1370–2 |date=December 1982 |pmid=6129466 |doi= |url=}}</ref><ref name="pmid18386537">{{cite journal |vauthors=Vanakankovit N, Taneepanichskul S |title=Effect of oral contraceptives on risk of cervical cancer |journal=J Med Assoc Thai |volume=91 |issue=1 |pages=7–12 |date=January 2008 |pmid=18386537 |doi= |url=}}</ref> | |||
* [[HLA]] type | |||
* [[Immunosuppression]], since response to [[HPV]] infection is cell mediated. | |||
* Use of [[oral contraceptives]] had been identified to play an important role in | |||
* Smoking which disrupts immune response. | |||
* History of promiscuous sexual activity in male partner | |||
* Early age sexual activities | |||
* Co-infection with [[herpes simplex virus type 2]], [[cytomegalovirus]] ([[CMV]]), [[human herpesvirus 6]] (HHV-6), and [[HHV-7]], which cause promotion of infection with [[HPV]] and plays an initiation role. | |||
== Genetic == | |||
* [[IL-1]]β, encoded by the [[IL-1|''IL''-''1B'']] gene, is an inflammatory [[cytokine]] and part of the innate [[immune system]].<ref>{{cite journal|doi=10.1016/S1674-8301(11)60020-1.}}</ref><ref name="ShiChen2013">{{cite journal|last1=Shi|first1=Ting-Yan|last2=Chen|first2=Xiao-Jun|last3=Zhu|first3=Mei-Ling|last4=Wang|first4=Meng-Yun|last5=He|first5=Jing|last6=Yu|first6=Ke-Da|last7=Shao|first7=Zhi-Ming|last8=Sun|first8=Meng-Hong|last9=Zhou|first9=Xiao-Yan|last10=Cheng|first10=Xi|last11=Wu|first11=Xiaohua|last12=Wei|first12=Qingyi|title=A pri-miR-218variant and risk of cervical carcinoma in Chinese women|journal=BMC Cancer|volume=13|issue=1|year=2013|issn=1471-2407|doi=10.1186/1471-2407-13-19}}</ref> | |||
* [[TNF-α]], encoded by the ''[[TNFAIP1|TNFA]]'' gene, is another potent pro-inflammatory [[cytokine]] that has been implicated in the control of HPV infection. | |||
* [[Polymorphisms]] within ''[[HLA]] plays a role in [[pathogenesis]] of cervical [[neoplasia]].'' | |||
* [[Interleukin-12]] A and B gene (''IL12A'' and '''''IL12B''''') | |||
* [[IFN|IFN-γ]], encoded by the ''[[IFNG]]'' gene has defensive role against [[Viruses|viruse]]<nowiki/>s and induces immune mediated [[inflammatory responses]]. | |||
* [[Interleukin-10]]: the risk and the progression of cervical cancer have been associated with increased [[IL-10]] serum levels. | |||
* [[Cytotoxic T-lymphocytes|Cytotoxic T-lymphocyte]] antigen-4 | |||
* [[HPV]] E6/E7 [[oncogenes]], proteins that interfere with [[cell cycle]] growth and [[Tumor supressor gene|tumor supressor genes]]. | |||
* Primary [[microRNA]]-218 (''pri''-''miR''-''218'') and [[laminin]]-5 β3 (''LAMB3''). | |||
== Associated Conditions: == | |||
Conditions associated with cervical cancer include:<ref name="OginoOkamoto2003">{{cite journal|last1=Ogino|first1=Ichiro|last2=Okamoto|first2=Naoyuki|last3=Ono|first3=Yoshimi|last4=Kitamura|first4=Tatsuo|last5=Nakayama|first5=Hiroki|title=Pelvic insufficiency fractures in postmenopausal woman with advanced cervical cancer treated by radiotherapy|journal=Radiotherapy and Oncology|volume=68|issue=1|year=2003|pages=61–67|issn=01678140|doi=10.1016/S0167-8140(03)00128-2}}</ref> | |||
* Enterovaginal, [[Rectovaginal fistula|rectovaginal]], and vesico- or ureterovaginal fistulas | |||
* [[Renal failure]] and/or [[uremia]] | |||
* [[Stress incontinence]] | |||
* [[Loss of libido]] | |||
* [[Vaginal atrophy]] and dryness | |||
* Early [[menopause]] | |||
* [[Malnutrition]] | |||
* [[Osteoprosis]] | |||
* [[Anemia]] | |||
* [[depression]] | |||
* | |||
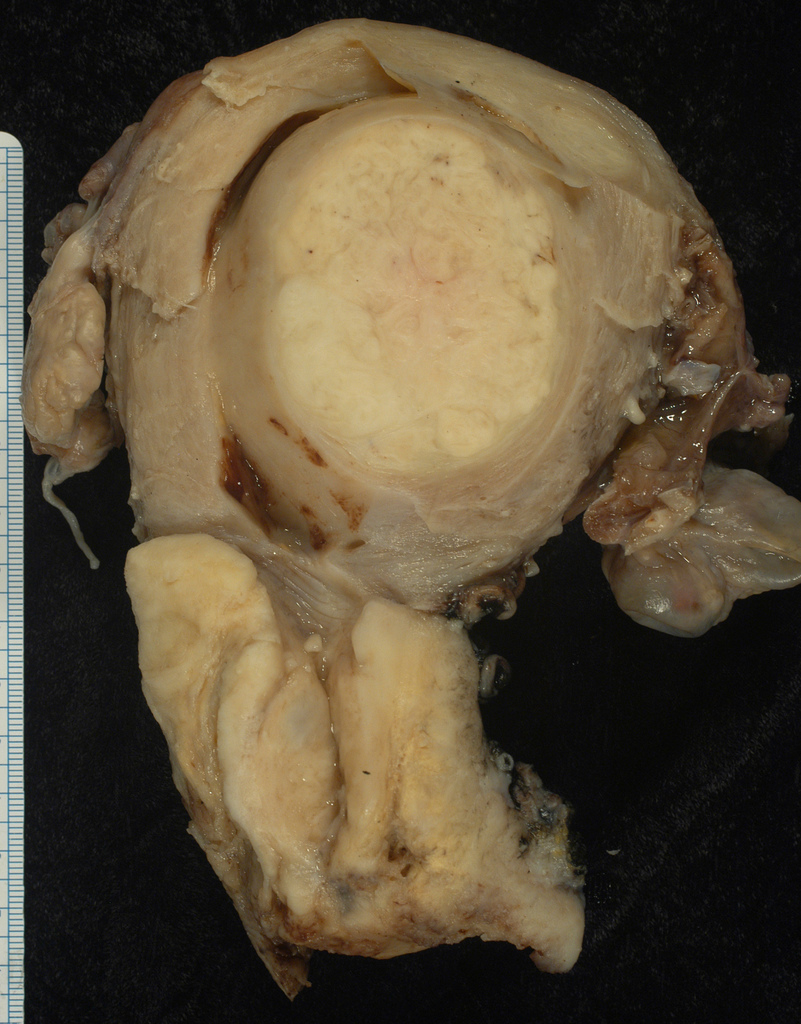
== Gross Pathology: == | |||
Gross pathological changes can be visualized by [[colposcopy]] and [[biopsy]] and application of a 3% acetic acid solution on [[biopsy]] speciemen and inspection under bright filtered [[light microscopy]] with 10 to 15 fold magnification. Findings in [[gross pathology]] of patients with cervical cancer include:<ref name="Burd2003">{{cite journal|last1=Burd|first1=E. M.|title=Human Papillomavirus and Cervical Cancer|journal=Clinical Microbiology Reviews|volume=16|issue=1|year=2003|pages=1–17|issn=0893-8512|doi=10.1128/CMR.16.1.1-17.2003}}</ref> | |||
* Acetowhitening | |||
* Characteristic vascular pattern of [[dysplasia]] or [[carcinoma]] | |||
[[File:Squamous carcinoma of the cervix.jpg|400px|thumb|left|squamous cell carcinoma of the cervix[https://librepathology.org/wiki/File:Squamous_carcinoma_of_the_cervix.jpg source:Ed Uthman, MD https://www.flickr.com/photos/euthman/119271511/in/set-72057594114099781/]]]<br style="clear:left" /> | |||
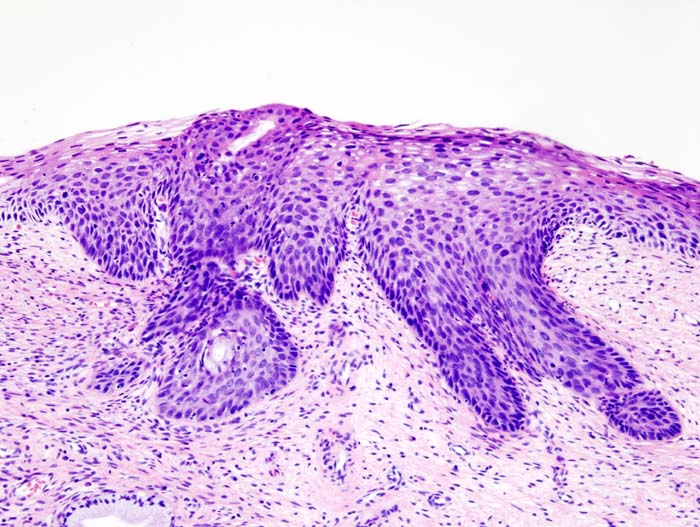
==Microscopic pathology== | |||
[[Microscopic]] morphology of '''low‐grade squamous intraepithelial lesions ([[CIN|CIN 1]])''' include:<ref name="KalofCooper2006">{{cite journal|last1=Kalof|first1=A. N|last2=Cooper|first2=K.|title=Our approach to squamous intraepithelial lesions of the uterine cervix|journal=Journal of Clinical Pathology|volume=60|issue=5|year=2006|pages=449–455|issn=0021-9746|doi=10.1136/jcp.2005.036426}}</ref> | |||
* Presence of [[koilocytosis]] ([[Perinuclear space|perinuclear]] [[cytoplasmic]] clearing with peripheral condensation of the [[cytoplasm]]) | |||
* Irregular nuclear contours, either binucleation or/and multinucleation | |||
* Hyperchromasia and/or cellular [[pleomorphism]] | |||
* Mild [[dysplasia]] | |||
[[File:LSIL (CIN 1), Cervical Biopsy (3776284166).jpg|400px|thumb|left|CIN1 morphology [https://commons.wikimedia.org/wiki/File:LSIL_(CIN_1),_Cervical_Biopsy_(3776284166).jpg#file source:Ed Uthman, Author,LSIL (CIN 1), Cervical Biopsy]]]<br style="clear:left" /> | |||
'''High‐grade dysplasia (CIN 2 and 3)''' is characterized by the following features: | |||
* Loss of maturation | |||
* Nuclear crowding | |||
* Loss of nuclear polarity | |||
* Prominent cytonuclear [[atypia]], increase in nuclear‐to‐cytoplasmic ratios | |||
* Irregular nuclear contours and coarse chromatin. | |||
* Increased proliferation and [[mitotic]] changes in the upper part of the epithelium. | |||
* In [[CIN|CIN2]], most cytonuclear abnormalities are seen in the lower and middle third of the [[epithelium]]. | |||
* [[CIN]]3 characteristic features include: | |||
** Full‐thickness cytonuclear [[atypia]] | |||
** Minimal to absent maturation | |||
** Numerous [[mitotic]] activities | |||
[[File:202px-CIN2.jpg|400px|thumb|left|showing CIN2[https://commons.wikimedia.org/wiki/File:Cervical_intraepithelial_neoplasia_(3)_CIN2.jpgNo machine-readable source provided. Own work assumed (based on copyright claims).]]] | |||
[[File:Cervical intraepithelial neoplasia CIN3.jpg|400px|thumb|left|CIN3 [https://upload.wikimedia.org/wikipedia/commons/f/fd/Cervical_intraepithelial_neoplasia_%285%29_CIN3.jpgNo machine-readable source provided. Own work assumed (based on copyright claims).]]]<br style="clear:left" /> | |||
===Video=== | ===Video=== | ||
{{#ev:youtube|J3kULzKGzws}} | {{#ev:youtube|J3kULzKGzws}} | ||
| Line 43: | Line 94: | ||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
{{WH}} | |||
{{WS}} | |||
[[Category:Disease]] | [[Category:Disease]] | ||
[[Category:Gynecology]] | [[Category:Gynecology]] | ||
[[Category:Types of cancer]] | [[Category:Types of cancer]] | ||
[[Category:Up-To-Date]] | |||
[[Category:Oncology]] | [[Category:Oncology]] | ||
[[Category:Medicine]] | [[Category:Medicine]] | ||
Latest revision as of 20:51, 29 July 2020
|
Cervical cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Cervical cancer pathophysiology On the Web |
|
American Roentgen Ray Society Images of Cervical cancer pathophysiology |
|
Risk calculators and risk factors for Cervical cancer pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Nima Nasiri, M.D.[2], Aida Javanbakht, M.D.
Overview
It is established that human papillomavirus (HPV) is the main cause of development of cervical neoplasia, only high risk strain of HPV can cause cervical cancer among women who are affected. This is because of HPV produced proteins E7 which alters epithelium of cervix mainly at junctional zone between the columnar epithelium of the endocervix and the squamous epithelium of the ectocervix.
Pathophysiology
Pathogenesis
High risk strains of HPV, mainly HPV types 16 and 18 had been identified as a potent cause of cancer of cervix. HPV plays main role in pathogenesis of cervical cancer and it is widely related to disrupting cell cycle growth and regulations, summary of these include:[1]
- The high risk HPV E6 and E7 gene products which are involved in viral replication and oncogenesis bind to p53 and prevents its normal activities which is G1 arrest, apoptosis, and DNA repair.
- HPV enters the host cell which are squamous cells of epithelium in cervix, mainly in the junctional zone, between the columnar epithelium of the endocervix and the squamous epithelium of the ectocervix and that is how viral transcription and replication begins.
- HPV infection of the basal layer of epithelium takes place by attachment via different mechanism of entry, this happens by cell surface heparan sulfate, stabilizing proteoglycans and Integrin.
There are other cofactors that cause progression of cervical neoplasia, some of these include:[2][3][4]
- HLA type
- Immunosuppression, since response to HPV infection is cell mediated.
- Use of oral contraceptives had been identified to play an important role in
- Smoking which disrupts immune response.
- History of promiscuous sexual activity in male partner
- Early age sexual activities
- Co-infection with herpes simplex virus type 2, cytomegalovirus (CMV), human herpesvirus 6 (HHV-6), and HHV-7, which cause promotion of infection with HPV and plays an initiation role.
Genetic
- IL-1β, encoded by the IL-1B gene, is an inflammatory cytokine and part of the innate immune system.[5][6]
- TNF-α, encoded by the TNFA gene, is another potent pro-inflammatory cytokine that has been implicated in the control of HPV infection.
- Polymorphisms within HLA plays a role in pathogenesis of cervical neoplasia.
- Interleukin-12 A and B gene (IL12A and IL12B)
- IFN-γ, encoded by the IFNG gene has defensive role against viruses and induces immune mediated inflammatory responses.
- Interleukin-10: the risk and the progression of cervical cancer have been associated with increased IL-10 serum levels.
- Cytotoxic T-lymphocyte antigen-4
- HPV E6/E7 oncogenes, proteins that interfere with cell cycle growth and tumor supressor genes.
- Primary microRNA-218 (pri-miR-218) and laminin-5 β3 (LAMB3).
Associated Conditions:
Conditions associated with cervical cancer include:[7]
- Enterovaginal, rectovaginal, and vesico- or ureterovaginal fistulas
- Renal failure and/or uremia
- Stress incontinence
- Loss of libido
- Vaginal atrophy and dryness
- Early menopause
- Malnutrition
- Osteoprosis
- Anemia
- depression
Gross Pathology:
Gross pathological changes can be visualized by colposcopy and biopsy and application of a 3% acetic acid solution on biopsy speciemen and inspection under bright filtered light microscopy with 10 to 15 fold magnification. Findings in gross pathology of patients with cervical cancer include:[8]
Microscopic pathology
Microscopic morphology of low‐grade squamous intraepithelial lesions (CIN 1) include:[9]
- Presence of koilocytosis (perinuclear cytoplasmic clearing with peripheral condensation of the cytoplasm)
- Irregular nuclear contours, either binucleation or/and multinucleation
- Hyperchromasia and/or cellular pleomorphism
- Mild dysplasia

High‐grade dysplasia (CIN 2 and 3) is characterized by the following features:
- Loss of maturation
- Nuclear crowding
- Loss of nuclear polarity
- Prominent cytonuclear atypia, increase in nuclear‐to‐cytoplasmic ratios
- Irregular nuclear contours and coarse chromatin.
- Increased proliferation and mitotic changes in the upper part of the epithelium.
- In CIN2, most cytonuclear abnormalities are seen in the lower and middle third of the epithelium.
- CIN3 characteristic features include:

Video
{{#ev:youtube|J3kULzKGzws}}
References
- ↑ Burd EM (January 2003). "Human papillomavirus and cervical cancer". Clin. Microbiol. Rev. 16 (1): 1–17. PMC 145302. PMID 12525422.
- ↑ Arends MJ, Buckley CH, Wells M (February 1998). "Aetiology, pathogenesis, and pathology of cervical neoplasia". J. Clin. Pathol. 51 (2): 96–103. PMID 9602680.
- ↑ zur Hausen H (December 1982). "Human genital cancer: synergism between two virus infections or synergism between a virus infection and initiating events?". Lancet. 2 (8312): 1370–2. PMID 6129466.
- ↑ Vanakankovit N, Taneepanichskul S (January 2008). "Effect of oral contraceptives on risk of cervical cancer". J Med Assoc Thai. 91 (1): 7–12. PMID 18386537.
- ↑ . doi:10.1016/S1674-8301(11)60020-1. Check
|doi=value (help). Missing or empty|title=(help) - ↑ Shi, Ting-Yan; Chen, Xiao-Jun; Zhu, Mei-Ling; Wang, Meng-Yun; He, Jing; Yu, Ke-Da; Shao, Zhi-Ming; Sun, Meng-Hong; Zhou, Xiao-Yan; Cheng, Xi; Wu, Xiaohua; Wei, Qingyi (2013). "A pri-miR-218variant and risk of cervical carcinoma in Chinese women". BMC Cancer. 13 (1). doi:10.1186/1471-2407-13-19. ISSN 1471-2407.
- ↑ Ogino, Ichiro; Okamoto, Naoyuki; Ono, Yoshimi; Kitamura, Tatsuo; Nakayama, Hiroki (2003). "Pelvic insufficiency fractures in postmenopausal woman with advanced cervical cancer treated by radiotherapy". Radiotherapy and Oncology. 68 (1): 61–67. doi:10.1016/S0167-8140(03)00128-2. ISSN 0167-8140.
- ↑ Burd, E. M. (2003). "Human Papillomavirus and Cervical Cancer". Clinical Microbiology Reviews. 16 (1): 1–17. doi:10.1128/CMR.16.1.1-17.2003. ISSN 0893-8512.
- ↑ Kalof, A. N; Cooper, K. (2006). "Our approach to squamous intraepithelial lesions of the uterine cervix". Journal of Clinical Pathology. 60 (5): 449–455. doi:10.1136/jcp.2005.036426. ISSN 0021-9746.