Carotid body tumor pathophysiology: Difference between revisions
No edit summary |
m (Bot: Removing from Primary care) |
||
| (26 intermediate revisions by one other user not shown) | |||
| Line 2: | Line 2: | ||
{{Carotid body tumor}} | {{Carotid body tumor}} | ||
{{CMG}}; {{AE}} {{Sahar}} | {{CMG}}; {{AE}} {{Sahar}} {{MV}} | ||
==Overview== | ==Overview== | ||
The [[carotid body]] is an ellipsoid-like structure located in the [[adventitia]] or periadventitial [[tissue]] of the [[bifurcation]] of the [[common carotid artery]]. This organ is a [[Chemoreceptor|chemo-receptor]] and its function is the monitoring of [[arterial]] [[Blood oxygen level|blood oxygen]] and carbon dioxide levels. The exact pathogenesis of [[carotid body]] [[tumor]] is not fully understood. however, the overgrowth of [[chemoreceptor]] [[paraganglioma]] [[cells]] in the [[carotid body]] leads to the formation of [[carotid body]] [[tumor]]. Recent litreture has suggested the role of several [[Germline mutation|germline mutations]] in the [[pathogenesis]] of this [[tumor]]. Also, the [[hyperplastic]] form of the [[tumor]] has been associated with conditions that causes [[chronic]] [[hypoxia]]. | |||
==Pathophysiology== | ==Pathophysiology== | ||
===Anatomy=== | |||
*The [[carotid body]] is an ellipsoid-like structure located in the [[adventitia]] or periadventitial [[tissue]] of the [[bifurcation]] of the [[common carotid artery]].<ref name="BurgessCalderon2017">{{cite journal|last1=Burgess|first1=Alfred|last2=Calderon|first2=Moises|last3=Jafif-Cojab|first3=Marcos|last4=Jorge|first4=Diego|last5=Balanza|first5=Ricardo|title=Bilateral carotid body tumor resection in a female patient|journal=International Journal of Surgery Case Reports|volume=41|year=2017|pages=387–391|issn=22102612|doi=10.1016/j.ijscr.2017.11.019}}</ref> | |||
*The normal [[carotid body]] weighs less than 15 mg and measures between 3 to 5 mm. | |||
*This structure [[innervated]] by the hearing branch of the [[glossopharyngeal nerve]], however, the [[carotid body]] is in close proximity of a majority of important [[nerves]]. | |||
*The [[blood]] supply to the [[carotid body]] is provided by [[ascending pharyngeal artery]], which is the branch of the [[external carotid artery]]. | |||
===Physiology=== | ===Physiology=== | ||
The | *The [[carotid body]] is a [[Chemoreceptor|chemo-receptor]] and its function is the monitoring of [[arterial]] [[Blood oxygen level|blood oxygen]] and carbon dioxide levels.<ref>{{cite book | last = Robertson | first = David | title = Primer on the autonomic nervous system | publisher = Elsevier | location = London | year = 2012 | isbn = 978-0-12-386525-0 }}</ref><ref>{{cite book | last = Zufall | first = Frank | title = Chemosensory transduction : the detection of odors, tastes, and other chemostimuli | publisher = Academic Press is an imprint of Elsevier | location = London, UK | year = 2016 | isbn = 978-0-12-801694-7 }}</ref> | ||
*This [[Organ (anatomy)|organ]] is sensitive to the reduction of oxygen [[partial pressure]] in the [[blood]] which results in reflexive activation of the [[autonomic nervous system]] and the resultant increase in the | |||
ventilation rate. | |||
===Pathogenesis=== | ===Pathogenesis=== | ||
*Carotid body tumor is a neuroendocrine neoplasm originating from carotid body.<ref name="pmid15883711">{{cite journal |vauthors=Boedeker CC, Ridder GJ, Schipper J |title=Paragangliomas of the head and neck: diagnosis and treatment |journal=Fam. Cancer |volume=4 |issue=1 |pages=55–9 |date=2005 |pmid=15883711 |doi=10.1007/s10689-004-2154-z |url=}}</ref> | *[[Carotid body]] [[tumor]] is a [[neuroendocrine]] [[neoplasm]] originating from [[carotid body]].<ref name="pmid15883711">{{cite journal |vauthors=Boedeker CC, Ridder GJ, Schipper J |title=Paragangliomas of the head and neck: diagnosis and treatment |journal=Fam. Cancer |volume=4 |issue=1 |pages=55–9 |date=2005 |pmid=15883711 |doi=10.1007/s10689-004-2154-z |url=}}</ref> | ||
**Carotid body is a component of the autonomic system derived from neural crest cells of the third | **[[Carotid body]] is a component of the [[autonomic nervous system]] derived from [[neural crest cells]] of the [[embryonic]] third [[branchial arch]].<ref name="BurgessCalderon2017">{{cite journal|last1=Burgess|first1=Alfred|last2=Calderon|first2=Moises|last3=Jafif-Cojab|first3=Marcos|last4=Jorge|first4=Diego|last5=Balanza|first5=Ricardo|title=Bilateral carotid body tumor resection in a female patient|journal=International Journal of Surgery Case Reports|volume=41|year=2017|pages=387–391|issn=22102612|doi=10.1016/j.ijscr.2017.11.019}}</ref> | ||
*The overgrowth of chemoreceptor paraganglioma cells in the carotid body leads to the formation of carotid body tumor. | *The overgrowth of [[chemoreceptor]] [[paraganglioma]] [[cells]] in the [[carotid body]] leads to the formation of [[carotid body]] [[tumor]]. | ||
*Carotid body tumors are normally located in the medial aspect adventitia of the carotid bifurcation. | *[[Carotid body]] [[tumors]] are normally located in the [[medial]] aspect [[adventitia]] of the [[carotid]] [[bifurcation]]. | ||
*Carotid body tumor occurs sporadicly in 85% to 90% of the cases.<ref name="BurgessCalderon2017">{{cite journal|last1=Burgess|first1=Alfred|last2=Calderon|first2=Moises|last3=Jafif-Cojab|first3=Marcos|last4=Jorge|first4=Diego|last5=Balanza|first5=Ricardo|title=Bilateral carotid body tumor resection in a female patient|journal=International Journal of Surgery Case Reports|volume=41|year=2017|pages=387–391|issn=22102612|doi=10.1016/j.ijscr.2017.11.019}}</ref><ref name="RidgeBrewster1993">{{cite journal|last1=Ridge|first1=Brian A.|last2=Brewster|first2=David C.|last3=Darling|first3=R. Clement|last4=Cambria|first4=Richard P.|last5=LaMuraglia|first5=Glenn M.|last6=Abbott|first6=William M.|title=Familial Carotid Body Tumors: Incidence and Implications|journal=Annals of Vascular Surgery|volume=7|issue=2|year=1993|pages=190–194|issn=08905096|doi=10.1007/BF02001015}}</ref> | *[[Carotid body]] [[tumor]] occurs sporadicly in 85% to 90% of the cases.<ref name="BurgessCalderon2017">{{cite journal|last1=Burgess|first1=Alfred|last2=Calderon|first2=Moises|last3=Jafif-Cojab|first3=Marcos|last4=Jorge|first4=Diego|last5=Balanza|first5=Ricardo|title=Bilateral carotid body tumor resection in a female patient|journal=International Journal of Surgery Case Reports|volume=41|year=2017|pages=387–391|issn=22102612|doi=10.1016/j.ijscr.2017.11.019}}</ref><ref name="RidgeBrewster1993">{{cite journal|last1=Ridge|first1=Brian A.|last2=Brewster|first2=David C.|last3=Darling|first3=R. Clement|last4=Cambria|first4=Richard P.|last5=LaMuraglia|first5=Glenn M.|last6=Abbott|first6=William M.|title=Familial Carotid Body Tumors: Incidence and Implications|journal=Annals of Vascular Surgery|volume=7|issue=2|year=1993|pages=190–194|issn=08905096|doi=10.1007/BF02001015}}</ref> | ||
* | *Recent litreture has suggested the role of several [[Germline mutation|germline mutations]] in the [[pathogenesis]] of this [[tumor]].<ref name="WienekeSmith2009">{{cite journal|last1=Wieneke|first1=Jacqueline A.|last2=Smith|first2=Alice|title=Paraganglioma: Carotid Body Tumor|journal=Head and Neck Pathology|volume=3|issue=4|year=2009|pages=303–306|issn=1936-055X|doi=10.1007/s12105-009-0130-5}}</ref> | ||
*It has been explained that the [[hyperplastic]] form of the [[tumor]] is associated with [[chronic]] [[hypoxia]] due to such as:<ref name="BurgessCalderon2017">{{cite journal|last1=Burgess|first1=Alfred|last2=Calderon|first2=Moises|last3=Jafif-Cojab|first3=Marcos|last4=Jorge|first4=Diego|last5=Balanza|first5=Ricardo|title=Bilateral carotid body tumor resection in a female patient|journal=International Journal of Surgery Case Reports|volume=41|year=2017|pages=387–391|issn=22102612|doi=10.1016/j.ijscr.2017.11.019}}</ref><ref name="SajidHamilton2007">{{cite journal|last1=Sajid|first1=M.S.|last2=Hamilton|first2=G.|last3=Baker|first3=D.M.|title=A Multicenter Review of Carotid Body Tumour Management|journal=European Journal of Vascular and Endovascular Surgery|volume=34|issue=2|year=2007|pages=127–130|issn=10785884|doi=10.1016/j.ejvs.2007.01.015}}</ref> | |||
**[[Chronic obstructive pulmonary disease]] | |||
*It has been explained that the hyperplastic form of the tumor is associated with chronic hypoxia due to such as:<ref name="BurgessCalderon2017">{{cite journal|last1=Burgess|first1=Alfred|last2=Calderon|first2=Moises|last3=Jafif-Cojab|first3=Marcos|last4=Jorge|first4=Diego|last5=Balanza|first5=Ricardo|title=Bilateral carotid body tumor resection in a female patient|journal=International Journal of Surgery Case Reports|volume=41|year=2017|pages=387–391|issn=22102612|doi=10.1016/j.ijscr.2017.11.019}}</ref><ref name="SajidHamilton2007">{{cite journal|last1=Sajid|first1=M.S.|last2=Hamilton|first2=G.|last3=Baker|first3=D.M.|title=A Multicenter Review of Carotid Body Tumour Management|journal=European Journal of Vascular and Endovascular Surgery|volume=34|issue=2|year=2007|pages=127–130|issn=10785884|doi=10.1016/j.ejvs.2007.01.015}}</ref> | **[[Cyanotic heart disease]] | ||
**Chronic obstructive pulmonary disease | *The [[tumor]] may be [[bilateral]] in fewer than 5% of the sporadic cases. | ||
**Cyanotic heart disease | *The [[tumor]] may be [[familial]] in the rest 10% to 15%. | ||
**In [[familial]] cases, it may be [[bilateral]] in 30% to 40% of the cases. | |||
==Genetics== | ==Genetics== | ||
*The | *The [[familial]] form of the [[tumor]] is associated with a [[mutation]] in a [[gene]] located on 11q23.<ref name="FennessyKozakewich2009">{{cite journal|last1=Fennessy|first1=B. G.|last2=Kozakewich|first2=H. P. W.|last3=Silvera|first3=M.|last4=Frerichs|first4=K.|last5=Lillhei|first5=C. W.|last6=Poe|first6=D.|last7=Rahbar|first7=R.|title=The presentation and management of multiple paraganglioma in head and neck|journal=Irish Journal of Medical Science|volume=180|issue=3|year=2009|pages=757–760|issn=0021-1265|doi=10.1007/s11845-009-0338-0}}</ref> | ||
*The [[disease]] inheritance is through [[Autosomal dominant|autosomal dominance]].<ref name="pmid12213855">{{cite journal |vauthors=Young AL, Baysal BE, Deb A, Young WF |title=Familial malignant catecholamine-secreting paraganglioma with prolonged survival associated with mutation in the succinate dehydrogenase B gene |journal=J. Clin. Endocrinol. Metab. |volume=87 |issue=9 |pages=4101–5 |date=September 2002 |pmid=12213855 |doi=10.1210/jc.2002-020312 |url=}}</ref> | |||
*The following [[genes]] has been linked to an increased [[incidence]] of [[paraganglioma]] including [[carotid body]] [[tumor]]:<ref name="DavilaChang2016">{{cite journal|last1=Davila|first1=Victor J.|last2=Chang|first2=James M.|last3=Stone|first3=William M.|last4=Fowl|first4=Richard J.|last5=Bower|first5=Thomas C.|last6=Hinni|first6=Michael L.|last7=Money|first7=Samuel R.|title=Current surgical management of carotid body tumors|journal=Journal of Vascular Surgery|volume=64|issue=6|year=2016|pages=1703–1710|issn=07415214|doi=10.1016/j.jvs.2016.05.076}}</ref><ref name="WienekeSmith2009">{{cite journal|last1=Wieneke|first1=Jacqueline A.|last2=Smith|first2=Alice|title=Paraganglioma: Carotid Body Tumor|journal=Head and Neck Pathology|volume=3|issue=4|year=2009|pages=303–306|issn=1936-055X|doi=10.1007/s12105-009-0130-5}}</ref> | |||
**[[Succinate dehydrogenase]] ([[SDH]]) complex [[SDHB|subunits B]], [[SDHC|C]], and [[SDHD|D]]. | |||
**[[RET gene|RET]] | |||
**[[Von Hippel-Lindau tumor suppressor|Von Hippel-Lindau]] ([[VHL]]) | |||
**[[Neurofibromatosis type I]] ([[NF1]]) | |||
==Associated Conditions== | ==Associated Conditions== | ||
Conditions associated with [disease name] | [[Conditions]] associated with [[carotid body]] [[tumor]] include:<ref name="WienekeSmith2009">{{cite journal|last1=Wieneke|first1=Jacqueline A.|last2=Smith|first2=Alice|title=Paraganglioma: Carotid Body Tumor|journal=Head and Neck Pathology|volume=3|issue=4|year=2009|pages=303–306|issn=1936-055X|doi=10.1007/s12105-009-0130-5}}</ref> | ||
*[[Von Hippel-Lindau syndrome]] | |||
*[[Neurofibromatosis type I]] ([[von Recklinghausen disease]]) | |||
*[[MEN 2a|MEN 2A]] | |||
*[[MEN 2B]] | |||
*Carney's triad which consists of:<ref name="pmid865533">{{cite journal |vauthors=Carney JA, Sheps SG, Go VL, Gordon H |title=The triad of gastric leiomyosarcoma, functioning extra-adrenal paraganglioma and pulmonary chondroma |journal=N. Engl. J. Med. |volume=296 |issue=26 |pages=1517–8 |date=June 1977 |pmid=865533 |doi=10.1056/NEJM197706302962609 |url=}}</ref> | |||
**[[Gastric]] [[leiomyosarcoma]] | |||
**[[Pulmonary]] [[chondroma]] | |||
**Extraadrenal [[paraganglioma]] | |||
==Gross Pathology== | ==Gross Pathology== | ||
|Characteristic findings of [[carotid body]] [[tumor]], include:<ref name="WienekeSmith2009">{{cite journal|last1=Wieneke|first1=Jacqueline A.|last2=Smith|first2=Alice|title=Paraganglioma: Carotid Body Tumor|journal=Head and Neck Pathology|volume=3|issue=4|year=2009|pages=303–306|issn=1936-055X|doi=10.1007/s12105-009-0130-5}}</ref> | |||
**Well-circumscribed with psudocapsule | **Well-circumscribed with psudocapsule | ||
**The size of the tumor | **The size of the [[tumor]] varies greatly and it may be as large as 10 cm | ||
**The cutting surface is solid with a smooth, rubbery texture | **The cutting surface is solid with a smooth, rubbery texture | ||
{| | |||
|[[File:Carotid body tumor.jpg|thumb|400px|Contributed by Paweł Kuźniar in wikimedia.commons]] | |||
<br style="clear:left" /> | |||
|- | |||
|} | |||
==Microscopic Pathology== | ==Microscopic Pathology== | ||
*On microscopic histopathological analysis, carotid body tumor composed of: | *On [[microscopic]] [[histopathological]] analysis, [[carotid body]] [[tumor]] composed of: | ||
**The chief or paraganglionic cells composing the predominant part of the tumor and contain eosinophilic | **The chief or [[paraganglionic]] cells composing the predominant part of the [[tumor]] and contain [[eosinophilic]] granular materials and oval or round nuclei.<ref name="PatetsiosGable2002">{{cite journal|last1=Patetsios|first1=Peter|last2=Gable|first2=Dennis R.|last3=Garrett|first3=Wilson V.|last4=Lamont|first4=Jeffrey P.|last5=Kuhn|first5=Joseph A.|last6=Shutze|first6=William P.|last7=Kourlis|first7=Harry|last8=Grimsley|first8=Bradley|last9=Pearl|first9=Gregory J.|last10=Smith|first10=Bertram L.|last11=Talkington|first11=C.M.|last12=Thompson|first12=Jesse E.|title=Management of Carotid Body Paragangliomas and Review of a 30-year Experience|journal=Annals of Vascular Surgery|volume=16|issue=3|year=2002|pages=331–338|issn=08905096|doi=10.1007/s10016-001-0106-8}}</ref> | ||
**The supporting or sustentacular cells responsible for the chemoreceptor activity of the carotid body | **The supporting or sustentacular cells responsible for the [[chemoreceptor]] activity of the [[carotid body]] | ||
*The | *The characteristic finding of this [[tumor]] is: | ||
:*Chief cells Arranged in distinctive pattern called cell balls (zellballen) | :*Chief cells Arranged in distinctive pattern called [[cell]] balls (zellballen) | ||
:*Separated by fibrovascular stroma and surrounded by sustentacular cells | :*Separated by fibrovascular stroma and surrounded by [[sustentacular]] cells | ||
*The tumor is highly vascular. | :*The [[cytoplasm]] is [[pale]] and diffuse with occasional presence of the [[eosinophilic]] [[granules]].<ref>{{cite book | last = Bibbo | first = Marluce | title = Comprehensive cytopathology | publisher = Saunders/Elsevier | location = Philadelphia, PA | year = 2008 | isbn = 978-1-4160-4208-2 }}</ref> | ||
*Although there is no well-accepted histologic criteria for the diagnosis of malignant tumors, worrisome histologic features include:<ref name="WienekeSmith2009">{{cite journal|last1=Wieneke|first1=Jacqueline A.|last2=Smith|first2=Alice|title=Paraganglioma: Carotid Body Tumor|journal=Head and Neck Pathology|volume=3|issue=4|year=2009|pages=303–306|issn=1936-055X|doi=10.1007/s12105-009-0130-5}}</ref> | :*The nuclei are round to spindle shape. | ||
**Necrosis | *The [[tumor]] is highly [[vascular]]. | ||
**Extensive vascular or capsular invasion | *Although there is no well-accepted [[histologic]] criteria for the [[diagnosis]] of [[malignant]] [[tumors]], worrisome [[histologic]] features include:<ref name="WienekeSmith2009">{{cite journal|last1=Wieneke|first1=Jacqueline A.|last2=Smith|first2=Alice|title=Paraganglioma: Carotid Body Tumor|journal=Head and Neck Pathology|volume=3|issue=4|year=2009|pages=303–306|issn=1936-055X|doi=10.1007/s12105-009-0130-5}}</ref> | ||
**Increased mitotic activity | **[[Necrosis]] | ||
**Atypical mitotic figures | **Extensive [[vascular]] or capsular [[invasion]] | ||
**Increased [[mitotic]] activity | |||
**Atypical [[mitotic]] figures | |||
{| | |||
|[[File:Neck Paraganglioma CarotidBody HP CTR.jpg|thumb|400px|Contributed by Sarahkayb in wikimedia.commons]] | |||
<br style="clear:left" /> | |||
|- | |||
|} | |||
==Immunohistochemistry== | ==Immunohistochemistry== | ||
*Type 1 cells, sustentacular cells, are stained by:<ref name="pmid8058707">{{cite journal |vauthors=Schmid KW, Schröder S, Dockhorn-Dworniczak B, Kirchmair R, Tötsch M, Böcker W, Fischer-Colbrie R |title=Immunohistochemical demonstration of chromogranin A, chromogranin B, and secretogranin II in extra-adrenal paragangliomas |journal=Mod. Pathol. |volume=7 |issue=3 |pages=347–53 |date=April 1994 |pmid=8058707 |doi= |url=}}</ref> | *Type 1 cells, sustentacular cells, are stained by:<ref name="pmid8058707">{{cite journal |vauthors=Schmid KW, Schröder S, Dockhorn-Dworniczak B, Kirchmair R, Tötsch M, Böcker W, Fischer-Colbrie R |title=Immunohistochemical demonstration of chromogranin A, chromogranin B, and secretogranin II in extra-adrenal paragangliomas |journal=Mod. Pathol. |volume=7 |issue=3 |pages=347–53 |date=April 1994 |pmid=8058707 |doi= |url=}}</ref> | ||
**S-100 | **[[S-100]] | ||
*Type 2 cells, cheif cell, are stained by: | *Type 2 cells, cheif cell, are stained by: | ||
**Chromogranins | **[[Chromogranin|Chromogranins]] | ||
**Synaptophysisn | **Synaptophysisn | ||
*The tumor cells may also be positive for other markers of neuroendocrine differentiation such as:<ref name="WienekeSmith2009">{{cite journal|last1=Wieneke|first1=Jacqueline A.|last2=Smith|first2=Alice|title=Paraganglioma: Carotid Body Tumor|journal=Head and Neck Pathology|volume=3|issue=4|year=2009|pages=303–306|issn=1936-055X|doi=10.1007/s12105-009-0130-5}}</ref> | *The [[Tumor cell|tumor cells]] may also be positive for other markers of [[neuroendocrine]] differentiation such as:<ref name="WienekeSmith2009">{{cite journal|last1=Wieneke|first1=Jacqueline A.|last2=Smith|first2=Alice|title=Paraganglioma: Carotid Body Tumor|journal=Head and Neck Pathology|volume=3|issue=4|year=2009|pages=303–306|issn=1936-055X|doi=10.1007/s12105-009-0130-5}}</ref> | ||
**CD56 | **[[CD56]] | ||
**Neuron specific enolase | **[[NES|Neuron specific enolase]] | ||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
[[Category:Medicine]] | [[Category:Medicine]] | ||
[[Category:Oncology]] | [[Category:Oncology]] | ||
[[Category: | [[Category:Up-To-Date]] | ||
[[Category:Surgery]] | [[Category:Surgery]] | ||
Latest revision as of 20:49, 29 July 2020
|
Carotid body tumor Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Carotid body tumor pathophysiology On the Web |
|
American Roentgen Ray Society Images of Carotid body tumor pathophysiology |
|
Risk calculators and risk factors for Carotid body tumor pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sahar Memar Montazerin, M.D.[2] Maria Fernanda Villarreal, M.D. [3]
Overview
The carotid body is an ellipsoid-like structure located in the adventitia or periadventitial tissue of the bifurcation of the common carotid artery. This organ is a chemo-receptor and its function is the monitoring of arterial blood oxygen and carbon dioxide levels. The exact pathogenesis of carotid body tumor is not fully understood. however, the overgrowth of chemoreceptor paraganglioma cells in the carotid body leads to the formation of carotid body tumor. Recent litreture has suggested the role of several germline mutations in the pathogenesis of this tumor. Also, the hyperplastic form of the tumor has been associated with conditions that causes chronic hypoxia.
Pathophysiology
Anatomy
- The carotid body is an ellipsoid-like structure located in the adventitia or periadventitial tissue of the bifurcation of the common carotid artery.[1]
- The normal carotid body weighs less than 15 mg and measures between 3 to 5 mm.
- This structure innervated by the hearing branch of the glossopharyngeal nerve, however, the carotid body is in close proximity of a majority of important nerves.
- The blood supply to the carotid body is provided by ascending pharyngeal artery, which is the branch of the external carotid artery.
Physiology
- The carotid body is a chemo-receptor and its function is the monitoring of arterial blood oxygen and carbon dioxide levels.[2][3]
- This organ is sensitive to the reduction of oxygen partial pressure in the blood which results in reflexive activation of the autonomic nervous system and the resultant increase in the
ventilation rate.
Pathogenesis
- Carotid body tumor is a neuroendocrine neoplasm originating from carotid body.[4]
- Carotid body is a component of the autonomic nervous system derived from neural crest cells of the embryonic third branchial arch.[1]
- The overgrowth of chemoreceptor paraganglioma cells in the carotid body leads to the formation of carotid body tumor.
- Carotid body tumors are normally located in the medial aspect adventitia of the carotid bifurcation.
- Carotid body tumor occurs sporadicly in 85% to 90% of the cases.[1][5]
- Recent litreture has suggested the role of several germline mutations in the pathogenesis of this tumor.[6]
- It has been explained that the hyperplastic form of the tumor is associated with chronic hypoxia due to such as:[1][7]
- The tumor may be bilateral in fewer than 5% of the sporadic cases.
- The tumor may be familial in the rest 10% to 15%.
Genetics
- The familial form of the tumor is associated with a mutation in a gene located on 11q23.[8]
- The disease inheritance is through autosomal dominance.[9]
- The following genes has been linked to an increased incidence of paraganglioma including carotid body tumor:[10][6]
- Succinate dehydrogenase (SDH) complex subunits B, C, and D.
- RET
- Von Hippel-Lindau (VHL)
- Neurofibromatosis type I (NF1)
Associated Conditions
Conditions associated with carotid body tumor include:[6]
- Von Hippel-Lindau syndrome
- Neurofibromatosis type I (von Recklinghausen disease)
- MEN 2A
- MEN 2B
- Carney's triad which consists of:[11]
- Gastric leiomyosarcoma
- Pulmonary chondroma
- Extraadrenal paraganglioma
Gross Pathology
|Characteristic findings of carotid body tumor, include:[6]
- Well-circumscribed with psudocapsule
- The size of the tumor varies greatly and it may be as large as 10 cm
- The cutting surface is solid with a smooth, rubbery texture

|
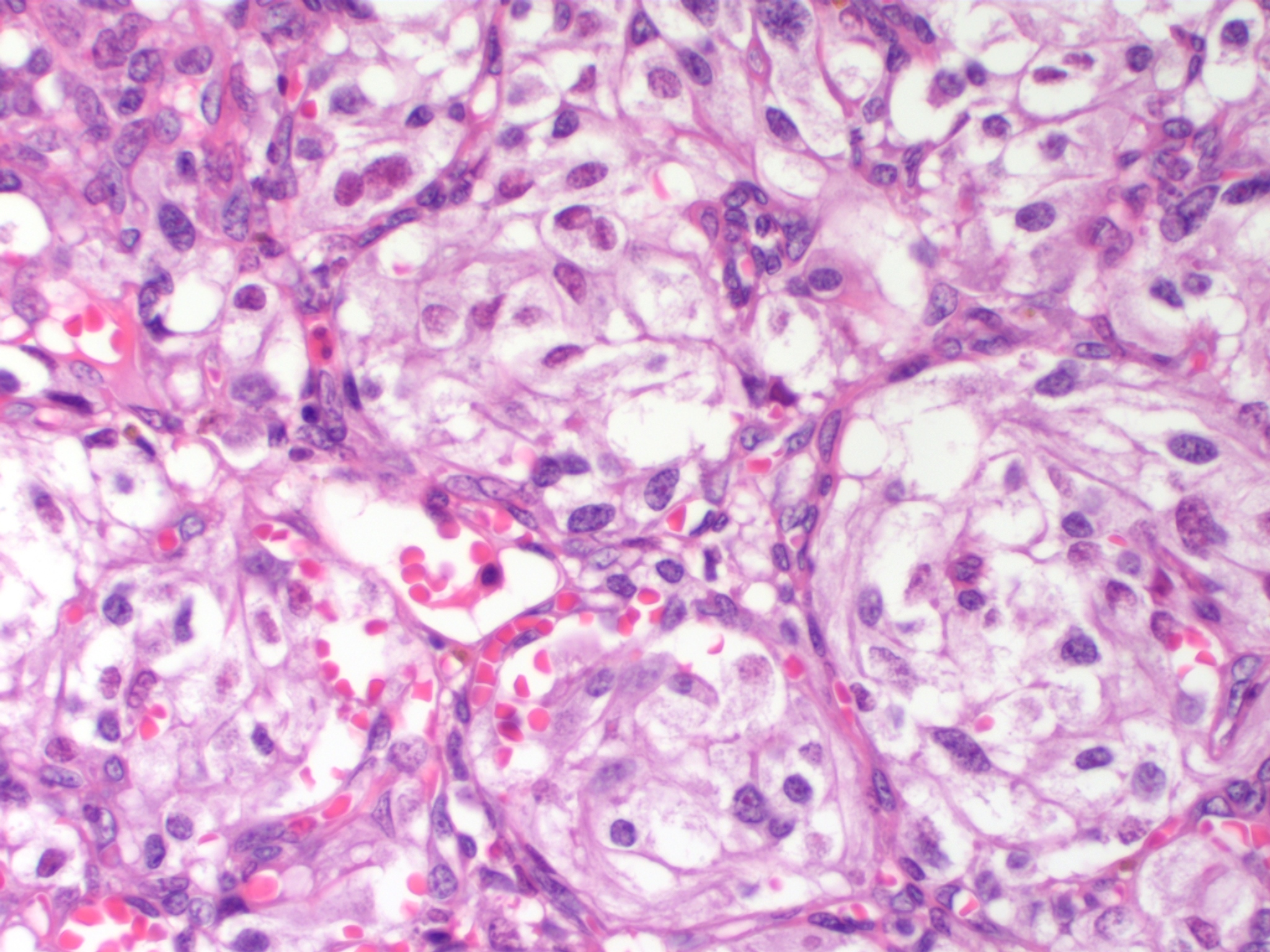
Microscopic Pathology
- On microscopic histopathological analysis, carotid body tumor composed of:
- The chief or paraganglionic cells composing the predominant part of the tumor and contain eosinophilic granular materials and oval or round nuclei.[12]
- The supporting or sustentacular cells responsible for the chemoreceptor activity of the carotid body
- The characteristic finding of this tumor is:
- Chief cells Arranged in distinctive pattern called cell balls (zellballen)
- Separated by fibrovascular stroma and surrounded by sustentacular cells
- The cytoplasm is pale and diffuse with occasional presence of the eosinophilic granules.[13]
- The nuclei are round to spindle shape.
- The tumor is highly vascular.
- Although there is no well-accepted histologic criteria for the diagnosis of malignant tumors, worrisome histologic features include:[6]
|
Immunohistochemistry
- Type 1 cells, sustentacular cells, are stained by:[14]
- Type 2 cells, cheif cell, are stained by:
- Chromogranins
- Synaptophysisn
- The tumor cells may also be positive for other markers of neuroendocrine differentiation such as:[6]
References
- ↑ 1.0 1.1 1.2 1.3 Burgess, Alfred; Calderon, Moises; Jafif-Cojab, Marcos; Jorge, Diego; Balanza, Ricardo (2017). "Bilateral carotid body tumor resection in a female patient". International Journal of Surgery Case Reports. 41: 387–391. doi:10.1016/j.ijscr.2017.11.019. ISSN 2210-2612.
- ↑ Robertson, David (2012). Primer on the autonomic nervous system. London: Elsevier. ISBN 978-0-12-386525-0.
- ↑ Zufall, Frank (2016). Chemosensory transduction : the detection of odors, tastes, and other chemostimuli. London, UK: Academic Press is an imprint of Elsevier. ISBN 978-0-12-801694-7.
- ↑ Boedeker CC, Ridder GJ, Schipper J (2005). "Paragangliomas of the head and neck: diagnosis and treatment". Fam. Cancer. 4 (1): 55–9. doi:10.1007/s10689-004-2154-z. PMID 15883711.
- ↑ Ridge, Brian A.; Brewster, David C.; Darling, R. Clement; Cambria, Richard P.; LaMuraglia, Glenn M.; Abbott, William M. (1993). "Familial Carotid Body Tumors: Incidence and Implications". Annals of Vascular Surgery. 7 (2): 190–194. doi:10.1007/BF02001015. ISSN 0890-5096.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 Wieneke, Jacqueline A.; Smith, Alice (2009). "Paraganglioma: Carotid Body Tumor". Head and Neck Pathology. 3 (4): 303–306. doi:10.1007/s12105-009-0130-5. ISSN 1936-055X.
- ↑ Sajid, M.S.; Hamilton, G.; Baker, D.M. (2007). "A Multicenter Review of Carotid Body Tumour Management". European Journal of Vascular and Endovascular Surgery. 34 (2): 127–130. doi:10.1016/j.ejvs.2007.01.015. ISSN 1078-5884.
- ↑ Fennessy, B. G.; Kozakewich, H. P. W.; Silvera, M.; Frerichs, K.; Lillhei, C. W.; Poe, D.; Rahbar, R. (2009). "The presentation and management of multiple paraganglioma in head and neck". Irish Journal of Medical Science. 180 (3): 757–760. doi:10.1007/s11845-009-0338-0. ISSN 0021-1265.
- ↑ Young AL, Baysal BE, Deb A, Young WF (September 2002). "Familial malignant catecholamine-secreting paraganglioma with prolonged survival associated with mutation in the succinate dehydrogenase B gene". J. Clin. Endocrinol. Metab. 87 (9): 4101–5. doi:10.1210/jc.2002-020312. PMID 12213855.
- ↑ Davila, Victor J.; Chang, James M.; Stone, William M.; Fowl, Richard J.; Bower, Thomas C.; Hinni, Michael L.; Money, Samuel R. (2016). "Current surgical management of carotid body tumors". Journal of Vascular Surgery. 64 (6): 1703–1710. doi:10.1016/j.jvs.2016.05.076. ISSN 0741-5214.
- ↑ Carney JA, Sheps SG, Go VL, Gordon H (June 1977). "The triad of gastric leiomyosarcoma, functioning extra-adrenal paraganglioma and pulmonary chondroma". N. Engl. J. Med. 296 (26): 1517–8. doi:10.1056/NEJM197706302962609. PMID 865533.
- ↑ Patetsios, Peter; Gable, Dennis R.; Garrett, Wilson V.; Lamont, Jeffrey P.; Kuhn, Joseph A.; Shutze, William P.; Kourlis, Harry; Grimsley, Bradley; Pearl, Gregory J.; Smith, Bertram L.; Talkington, C.M.; Thompson, Jesse E. (2002). "Management of Carotid Body Paragangliomas and Review of a 30-year Experience". Annals of Vascular Surgery. 16 (3): 331–338. doi:10.1007/s10016-001-0106-8. ISSN 0890-5096.
- ↑ Bibbo, Marluce (2008). Comprehensive cytopathology. Philadelphia, PA: Saunders/Elsevier. ISBN 978-1-4160-4208-2.
- ↑ Schmid KW, Schröder S, Dockhorn-Dworniczak B, Kirchmair R, Tötsch M, Böcker W, Fischer-Colbrie R (April 1994). "Immunohistochemical demonstration of chromogranin A, chromogranin B, and secretogranin II in extra-adrenal paragangliomas". Mod. Pathol. 7 (3): 347–53. PMID 8058707.