COVID-19-associated headache
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Fahimeh Shojaei, M.D. Syed Musadiq Ali M.B.B.S.[2]
Synonyms and keywords:
Overview
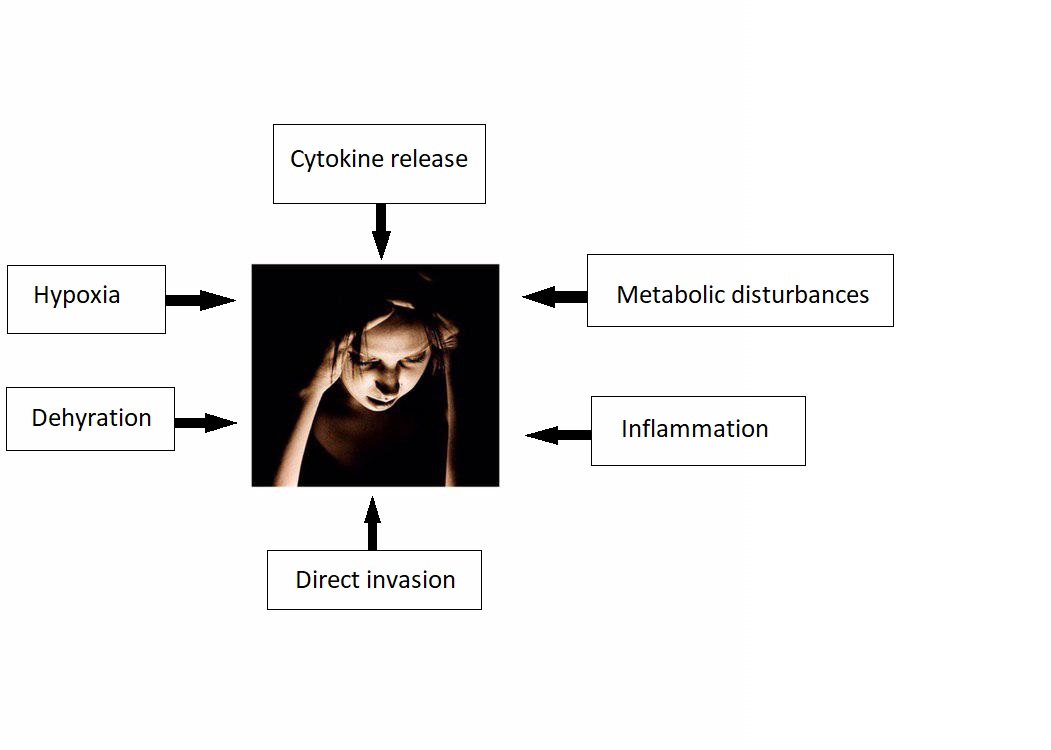
The association between COVID-19 and headache was made in 2020. COVID-19 associated headache may be caused by SARS-CoV-2 virus. There is no established system for the classification of COVID-19 associated headache. The exact pathogenesis of headache in COVID 19 patients is not fully understood. It is thought that headache is the result of cytokine release, direct invasion, metabolic disturbances, inflammation, dehydration, and hypoxia. COVID-19-associated headache must be differentiated from other diseases that cause headache, such as migraine, tension-type headache, cluster headache, seizure, meningitis, encephalitis, neurosyphilis, SAH, subdural hematoma, brain tumor, hypertensive encephalopathy, brain abscess, multiple sclerosis, hemorrhagic stroke, Wernickes encephalopathy, and drug toxicity. A positive history of fever and cough in addition to headache is suggestive of COVID-19-associated headache.
Historical Perspective
- The association between COVID-19 and headache was made in December, 2019 during SARS-CoV-2 outbreak initiated in Wuhan, Hubei Province, China.[1]
Classification
- There is no established system for the classification of COVID-19 associated headache.
Pathophysiology
- The exact pathogenesis of headache in COVID 19 patients is not fully understood.
- It is thought that headache is the result of:[2][3][4][5]
- Cytokine release
- There is higher concentration on IL-6 and INF-gamma in patients infected with SARS/ CoV2.
- Cytokines can disrupt blood brain barrier and cause tissue injury and cerebral edema.
- Direct invasion
- Metabolic disturbances
- Inflammation
- Dehydration
- Hypoxia
- Cytokine release
Causes
- COVID-19 associated headache may be caused by SARS-CoV-2 virus.
Differentiating COVID-19-associated headache from other Diseases
- For further information about the differential diagnosis, click here.
- To view the differential diagnosis of COVID-19, click here.
Epidemiology and Demographics
Incidence / Prevalence
- WHO reported that more than 462,801 people have been infected worldwide, more than 380,723 of which are outside of China.[6]
- The incidence/prevalence of COVID-19-associated headache is still unknown.
- Guan et al. recently reported 13 percent of COVID-19-associated headache among 1099 laboratory-confirmed cases.
Age
- There is insufficient information regarding age-specific prevalence or incidence of COVID-19-associated headache.
Gender
- There is insufficient information regarding gender-specific prevalence or incidence of COVID-19-associated headache.
Race
- There is insufficient information regarding race-specific prevalence or incidence of COVID-19-associated headache.
Risk Factors
- There are no established risk factors for COVID-19-associated headache.
Screening
Natural History, Complications, and Prognosis
Natural History
- At this point natural history of COVID-19-associated headache is unknown.
- Further studies are needed to better understand the COVID-19-associated headache.
Complication
- Patients with a history migraine may experience headache as their first symptom, these patients experience more severe headache and are more disabled by the infection compared with age‐matched cohorts.
- Further studies are needed to better understand complication.
- Larger retrospective studies are needed for evaluating the experience of COVID‐19 in patients with a history of a primary headache disorder.
Diagnosis
Diagnostic Study of Choice
- There are no established criteria for the diagnosis of COVID-19-associated headache.
History and Symptoms
- The hallmark of COVID-19-associated headache is headache.
- A positive history of fever and cough in addition to headache is suggestive of COVID-19-associated headache.
Common Symptoms
- Common symptoms of COVID-19-associated headache are:
- Fever,
- Shortness of breath
- Cognitive impairment
- Cough
- Fatigue
Less Common Symptoms
Physical Examination
- Patients with COVID-19-associated headache usually appear normal.
- Physical examination of patients with COVID-19-associated headache is usually remarkable for fever, cough, and malaise.
Laboratory Findings
- Additional diagnostic tests like blood chemistry and urine analysis may be needed to rule out other medical conditions.
- There are no diagnostic laboratory findings associated with COVID-19-associated headache.
Electrocardiogram
X-ray
Echocardiography or Ultrasound
- There are no echocardiography/ultrasound findings associated with COVID-19-associated headache.
CT scan
- There are no CT scan findings associated with COVID-19-associated headache.
MRI
- There are no MRI findings associated with COVID-19-associated headache.
Other Imaging Findings
- There are no other imaging findings associated with COVID-19-associated headache.
Other Diagnostic Studies
- There are no other diagnostic studies associated with COVID-19-associated headache.
Treatment
Medical Therapy
- Medical therapy for COVID-assocaited-headache is still controversial[7].
- The use of NSAIDs, who received treatment early in the disease causes worsening of COVID-19 symptoms according to some anecdotal evidences.
- In March 11, 2020, Fang et al. reported the hypothesis that ibuprofen (40 mg/kg/dose)[8] can increase the risk of developing severe and fatal COVID-19 since ibuprofen is known to upregulate ACE2 receptors[9].
- In March 23, 2020, US FDA announced that it is not aware of any evidence that NSAIDs such as ibuprofen could worsen COVID-19[10].
- The European Medicines Agency and World Health Organization (WHO) have not yet recommended that NSAIDs be avoided.
- Despite this recommendation, as a precautionary measure many providers are avoiding NSAIDs in patients with COVID-19.
- In practice, the decision to continue or stop NSAIDs in patients with COVID-19 is made in collaboration between the treating physician and the patient, after a brief discussion on the limited available evidence.
- More data are needed before broad recommendations are made.
Surgery
Primary Prevention
- There are no established measures for the primary prevention of COVID-19 associated headache.
Secondary Prevention
- There are no established measures for the secondary prevention of COVID-19-associated headache.
References
- ↑ Meng X, Deng Y, Dai Z, Meng Z (June 2020). "COVID-19 and anosmia: A review based on up-to-date knowledge". Am J Otolaryngol. 41 (5): 102581. doi:10.1016/j.amjoto.2020.102581. PMC 7265845 Check
|pmc=value (help). PMID 32563019 Check|pmid=value (help). - ↑ Baig, Abdul Mannan; Khaleeq, Areeba; Ali, Usman; Syeda, Hira (2020). "Evidence of the COVID-19 Virus Targeting the CNS: Tissue Distribution, Host–Virus Interaction, and Proposed Neurotropic Mechanisms". ACS Chemical Neuroscience. 11 (7): 995–998. doi:10.1021/acschemneuro.0c00122. ISSN 1948-7193.
- ↑ St-Jean JR, Jacomy H, Desforges M, Vabret A, Freymuth F, Talbot PJ (August 2004). "Human respiratory coronavirus OC43: genetic stability and neuroinvasion". J. Virol. 78 (16): 8824–34. doi:10.1128/JVI.78.16.8824-8834.2004. PMC 479063. PMID 15280490.
- ↑ Rossi, Andrea (2008). "Imaging of Acute Disseminated Encephalomyelitis". Neuroimaging Clinics of North America. 18 (1): 149–161. doi:10.1016/j.nic.2007.12.007. ISSN 1052-5149.
- ↑ St-Jean, Julien R.; Jacomy, Hélène; Desforges, Marc; Vabret, Astrid; Freymuth, François; Talbot, Pierre J. (2004). "Human Respiratory Coronavirus OC43: Genetic Stability and Neuroinvasion". Journal of Virology. 78 (16): 8824–8834. doi:10.1128/JVI.78.16.8824-8834.2004. ISSN 0022-538X.
- ↑ Tu H, Tu S, Gao S, Shao A, Sheng J (2020). "Current epidemiological and clinical features of COVID-19; a global perspective from China". J Infect. 81 (1): 1–9. doi:10.1016/j.jinf.2020.04.011. PMC 7166041 Check
|pmc=value (help). PMID 32315723 Check|pmid=value (help). - ↑ Zhang J, Xie B, Hashimoto K (2020). "Current status of potential therapeutic candidates for the COVID-19 crisis". Brain Behav Immun. 87: 59–73. doi:10.1016/j.bbi.2020.04.046. PMC 7175848 Check
|pmc=value (help). PMID 32334062 Check|pmid=value (help). - ↑ MaassenVanDenBrink A, de Vries T, Danser A (April 2020). "Headache medication and the COVID-19 pandemic". J Headache Pain. 21 (1): 38. doi:10.1186/s10194-020-01106-5. PMC 7183387 Check
|pmc=value (help). PMID 32334535 Check|pmid=value (help). Vancouver style error: initials (help) - ↑ Fang L, Karakiulakis G, Roth M (2020) Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir Med 8 (4):e21. DOI:10.1016/S2213-2600(20)30116-8 PMID: 32171062
- ↑ FitzGerald GA (2020) Misguided drug advice for COVID-19. Science 367 (6485):1434. DOI:10.1126/science.abb8034 PMID: 32198292