COVID-19-associated headache: Difference between revisions
No edit summary |
Sam Norris (talk | contribs) |
||
| (One intermediate revision by one other user not shown) | |||
| Line 6: | Line 6: | ||
==Overview== | ==Overview== | ||
The association between COVID-19 and headache was made in 2020. COVID-19 associated headache may be caused by [[SARS-CoV-2|SARS-CoV-2 virus]]. There is no established system for the [[classification]] of COVID-19 associated headache. The exact [[pathogenesis]] of [[headache]] in COVID 19 patients is not fully understood. It is thought that [[Cluster headache|headache]] is the result of [[cytokine]] release, direct [[invasion]], metabolic disturbances, [[Cervicitis|inflammation]], [[dehydration]], and [[hypoxia]]. COVID-19-associated headache must be differentiated from other diseases that cause [[headache]], such as [[migraine]], [[tension-type headache]], [[Cluster headache (patient information)|cluster headache]], [[seizure]], [[meningitis]], [[encephalitis]], [[neurosyphilis]], [[Subarachnoid hemorrhage|SAH]], [[subdural hematoma]], [[brain tumor]], [[hypertensive encephalopathy]], [[brain abscess]], [[multiple sclerosis]], [[hemorrhagic stroke]], [[Wernicke's encephalopathy|Wernickes encephalopathy]], and [[drug toxicity]]. A positive history of [[fever]] and [[cough]] in addition to headache is suggestive of [[COVID]]-19-associated headache. | The association between COVID-19 and headache was made in 2020. COVID-19 associated headache may be caused by the [[SARS-CoV-2|SARS-CoV-2 virus]]. There is no established system for the [[classification]] of COVID-19 associated headache. The exact [[pathogenesis]] of [[headache]] in COVID-19 patients is not fully understood. It is thought that [[Cluster headache|headache]] is the result of [[cytokine]] release, direct [[invasion]], metabolic disturbances, [[Cervicitis|inflammation]], [[dehydration]], and [[hypoxia]]. COVID-19-associated headache must be differentiated from other diseases that cause [[headache]], such as [[migraine]], [[tension-type headache]], [[Cluster headache (patient information)|cluster headache]], [[seizure]], [[meningitis]], [[encephalitis]], [[neurosyphilis]], [[Subarachnoid hemorrhage|SAH]], [[subdural hematoma]], [[brain tumor]], [[hypertensive encephalopathy]], [[brain abscess]], [[multiple sclerosis]], [[hemorrhagic stroke]], [[Wernicke's encephalopathy|Wernickes encephalopathy]], and [[drug toxicity]]. A positive history of [[fever]] and [[cough]] in addition to headache is suggestive of [[COVID]]-19-associated headache. | ||
==Historical Perspective== | ==Historical Perspective== | ||
* The association between COVID-19 and [[headache]] was made in December, 2019 during [[SARS-CoV-2]] [[outbreak]] initiated in Wuhan, Hubei Province, China.<ref name="pmid32563019">{{cite journal |vauthors=Meng X, Deng Y, Dai Z, Meng Z |title=COVID-19 and anosmia: A review based on up-to-date knowledge |journal=Am J Otolaryngol |volume=41 |issue=5 |pages=102581 |date=June 2020 |pmid=32563019 |pmc=7265845 |doi=10.1016/j.amjoto.2020.102581 |url=}}</ref> | * The association between COVID-19 and [[headache]] was made in December, 2019 during the [[SARS-CoV-2]] [[outbreak]] initiated in Wuhan, Hubei Province, China.<ref name="pmid32563019">{{cite journal |vauthors=Meng X, Deng Y, Dai Z, Meng Z |title=COVID-19 and anosmia: A review based on up-to-date knowledge |journal=Am J Otolaryngol |volume=41 |issue=5 |pages=102581 |date=June 2020 |pmid=32563019 |pmc=7265845 |doi=10.1016/j.amjoto.2020.102581 |url=}}</ref> | ||
==Classification== | ==Classification== | ||
| Line 72: | Line 72: | ||
===Natural History=== | ===Natural History=== | ||
* At this point [[natural history]] of [[COVID-19]]-associated [[headache]] is unknown. | * At this point, the [[natural history]] of [[COVID-19]]-associated [[headache]] is unknown. | ||
* Further studies are needed to better understand the [[COVID-19]]-associated [[headache]]. | * Further studies are needed to better understand the [[COVID-19]]-associated [[headache]]. | ||
===Complication=== | ===Complication=== | ||
* Patients with a history [[migraine]] may experience [[headache]] as their first [[symptom]], these [[patients]] experience more severe [[headache]] and are more disabled by the [[HIV AIDS|infection]] compared with age‐matched [[cohorts]]. | * Patients with a history [[migraine]] may experience [[headache]] as their first [[symptom]], and these [[patients]] experience more severe [[headache]] and are more disabled by the [[HIV AIDS|infection]] compared with age‐matched [[cohorts]]. | ||
* Further studies are needed to better understand [[complication]]. | * Further studies are needed to better understand [[complication]]<nowiki/>s. | ||
* Larger retrospective studies are needed for evaluating the experience of [[COVID-19|COVID‐19]] in [[patients]] with a [[History and Physical examination|history]] of a primary [[headache]] disorder. | * Larger retrospective studies are needed for evaluating the experience of [[COVID-19|COVID‐19]] in [[patients]] with a [[History and Physical examination|history]] of a primary [[headache]] disorder. | ||
| Line 84: | Line 84: | ||
===Diagnostic Study of Choice=== | ===Diagnostic Study of Choice=== | ||
* The [[diagnosis]] of COVID-19-associated [[headache]] is based on the [[clinical]] presentation | * The [[diagnosis]] of COVID-19-associated [[headache]] is based on the [[clinical]] presentation. | ||
* There are no established criteria for the diagnosis of COVID-19-associated headache. | * There are no established criteria for the diagnosis of COVID-19-associated headache. | ||
| Line 97: | Line 97: | ||
*Common [[symptoms]] of COVID-19-associated [[headache]] are: | *Common [[symptoms]] of COVID-19-associated [[headache]] are: | ||
**[[Fever]] | **[[Fever]] | ||
**[[Shortness of breath]] | **[[Shortness of breath]] | ||
**[[Consciousness|Cognitive]] impairment | **[[Consciousness|Cognitive]] impairment | ||
| Line 105: | Line 105: | ||
====Less Common Symptoms==== | ====Less Common Symptoms==== | ||
*Less common [[symptoms]] of COVID-19-associated [[headache]] are | *Less common [[symptoms]] of COVID-19-associated [[headache]] are: | ||
**[[Facial droop]] | **[[Facial droop]] | ||
**[[Myoclonus]] | **[[Myoclonus]] | ||
**[[Dysarthria]] | **[[Dysarthria]] | ||
**[[Generalized seizure|S]]<nowiki/>[[Generalized seizure|eiz]]<nowiki/>[[Generalized seizure|ures]] | **<nowiki/><nowiki/>[[Generalized seizure|S]]<nowiki/>[[Generalized seizure|eiz]]<nowiki/>[[Generalized seizure|ures]] | ||
**[[Paralysis| | **[[Paralysis|P]]<nowiki/>[[Paralysis|ar]][[Paralysis|a]]<nowiki/>[[Paralysis|ly]][[Paralysis|sis]] | ||
**[[Dizziness]] | **[[Dizziness]] | ||
**[[Sedation]] | **[[Sedation]] | ||
| Line 180: | Line 180: | ||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
[[Category:Up-To-Date]] | |||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
Latest revision as of 18:10, 22 July 2020
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Fahimeh Shojaei, M.D. Syed Musadiq Ali M.B.B.S.[2]
Synonyms and keywords:
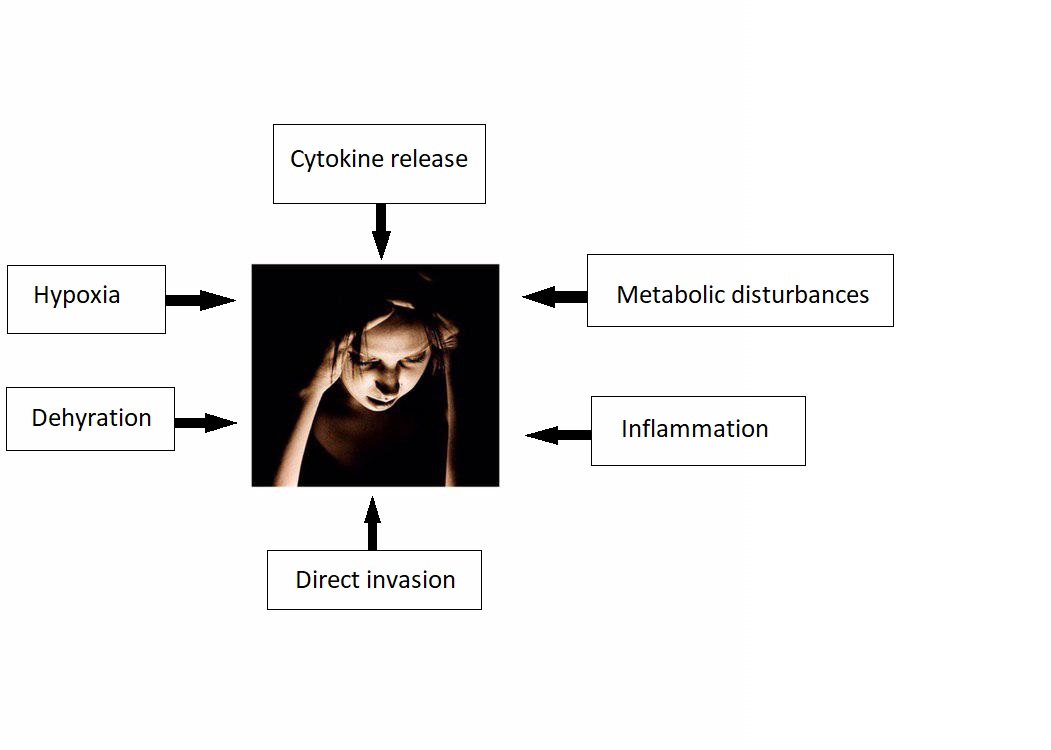
Overview
The association between COVID-19 and headache was made in 2020. COVID-19 associated headache may be caused by the SARS-CoV-2 virus. There is no established system for the classification of COVID-19 associated headache. The exact pathogenesis of headache in COVID-19 patients is not fully understood. It is thought that headache is the result of cytokine release, direct invasion, metabolic disturbances, inflammation, dehydration, and hypoxia. COVID-19-associated headache must be differentiated from other diseases that cause headache, such as migraine, tension-type headache, cluster headache, seizure, meningitis, encephalitis, neurosyphilis, SAH, subdural hematoma, brain tumor, hypertensive encephalopathy, brain abscess, multiple sclerosis, hemorrhagic stroke, Wernickes encephalopathy, and drug toxicity. A positive history of fever and cough in addition to headache is suggestive of COVID-19-associated headache.
Historical Perspective
- The association between COVID-19 and headache was made in December, 2019 during the SARS-CoV-2 outbreak initiated in Wuhan, Hubei Province, China.[1]
Classification
- There is no established system for the classification of COVID-19 associated headache.
Pathophysiology
- The exact pathogenesis of headache in COVID 19 patients is not fully understood.
- It is thought that headache is the result of:[2][3][4][5]
- Cytokine release
- There is higher concentration on IL-6 and INF-gamma in patients infected with SARS/ CoV2.
- Cytokines can disrupt blood brain barrier and cause tissue injury and cerebral edema.
- Direct invasion
- Metabolic disturbances
- Inflammation
- Dehydration
- Hypoxia
- Cytokine release
Causes
- COVID-19 associated headache may be caused by SARS-CoV-2 virus.
Differentiating COVID-19-associated headache from other Diseases
- For further information about the differential diagnosis, click here.
- To view the differential diagnosis of COVID-19, click here.
Epidemiology and Demographics
Incidence / Prevalence
- WHO reported that more than 462,801 people have been infected worldwide, more than 380,723 of which are outside of China.[6]
- The incidence/prevalence of COVID-19-associated headache is still unknown.
- Guan et al. recently reported 13 percent of COVID-19-associated headache among 1099 laboratory-confirmed cases.
Age
- There is insufficient information regarding age-specific prevalence or incidence of COVID-19-associated headache.
Gender
- There is insufficient information regarding gender-specific prevalence or incidence of COVID-19-associated headache.
Race
- There is insufficient information regarding race-specific prevalence or incidence of COVID-19-associated headache.
Risk Factors
- There are no established risk factors for COVID-19-associated headache.
Screening
Natural History, Complications, and Prognosis
Natural History
- At this point, the natural history of COVID-19-associated headache is unknown.
- Further studies are needed to better understand the COVID-19-associated headache.
Complication
- Patients with a history migraine may experience headache as their first symptom, and these patients experience more severe headache and are more disabled by the infection compared with age‐matched cohorts.
- Further studies are needed to better understand complications.
- Larger retrospective studies are needed for evaluating the experience of COVID‐19 in patients with a history of a primary headache disorder.
Diagnosis
Diagnostic Study of Choice
- There are no established criteria for the diagnosis of COVID-19-associated headache.
History and Symptoms
- The hallmark of COVID-19-associated headache is headache.
- A positive history of fever and cough in addition to headache is suggestive of COVID-19-associated headache.
Common Symptoms
- Common symptoms of COVID-19-associated headache are:
- Fever
- Shortness of breath
- Cognitive impairment
- Cough
- Fatigue
Less Common Symptoms
Physical Examination
- Patients with COVID-19-associated headache usually appear normal.
- Physical examination of patients with COVID-19-associated headache is usually remarkable for fever, cough, and malaise.
Laboratory Findings
- Additional diagnostic tests like blood chemistry and urine analysis may be needed to rule out other medical conditions.
- There are no diagnostic laboratory findings associated with COVID-19-associated headache.
Electrocardiogram
X-ray
Echocardiography or Ultrasound
- There are no echocardiography/ultrasound findings associated with COVID-19-associated headache.
CT scan
- There are no CT scan findings associated with COVID-19-associated headache.
MRI
- There are no MRI findings associated with COVID-19-associated headache.
Other Imaging Findings
- There are no other imaging findings associated with COVID-19-associated headache.
Other Diagnostic Studies
- There are no other diagnostic studies associated with COVID-19-associated headache.
Treatment
Medical Therapy
- Medical therapy for COVID-assocaited-headache is still controversial.[7][8][9][10]
- The use of NSAIDs, who received treatment early in the disease causes worsening of COVID-19 symptoms according to some anecdotal evidences.
- In March 11, 2020, Fang et al. reported the hypothesis that ibuprofen (40 mg/kg/dose) can increase the risk of developing severe and fatal COVID-19 since ibuprofen is known to upregulate ACE2 receptors.
- In March 23, 2020, US FDA announced that it is not aware of any evidence that NSAIDs such as ibuprofen could worsen COVID-19.
- The European Medicines Agency and World Health Organization (WHO) have not yet recommended that NSAIDs be avoided.
- Despite this recommendation, as a precautionary measure many providers are avoiding NSAIDs in patients with COVID-19.
- In practice, the decision to continue or stop NSAIDs in patients with COVID-19 is made in collaboration between the treating physician and the patient, after a brief discussion on the limited available evidence.
- More data are needed before broad recommendations are made.
Surgery
Primary Prevention
- There are no established measures for the primary prevention of COVID-19 associated headache.
Secondary Prevention
- There are no established measures for the secondary prevention of COVID-19-associated headache.
References
- ↑ Meng X, Deng Y, Dai Z, Meng Z (June 2020). "COVID-19 and anosmia: A review based on up-to-date knowledge". Am J Otolaryngol. 41 (5): 102581. doi:10.1016/j.amjoto.2020.102581. PMC 7265845 Check
|pmc=value (help). PMID 32563019 Check|pmid=value (help). - ↑ Baig, Abdul Mannan; Khaleeq, Areeba; Ali, Usman; Syeda, Hira (2020). "Evidence of the COVID-19 Virus Targeting the CNS: Tissue Distribution, Host–Virus Interaction, and Proposed Neurotropic Mechanisms". ACS Chemical Neuroscience. 11 (7): 995–998. doi:10.1021/acschemneuro.0c00122. ISSN 1948-7193.
- ↑ St-Jean JR, Jacomy H, Desforges M, Vabret A, Freymuth F, Talbot PJ (August 2004). "Human respiratory coronavirus OC43: genetic stability and neuroinvasion". J. Virol. 78 (16): 8824–34. doi:10.1128/JVI.78.16.8824-8834.2004. PMC 479063. PMID 15280490.
- ↑ Rossi, Andrea (2008). "Imaging of Acute Disseminated Encephalomyelitis". Neuroimaging Clinics of North America. 18 (1): 149–161. doi:10.1016/j.nic.2007.12.007. ISSN 1052-5149.
- ↑ St-Jean, Julien R.; Jacomy, Hélène; Desforges, Marc; Vabret, Astrid; Freymuth, François; Talbot, Pierre J. (2004). "Human Respiratory Coronavirus OC43: Genetic Stability and Neuroinvasion". Journal of Virology. 78 (16): 8824–8834. doi:10.1128/JVI.78.16.8824-8834.2004. ISSN 0022-538X.
- ↑ Tu H, Tu S, Gao S, Shao A, Sheng J (2020). "Current epidemiological and clinical features of COVID-19; a global perspective from China". J Infect. 81 (1): 1–9. doi:10.1016/j.jinf.2020.04.011. PMC 7166041 Check
|pmc=value (help). PMID 32315723 Check|pmid=value (help). - ↑ Zhang J, Xie B, Hashimoto K (2020). "Current status of potential therapeutic candidates for the COVID-19 crisis". Brain Behav Immun. 87: 59–73. doi:10.1016/j.bbi.2020.04.046. PMC 7175848 Check
|pmc=value (help). PMID 32334062 Check|pmid=value (help). - ↑ MaassenVanDenBrink A, de Vries T, Danser A (April 2020). "Headache medication and the COVID-19 pandemic". J Headache Pain. 21 (1): 38. doi:10.1186/s10194-020-01106-5. PMC 7183387 Check
|pmc=value (help). PMID 32334535 Check|pmid=value (help). Vancouver style error: initials (help) - ↑ Fang L, Karakiulakis G, Roth M (2020) Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir Med 8 (4):e21. DOI:10.1016/S2213-2600(20)30116-8 PMID: 32171062
- ↑ FitzGerald GA (2020) Misguided drug advice for COVID-19. Science 367 (6485):1434. DOI:10.1126/science.abb8034 PMID: 32198292