Burn pathophysiology: Difference between revisions
EmanAlademi (talk | contribs) No edit summary |
EmanAlademi (talk | contribs) No edit summary |
||
| Line 5: | Line 5: | ||
<br /> | <br /> | ||
==Pathophysiology== | ==Pathophysiology== | ||
Burns is the result of damage to the skin by a temperatures greater than 44 °C (111 °F), leads to cell and tissue damage because of breaking down of the cells proteins then start losing their three-dimensional shape42. Burn caused by Thermal injuries, Electrical injuries, Chemical injuries or Non-accidental injury. Non -accidental injury like:<ref name="pmid15191982">Hettiaratchy S, Dziewulski P (2004) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=15191982 ABC of burns: pathophysiology and types of burns.] ''BMJ'' 328 (7453):1427-9. [http://dx.doi.org/10.1136/bmj.328.7453.1427 DOI:10.1136/bmj.328.7453.1427] PMID: [https://pubmed.gov/PMID: 15191982 PMID: 15191982]</ref><ref name="urlPathophysiology and Current Management of Burn Injury : Advances in Skin & Wound Care">{{cite web |url=https://journals.lww.com/aswcjournal/fulltext/2005/07000/pathophysiology_and_current_management_of_burn.13.aspx |title=Pathophysiology and Current Management of Burn Injury : Advances in Skin & Wound Care |format= |work= |accessdate=}}</ref> | |||
{| class="wikitable" | {| class="wikitable" | ||
| colspan="1" rowspan="1" |• Obvious pattern from cigarettes, lighters, irons | | colspan="1" rowspan="1" |• Obvious pattern from cigarettes, lighters, irons | ||
| Line 23: | Line 23: | ||
| colspan="1" rowspan="1" |• Other signs of physical abuse—bruises of varied age, poorly kempt, lack of compliance with health care (such as no immunisations) | | colspan="1" rowspan="1" |• Other signs of physical abuse—bruises of varied age, poorly kempt, lack of compliance with health care (such as no immunisations) | ||
|} | |} | ||
<br /> | <br /><ref name="pmid23121414">{{cite journal |vauthors=Rojas Y, Finnerty CC, Radhakrishnan RS, Herndon DN |title=Burns: an update on current pharmacotherapy |journal=Expert Opin Pharmacother |volume=13 |issue=17 |pages=2485–94 |date=December 2012 |pmid=23121414 |pmc=3576016 |doi=10.1517/14656566.2012.738195 |url=}}</ref>Burn injuries result in both local and systemic responses:<ref name="urlABC of burns: Pathophysiology and types of burns">{{cite web |url=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC421790/ |title=ABC of burns: Pathophysiology and types of burns |format= |work= |accessdate=}}</ref> | ||
=== Local response === | |||
The three zones of a burn were described by Jackson in 1947. | |||
''Zone of coagulation''—This occurs at the point of maximum damage. In this zone there is irreversible tissue loss due to coagulation of the constituent proteins. | |||
''Zone of stasis''—The surrounding zone of stasis is characterized by decreased tissue perfusion. The tissue in this zone is potentially salvageable. The main aim of burns resuscitation is to increase tissue perfusion here and prevent any damage becoming irreversible. Additional insults—such as prolonged hypotension, infection, or edema—can convert this zone into an area of complete tissue loss. | |||
''Zone of hyperemia''—In this outermost zone tissue perfusion is increased. The tissue here will invariably recover unless there is severe sepsis or prolonged hypoperfusion. | |||
These three zones of a burn are three dimensional, and loss of tissue in the zone of stasis will lead to the wound deepening as well as widening. | |||
<br /> | |||
===Systemic response=== | |||
The increase of the catecholamines and cortisol,or The release of cytokines and other inflammatory mediators at the site of injury has a systemic effect once the burn reaches 30% of total body surface area. | |||
Increase of the catecholamines and cortisol lead to: | |||
''Cardiovascular changes''—Capillary permeability is increased, leading to loss of intravascular proteins and fluids into the interstitial compartment. Peripheral and splanchnic vasoconstriction occurs. Myocardial contractility is decreased, possibly due to release of tumor necrosis factor α. These changes, coupled with fluid loss from the burn wound, result in systemic hypotension and end organ hypoperfusion because of Increased levels of catecholamines. and a fast heart rate. | |||
'' | ''Metabolic changes''—The basal metabolic rate increases up(hypermetabolic) to three times its original rate because of Increased levels of catecholamines and cortisol . This, coupled with splanchnic hypoperfusion, necessitates early and aggressive enteral feeding to decrease catabolism and maintain gut integrity. | ||
'' | ''Immunological changes''—Non-specific down regulation of the immune response occurs, affecting both cell mediated and humoral pathways.pathways. | ||
Release of cytokines and other inflammatory mediators at the site of injury lead to: | |||
''Respiratory changes''—Inflammatory mediators cause bronchoconstriction, and in severe burns adult respiratory distress syndrome can occur. | |||
'' | gastrointestinal tract ''changes''— stomach ulcers because of the Poor blood flow to organs. | ||
'' | Renal ''changes''—kidney failure because of the Poor blood flow to organs | ||
Increased leakage of fluid from the capillaries, and subsequent tissue edema. This causes overall blood volume loss, with the remaining blood suffering significant plasma loss, making the blood more concentrated.<ref name="urlPorth Pathophysiology: Concepts of Altered Health States - Charlotte Pooler - كتب Google">{{cite web |url=https://books.google.ae/books?id=2-MFXOEG0lcC&pg=PA1516&redir_esc=y#v=onepage&q&f=false |title=Porth Pathophysiology: Concepts of Altered Health States - Charlotte Pooler - كتب Google |format= |work= |accessdate=}}</ref><br /> | |||
<br /> | |||
Revision as of 12:54, 25 September 2020
|
Burn Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Burn pathophysiology On the Web |
|
American Roentgen Ray Society Images of Burn pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Eman Alademi, M.D.[2]
Pathophysiology
Burns is the result of damage to the skin by a temperatures greater than 44 °C (111 °F), leads to cell and tissue damage because of breaking down of the cells proteins then start losing their three-dimensional shape42. Burn caused by Thermal injuries, Electrical injuries, Chemical injuries or Non-accidental injury. Non -accidental injury like:[1][2]
| • Obvious pattern from cigarettes, lighters, irons |
| • Burns to soles, palms, genitalia, buttocks, perineum |
| • Symmetrical burns of uniform depth |
| • No splash marks in a scald injury. A child falling into a bath will splash; one that is placed into it may not |
| • Restraint injuries on upper limbs |
| • Is there sparing of flexion creases—that is, was child in fetal position (position of protection) when burnt? Does this correlate to a “tide line” of scald—that is, if child is put into a fetal position, do the burns line up? |
| • “Doughnut sign,” an area of spared skin surrounded by scald. If a child is forcibly held down in a bath of hot water, the part in contact with the bottom of the bath will not burn, but the tissue around will |
| • Other signs of physical abuse—bruises of varied age, poorly kempt, lack of compliance with health care (such as no immunisations) |
[3]Burn injuries result in both local and systemic responses:[4]
Local response
The three zones of a burn were described by Jackson in 1947.
Zone of coagulation—This occurs at the point of maximum damage. In this zone there is irreversible tissue loss due to coagulation of the constituent proteins.
Zone of stasis—The surrounding zone of stasis is characterized by decreased tissue perfusion. The tissue in this zone is potentially salvageable. The main aim of burns resuscitation is to increase tissue perfusion here and prevent any damage becoming irreversible. Additional insults—such as prolonged hypotension, infection, or edema—can convert this zone into an area of complete tissue loss.
Zone of hyperemia—In this outermost zone tissue perfusion is increased. The tissue here will invariably recover unless there is severe sepsis or prolonged hypoperfusion.
These three zones of a burn are three dimensional, and loss of tissue in the zone of stasis will lead to the wound deepening as well as widening.
Systemic response
The increase of the catecholamines and cortisol,or The release of cytokines and other inflammatory mediators at the site of injury has a systemic effect once the burn reaches 30% of total body surface area.
Increase of the catecholamines and cortisol lead to:
Cardiovascular changes—Capillary permeability is increased, leading to loss of intravascular proteins and fluids into the interstitial compartment. Peripheral and splanchnic vasoconstriction occurs. Myocardial contractility is decreased, possibly due to release of tumor necrosis factor α. These changes, coupled with fluid loss from the burn wound, result in systemic hypotension and end organ hypoperfusion because of Increased levels of catecholamines. and a fast heart rate.
Metabolic changes—The basal metabolic rate increases up(hypermetabolic) to three times its original rate because of Increased levels of catecholamines and cortisol . This, coupled with splanchnic hypoperfusion, necessitates early and aggressive enteral feeding to decrease catabolism and maintain gut integrity.
Immunological changes—Non-specific down regulation of the immune response occurs, affecting both cell mediated and humoral pathways.pathways.
Release of cytokines and other inflammatory mediators at the site of injury lead to:
Respiratory changes—Inflammatory mediators cause bronchoconstriction, and in severe burns adult respiratory distress syndrome can occur.
gastrointestinal tract changes— stomach ulcers because of the Poor blood flow to organs.
Renal changes—kidney failure because of the Poor blood flow to organs
Increased leakage of fluid from the capillaries, and subsequent tissue edema. This causes overall blood volume loss, with the remaining blood suffering significant plasma loss, making the blood more concentrated.[5]
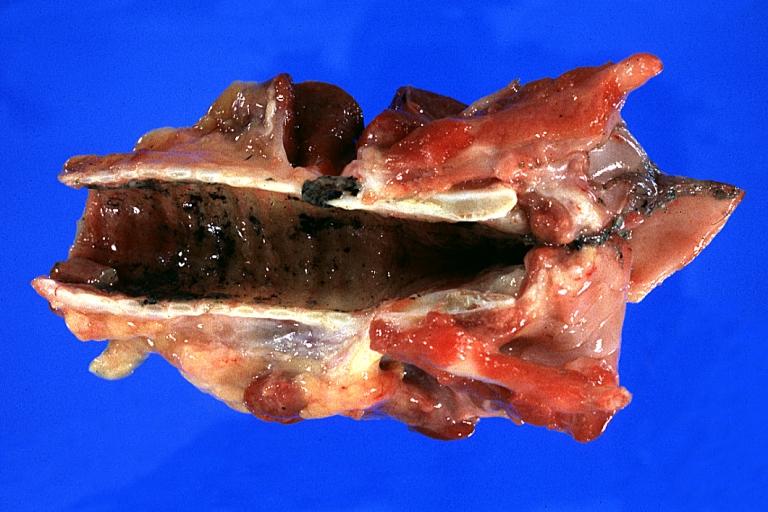
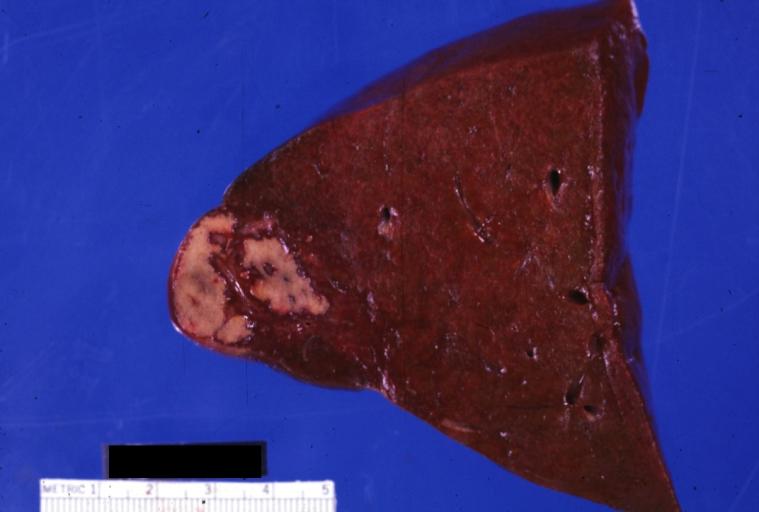
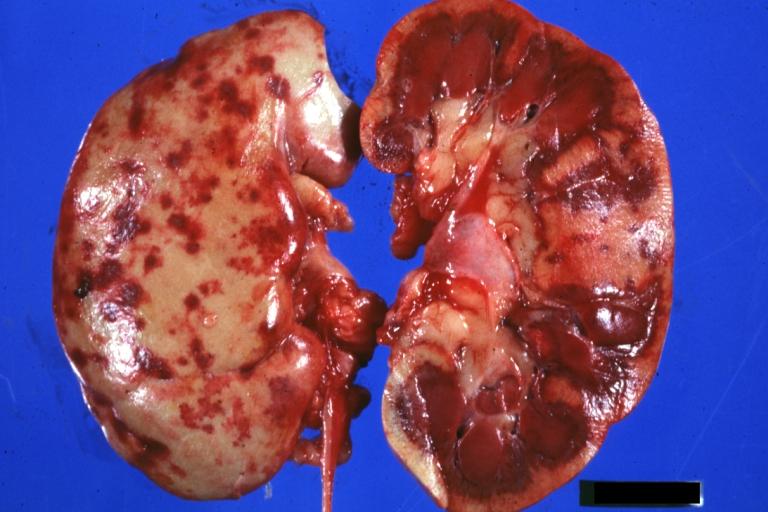
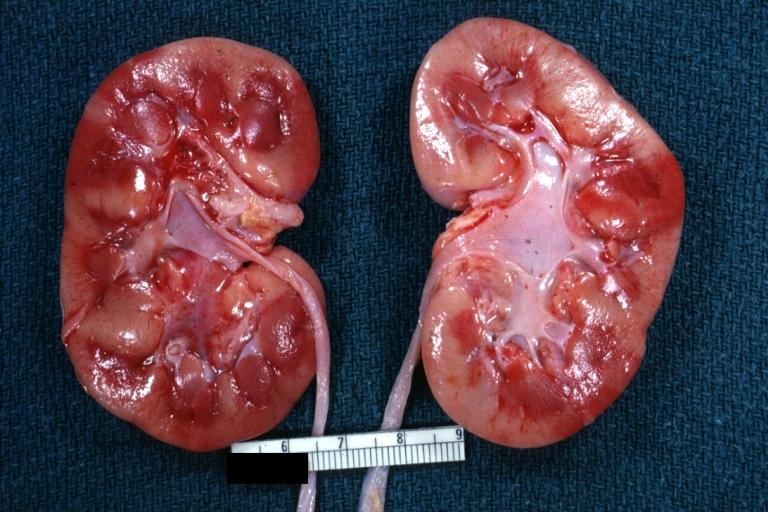
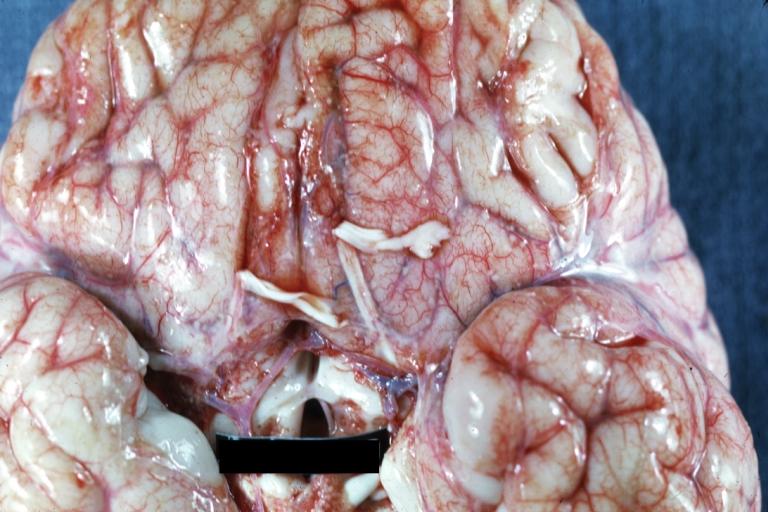
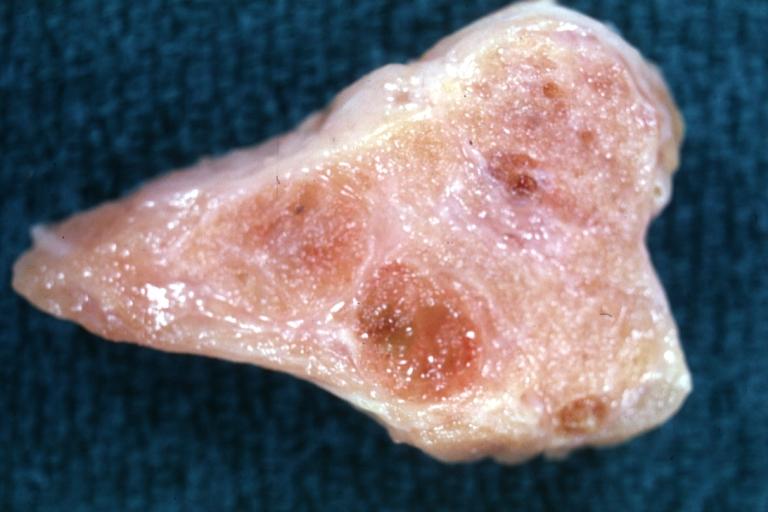
Gross Pathology
References
- ↑ Hettiaratchy S, Dziewulski P (2004) ABC of burns: pathophysiology and types of burns. BMJ 328 (7453):1427-9. DOI:10.1136/bmj.328.7453.1427 PMID: 15191982 PMID: 15191982
- ↑ "Pathophysiology and Current Management of Burn Injury : Advances in Skin & Wound Care".
- ↑ Rojas Y, Finnerty CC, Radhakrishnan RS, Herndon DN (December 2012). "Burns: an update on current pharmacotherapy". Expert Opin Pharmacother. 13 (17): 2485–94. doi:10.1517/14656566.2012.738195. PMC 3576016. PMID 23121414.
- ↑ "ABC of burns: Pathophysiology and types of burns".
- ↑ "Porth Pathophysiology: Concepts of Altered Health States - Charlotte Pooler - كتب Google".