Back pain: Difference between revisions
| Line 54: | Line 54: | ||
Direct bending to the ground without bending the knee causes severe impact on the lower back in pregnancy and in normal individuals, which leads to strain, especially in the lumbo-saccral region that in turn strains the multifidus. | Direct bending to the ground without bending the knee causes severe impact on the lower back in pregnancy and in normal individuals, which leads to strain, especially in the lumbo-saccral region that in turn strains the multifidus. | ||
===Treatments with uncertain or doubtful benefit=== | ===Treatments with uncertain or doubtful benefit=== | ||
Revision as of 21:43, 23 August 2012
For patient information click here
| Back pain | |
 | |
|---|---|
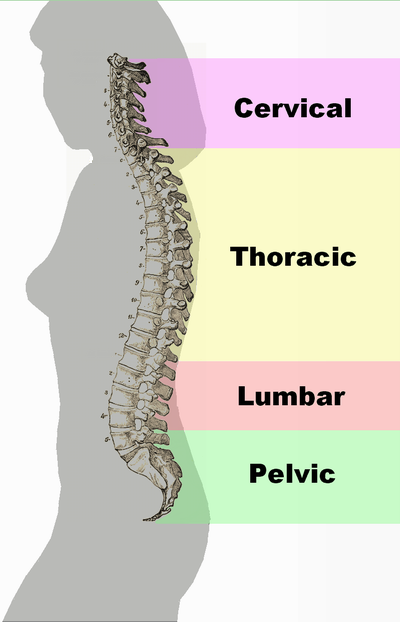
| Different regions (curvatures) of the vertebral column | |
| ICD-10 | M54 |
| ICD-9 | 724.5 |
| DiseasesDB | 15544 |
| MeSH | D001416 |
|
Back pain Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Lecture |
|
Case Studies |
|
Back pain On the Web |
|
American Roentgen Ray Society Images of Back pain |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Robert G. Schwartz, M.D. [2], Piedmont Physical Medicine and Rehabilitation, P.A.; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [3], M.Umer Tariq [4]
Synonyms and keywords: Lumbago; backache; dorsalgia
Associated conditions
Back pain can be a sign of a serious medical problem, although this is not most frequently the underlying cause:
- Typical warning signs of a potentially life-threatening problem are bowel and/or bladder incontinence or progressive weakness in the legs. Patients with these symptoms should seek immediate medical care.
- Severe back pain (such as pain that is bad enough to interrupt sleep) that occurs with other signs of severe illness (e.g. fever, unexplained weight loss) may also indicate a serious underlying medical condition, such as cancer.
- Back pain that occurs after a trauma, such as a car accident or fall, should also be promptly evaluated by a medical professional to check for a fracture or other injury.
- Back pain in individuals with medical conditions that put them at high risk for a spinal fracture, such as osteoporosis or multiple myeloma, also warrants prompt medical attention.
In general, however, back pain does not usually require immediate medical intervention. The vast majority of episodes of back pain are self-limiting and non-progressive. Most back pain syndromes are due to inflammation, especially in the acute phase, which typically lasts for two weeks to three months.
A few observational studies suggest that two common diagnoses of back pain, lumbar disc herniation or degenerative disc disease may not be more prevalent among those in pain than among the general population and that the mechanisms by which these conditions might cause pain are not known.[1][2][3][4] Other studies suggest that for as many as 85% of cases, no physiological cause for the pain has been able to be specifically identified.[5][6]
A few studies suggest that psychosocial factors such as on-the-job stress and dysfunctional family relationships may correlate more closely with back pain than structural abnormalities revealed in x-rays and other medical imaging scans.[7][8][9][10]
Underlying causes
Transient back pain is likely one of the first symptoms of influenza.
Muscle strains (pulled muscles) are commonly identified as the cause of back pain, as are muscle imbalances. Pain from such an injury often remains as long as the muscle imbalances persist. The muscle imbalances cause a mechanical problem with the skeleton, building up pressure at points along the spine, which causes the pain. Ligament strain is a very common cause of back pain as well [5].
Another cause of acute low back pain is a Meniscoid Occlusion. The more mobile regions of the spine have invaginations of the synovial membrane that act as a cushion to help the bones move over each other smoothly. The synovial membrane is well supplied with blood and nerves. When it becomes pinched or trapped it can cause sudden severe pain. The pinching causes the membrane to become inflamed, causing greater pressure and ongoing pain. Symptoms include severe low back pain that may be accompanied by muscle spasm, pain with walking, concentration of pain to one side, and no radiculopathy (radiating pain down buttock and leg). Relief should be felt with flexion (bending forward),and exacerbated with extension (bending backward).
When back pain lasts more than three months, or if there is more radicular pain (sciatica) than back pain, a more specific diagnosis can usually be made. There are several common causes of back pain: for adults under age 50, these include ligament strain, nerve root irritation, spinal disc herniation and degenerative disc disease or isthmic spondylolisthesis; in adults over age 50, common causes also include osteoarthritis (degenerative joint disease) and spinal stenosis [6],trauma, cancer, infection, fractures, and inflammatory disease [7]. Non-anatomical factors can also contribute to or cause back pain, such as stress, repressed anger,[8] or depression. Even if there is an anatomical cause for the pain, if depression is present it should also be treated concurrently.
New attention has been focused on non-discogenic back pain, where patients have normal or near-normal MRI and CT scans. One of the newer investigations looks into the role of the dorsal ramus in patient's pain that have normal radiographic evidence. See Posterior Rami Syndrome. Diagnostic musculoskeletal ultrasonography has been shown to be helpful in objectifying multifidus atropy.
Back Pain During Pregnancy
About 50% of women experience low back pain during pregnancy.[11]
Back pain in pregnancy may be severe enough to cause significant pain and disability and pre-dispose patients to back pain in a following pregnancy. No significant increased risk of back pain with pregnancy has been found with respect to maternal weight gain, exercise, work satisfaction, or pregnancy outcome factors such as birth weight, birth length, and Apgar scores.
Biomechanical factors of pregnancy that are shown to be associated with low back pain of pregnancy include abdominal sagittal and transverse diameter and the depth of lumbar lordosis. Typical factors aggravating the back pain of pregnancy include standing, sitting, forward bending, lifting, and walking. Back pain in pregnancy may also be characterized by pain radiating into the thigh and buttocks, night-time pain severe enough to wake the patient, pain that is increased during the night-time, or pain that is increased during the day-time.
The avoidance of high impact, weight-bearing activities and especially those that asymmetrically load the involved structures such as: extensive twisting with lifting, single-leg stance postures, stair climbing, and repetitive motions at or near the end-ranges of back or hip motion can ease the pain.
Direct bending to the ground without bending the knee causes severe impact on the lower back in pregnancy and in normal individuals, which leads to strain, especially in the lumbo-saccral region that in turn strains the multifidus.
Treatments with uncertain or doubtful benefit
- While some citations report limited benefit from Injections, such as epidural steroid injections, facet joint injections, or prolotherapy they still enjoy considerable support among the majority of patients and clinicians.[12][13] Arguments against those citations with negative outcomes include the extreme difficulty in finding literature that has consistent and clearly defined patient populations while accounting for the multifactoral nature of back pain.
- Cold compression therapy is advocated for a strained back or chronic back pain and is postulated to reduce pain and inflammation, especially after strenuous exercise such as golf, gardening, or lifting. However, a meta-analysis of randomized controlled trials by the Cochrane Collaboration concluded "The evidence for the application of cold treatment to low-back pain is even more limited, with only three poor quality studies located. No conclusions can be drawn about the use of cold for low-back pain"[14] Despite this, cryotherapy is inexpensive, easily tolerated and been used with high success for decades in patients with numerous kinds of musculoskeletal conditions.
- Bed rest is rarely recommended as it can exacerbate symptoms,[15] and when necessary is usually limited to one or two days. Prolonged bed rest or inactivity is actually counterproductive, as the resulting stiffness leads to more pain.
- Electrotherapy, such as a Transcutaneous Electrical Nerve Stimulator (TENS) has been proposed. Two randomized controlled trials found conflicting results.[16][17] Despite the fact the the article by Walsh NE made use of "sham TENS" (essentially a TENS unit that could not be felt compared to a second unit that was off) the expected negative outcome study results have been cited by the Cochrane Collaboration to conclude that there is inconsistent evidence to support use of TENS.[18] In addition, spinal cord stimulation (SCS), where an electrical device is used to interrupt the pain signals being sent to the brain and has been studied for various underlying causes of back pain. While SCS still enjoys limited acceptance, it is expensive, requires lifelong monitoring and is not without complication.
- Inversion therapy may be useful for temporary back relief due to the traction method or spreading of the back vertebra's through (in this case) gravity. The patient hangs in an upside down position for a period of time from ankles or knees until this separation occurs. The effect can be achieved without a complete vertical hang (90 degree) and noticeable benefits can be observed at angles as low as 10 to 45 degrees.
Differential Diagnosis
In alphabetical order. [19] [20]
Common Causes
- Discopathy
- Idiopathic lumbago
- Trauma due to lifting
- Ligament strain
- Radiculopathy
- Posterior Rami Syndrome
Complete Differential Diagnosis of the Causes of Back pain
(In alphabetical order)
Complete Differential Diagnosis of the Causes of Back pain
(By organ system)
Prognosis
Most patients with back pain recover without residual functional loss, but individuals should contact a doctor if there is not a noticeable reduction in pain and inflammation after 72 hours of self-care. Recurring back pain resulting from improper body mechanics or other nontraumatic causes is often preventable. Engaging in exercises that don't jolt or strain the back, maintaining correct posture, and lifting objects properly can help prevent injuries. Many work-related injuries are caused or aggravated by stressors such as heavy lifting, vibration, repetitive motion, and awkward posture. Applying ergonomic principles — designing furniture and tools to protect the body from injury — at home and in the workplace can greatly reduce the risk of back injury and help maintain a healthy back.
See also
- Failed back syndrome
- Low back pain
- Posterior Rami Syndrome
- Tension myositis syndrome
- Upper back pain
- Pregnancy related pelvic girdle pain
References
- ↑ Borenstein DG, O'Mara JW, Boden SD; et al. (2001). "The value of magnetic resonance imaging of the lumbar spine to predict low-back pain in asymptomatic subjects : a seven-year follow-up study". The Journal of bone and joint surgery. American volume. 83-A (9): 1306–11. PMID 11568190.
- ↑ Savage RA, Whitehouse GH, Roberts N (1997). "The relationship between the magnetic resonance imaging appearance of the lumbar spine and low back pain, age and occupation in males". European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 6 (2): 106–14. PMID 9209878.
- ↑ Jensen MC, Brant-Zawadzki MN, Obuchowski N, Modic MT, Malkasian D, Ross JS (1994). "Magnetic resonance imaging of the lumbar spine in people without back pain". N. Engl. J. Med. 331 (2): 69–73. PMID 8208267.
- ↑ Kleinstück F, Dvorak J, Mannion AF (2006). "Are "structural abnormalities" on magnetic resonance imaging a contraindication to the successful conservative treatment of chronic nonspecific low back pain?". Spine. 31 (19): 2250–7. doi:10.1097/01.brs.0000232802.95773.89. PMID 16946663.
- ↑ White AA, Gordon SL (1982). "Synopsis: workshop on idiopathic low-back pain". Spine. 7 (2): 141–9. PMID 6211779.
- ↑ van den Bosch MA, Hollingworth W, Kinmonth AL, Dixon AK (2004). "Evidence against the use of lumbar spine radiography for low back pain". Clinical radiology. 59 (1): 69–76. PMID 14697378.
- ↑ Burton AK, Tillotson KM, Main CJ, Hollis S (1995). "Psychosocial predictors of outcome in acute and subchronic low back trouble". Spine. 20 (6): 722–8. PMID 7604349.
- ↑ Carragee EJ, Alamin TF, Miller JL, Carragee JM (2005). "Discographic, MRI and psychosocial determinants of low back pain disability and remission: a prospective study in subjects with benign persistent back pain". The spine journal : official journal of the North American Spine Society. 5 (1): 24–35. doi:10.1016/j.spinee.2004.05.250. PMID 15653082.
- ↑ Hurwitz EL, Morgenstern H, Yu F (2003). "Cross-sectional and longitudinal associations of low-back pain and related disability with psychological distress among patients enrolled in the UCLA Low-Back Pain Study". Journal of clinical epidemiology. 56 (5): 463–71. PMID 12812821.
- ↑ Dionne CE (2005). "Psychological distress confirmed as predictor of long-term back-related functional limitations in primary care settings". Journal of clinical epidemiology. 58 (7): 714–8. doi:10.1016/j.jclinepi.2004.12.005. PMID 15939223.
- ↑ Ostgaard HC, Andersson GBJ, Karlsson K. Prevalence of back pain in pregnancy. Spine 1991;16:549-52.
- ↑ Nelemans P, de Bie R, de Vet H, Sturmans F. "Injection therapy for subacute and chronic benign low back pain". Cochrane Database Syst Rev: CD001824. PMID 10796449.
- ↑ Yelland M, Mar C, Pirozzo S, Schoene M, Vercoe P. "Prolotherapy injections for chronic low-back pain". Cochrane Database Syst Rev: CD004059. PMID 15106234.
- ↑ French S, Cameron M, Walker B, Reggars J, Esterman A (2006). "A Cochrane review of superficial heat or cold for low back pain". Spine. 31 (9): 998–1006. PMID 16641776.
- ↑ Hagen K, Hilde G, Jamtvedt G, Winnem M. "Bed rest for acute low-back pain and sciatica". Cochrane Database Syst Rev: CD001254. PMID 15495012.
- ↑ Cheing GL, Hui-Chan CW (1999). "Transcutaneous electrical nerve stimulation: nonparallel antinociceptive effects on chronic clinical pain and acute experimental pain". Archives of physical medicine and rehabilitation. 80 (3): 305–12. PMID 10084439.
- ↑ Deyo RA, Walsh NE, Martin DC, Schoenfeld LS, Ramamurthy S (1990). "A controlled trial of transcutaneous electrical nerve stimulation (TENS) and exercise for chronic low back pain". N. Engl. J. Med. 322 (23): 1627–34. PMID 2140432.
- ↑ Khadilkar A, Milne S, Brosseau L; et al. (2005). "Transcutaneous electrical nerve stimulation (TENS) for chronic low-back pain". Cochrane database of systematic reviews (Online) (3): CD003008. doi:10.1002/14651858.CD003008.pub2. PMID 16034883.
- ↑ Sailer, Christian, Wasner, Susanne. Differential Diagnosis Pocket. Hermosa Beach, CA: Borm Bruckmeir Publishing LLC, 2002:77 ISBN 1591032016
- ↑ Kahan, Scott, Smith, Ellen G. In A Page: Signs and Symptoms. Malden, Massachusetts: Blackwell Publishing, 2004:68 ISBN 140510368X
External links
- Back Pain - Information for Patients
- Back pain at the Open Directory Project
- Template:NINDS
- Handout on Health: Back Pain at National Institute of Arthritis and Musculoskeletal and Skin Diseases
- Back Pain Information for Patients: Spine-health.com
- Patient's guide to back pain
- Back pain, on Medline plus, a service of the National Library of Medicine
Template:Diseases of the musculoskeletal system and connective tissue
de:Rückenschmerzen it:Dorsopatia nl:Rugpijn simple:back pain