Aortic dissection CT: Difference between revisions
No edit summary |
No edit summary |
||
| Line 56: | Line 56: | ||
| bgcolor="LightGreen" |1. In patients with aortic root/ascending aortic aneurysms or aortic dissection, obtaining a multigenerational family history of TAD, unexplained sudden deaths, and peripheral and intracranial aneurysms is recommended''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: B-NR]])'' | | bgcolor="LightGreen" |1. In patients with aortic root/ascending aortic aneurysms or aortic dissection, obtaining a multigenerational family history of TAD, unexplained sudden deaths, and peripheral and intracranial aneurysms is recommended''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: B-NR]])'' | ||
2. In patients with aortic root/ascending aortic aneurysms or aortic dissection and risk factors for HTAD (Table 8, Figure 17), genetic testing to identify pathogenic/likely pathogenic variants (ie, mutations) is recommended''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: B-NR]])'' | 2. In patients with aortic root/ascending aortic aneurysms or aortic dissection and risk factors for HTAD (Table 8, Figure 17), genetic testing to identify pathogenic/likely pathogenic variants (ie, mutations) is recommended''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: B-NR]])'' | ||
3. In patients with an established pathogenic or likely pathogenic variant in a gene predisposing to HTAD, it is recommended that genetic counseling be provided and the patient’s clinical management be informed by the specific gene and variant in the gene''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: B-NR]])'' | 3. In patients with an established pathogenic or likely pathogenic variant in a gene predisposing to HTAD, it is recommended that genetic counseling be provided and the patient’s clinical management be informed by the specific gene and variant in the gene''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: B-NR]])'' | ||
4. In patients with TAD who have a pathogenic/likely pathogenic variant, genetic testing of at-risk biological relatives (ie, cascade testing) is recommended.6,10,11 In family members who are found by genetic screening to have inherited the pathogenic/likely pathogenic variant, aortic imaging with TTE (if aortic root and ascending aorta are adequately visualized, otherwise with CT or MRI) is recommended.''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: B-NR]])'' | 4. In patients with TAD who have a pathogenic/likely pathogenic variant, genetic testing of at-risk biological relatives (ie, cascade testing) is recommended.6,10,11 In family members who are found by genetic screening to have inherited the pathogenic/likely pathogenic variant, aortic imaging with TTE (if aortic root and ascending aorta are adequately visualized, otherwise with CT or MRI) is recommended.''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: B-NR]])'' | ||
5. In a family with aortic root/ascending aortic aneurysms or aortic dissection, if the disease-causing variant is not identified with genetic testing, screening aortic imaging (as per recommendation 4) of at-risk biological relatives (ie, cascade testing) is recommended.''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: B-NR]])'' | 5. In a family with aortic root/ascending aortic aneurysms or aortic dissection, if the disease-causing variant is not identified with genetic testing, screening aortic imaging (as per recommendation 4) of at-risk biological relatives (ie, cascade testing) is recommended.''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: B-NR]])'' | ||
6. In patients with aortic root/ascending aortic aneurysms or aortic dissection, in the absence of either a known family history of TAD or pathogenic/likely pathogenic variant, screening aortic imaging (as per recommendation 4) of first-degree relatives is recommended.''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: C-LD]])'' | 6. In patients with aortic root/ascending aortic aneurysms or aortic dissection, in the absence of either a known family history of TAD or pathogenic/likely pathogenic variant, screening aortic imaging (as per recommendation 4) of first-degree relatives is recommended.''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: C-LD]])'' | ||
7. In patients with acute type A aortic dissection, the diameter of the aortic root and ascending aorta should be recorded in the operative note and medical record to inform the management of affected relatives.''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: C-EO]])'' | |||
7. In patients with acute type A aortic dissection, the diameter of the aortic root and ascending aorta should be recorded in the operative note and medical record to inform the management of affected relatives.''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: C-EO]])'' | |||
|} | |} | ||
Revision as of 20:01, 2 December 2022
|
Aortic dissection Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Special Scenarios |
|
Case Studies |
|
|
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Cafer Zorkun, M.D., Ph.D. [2]; Aarti Narayan, M.B.B.S [3]; Raviteja Guddeti, M.B.B.S. [4] Sahar Memar Montazerin, M.D.[5]
Overview
A CT scan can be used to diagnose aortic dissection if neither a TEE nor MRI is available in a timely fashion, or if there is a contraindication to their performance. An example would be after hours in an emergency room setting. If the results of the CT scan are non-diagnostic, then TEE or MRI should be performed to confirm the diagnosis.
CT
Computed Tomography Angiography (CTA)
- Computed tomography angiography is a fast non-invasive test that will give an accurate three-dimensional view of the aorta. These images are produced by taking rapid thin cut slices of the chest and abdomen, and combining them in the computer to create cross-sectional slices.
- In order to delineate the aorta to the accuracy necessary to make the proper diagnosis, an iodinated contrast material is injected into a peripheral vein. Contrast is injected and the scan performed using a Bolus Tracking method. This is a type of scan timed to an injection, in order to capture the contrast as it enters the aorta.
- The scan will then follow the contrast as it flows though the vessel.
Differentiating a True Lumen from a False Lumen
- Beak sign: In the false lumen, there will be an acute angle between the dissection flap and the arterial wall.
- Aortic cobwebs: In the false lumen, there may be fibroelastic bands.
- Size: False lumen is usually larger than the true lumen.
- Displaced intimal calcification: Usually faces the true lumen.
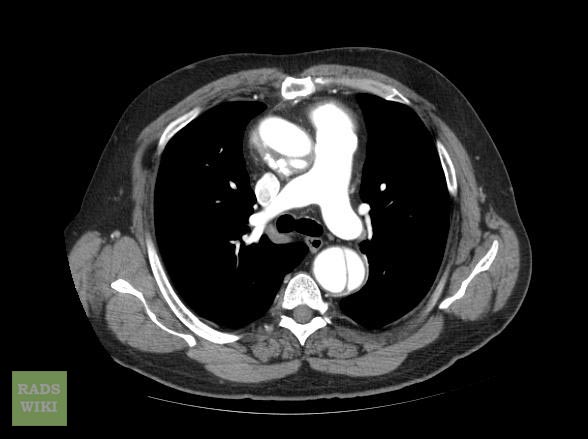
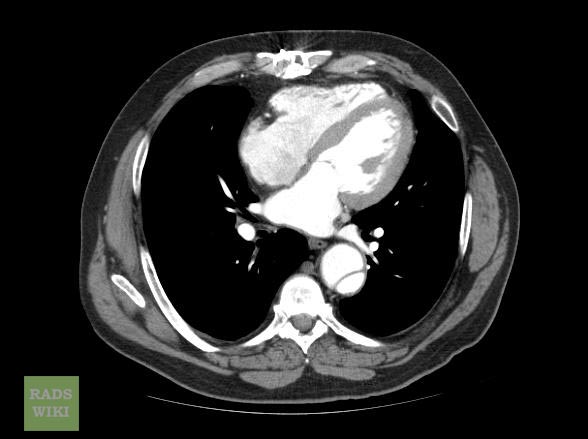
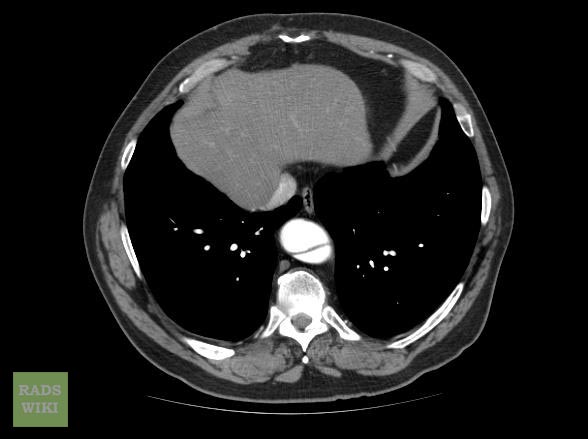
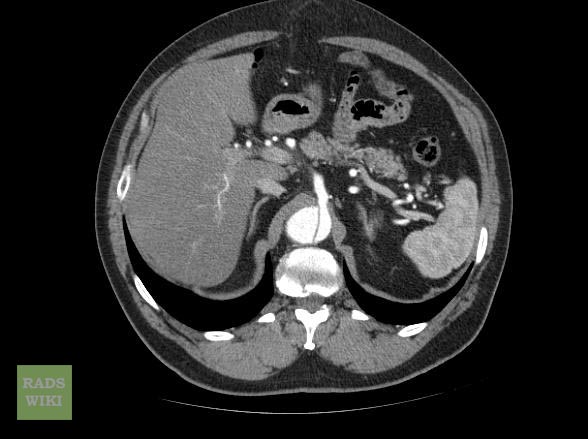
CT Examples of Aortic dissection
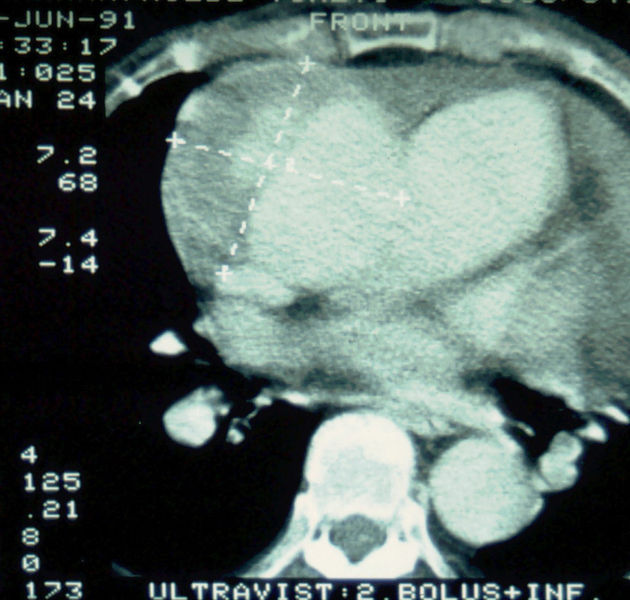
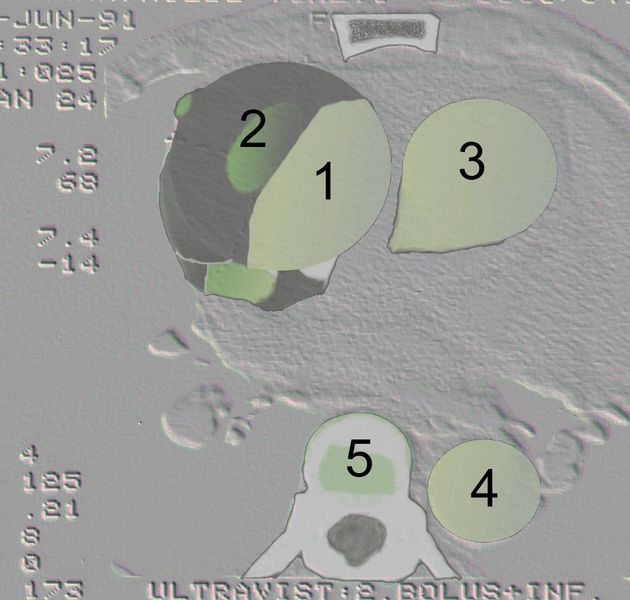
Type A Dissection
-
Aortic dissection Type Stanford A
-
Aortic dissection Type Stanford A - '1 Aorta ascendens, true Lumen - 2 false lumen - 3 Pulmonary artery - 4 Aorta descendens - 5 thoracic vertebra
-
Another example of Stanford A type dissection[1]
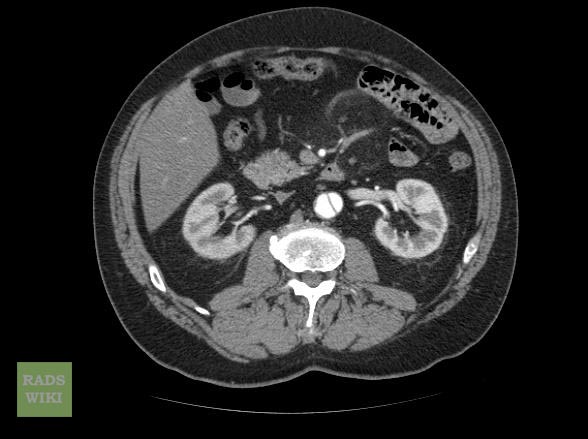
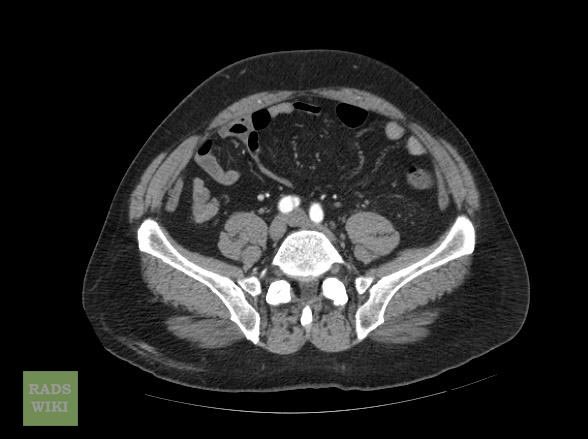
Type B Dissection
2022ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM Guidelines for the Diagnosis and Management of Patients with Thoracic Aortic Disease[4]
Screening Tests
| Class I |
| 1. In patients with aortic root/ascending aortic aneurysms or aortic dissection, obtaining a multigenerational family history of TAD, unexplained sudden deaths, and peripheral and intracranial aneurysms is recommended(Level of Evidence: B-NR)
2. In patients with aortic root/ascending aortic aneurysms or aortic dissection and risk factors for HTAD (Table 8, Figure 17), genetic testing to identify pathogenic/likely pathogenic variants (ie, mutations) is recommended(Level of Evidence: B-NR) 3. In patients with an established pathogenic or likely pathogenic variant in a gene predisposing to HTAD, it is recommended that genetic counseling be provided and the patient’s clinical management be informed by the specific gene and variant in the gene(Level of Evidence: B-NR) 4. In patients with TAD who have a pathogenic/likely pathogenic variant, genetic testing of at-risk biological relatives (ie, cascade testing) is recommended.6,10,11 In family members who are found by genetic screening to have inherited the pathogenic/likely pathogenic variant, aortic imaging with TTE (if aortic root and ascending aorta are adequately visualized, otherwise with CT or MRI) is recommended.(Level of Evidence: B-NR) 5. In a family with aortic root/ascending aortic aneurysms or aortic dissection, if the disease-causing variant is not identified with genetic testing, screening aortic imaging (as per recommendation 4) of at-risk biological relatives (ie, cascade testing) is recommended.(Level of Evidence: B-NR) 6. In patients with aortic root/ascending aortic aneurysms or aortic dissection, in the absence of either a known family history of TAD or pathogenic/likely pathogenic variant, screening aortic imaging (as per recommendation 4) of first-degree relatives is recommended.(Level of Evidence: C-LD) 7. In patients with acute type A aortic dissection, the diameter of the aortic root and ascending aorta should be recorded in the operative note and medical record to inform the management of affected relatives.(Level of Evidence: C-EO) |
2014 ESC Guidelines on the Diagnosis and Treatment of Aortic Diseases (DO NOT EDIT)[5]
Diagnostic Value of Computed Tomography in Aortic Dissection
| Class I |
| "In unstabled patients with a suspicion of AAS, the following imaging modalities are recommended according to local availability and expertise:transoesophageal echocardiography; CT scan.(Level of Evidence: C)" |
| "In stable patients with a suspicion of AAS, the following imaging modalities are recommended (or should be considered) according to local availability and expertise:CT scan; MRI.(Level of Evidence: C)" |
Follow-up Imaging study
| Class I |
| "In case of initially negative imaging with persistence of suspicion of AAS, repetitive imaging (CT or MRI) is recommended.(Level of Evidence: C)" |
| "In case of uncomplicated Type B AD treated medically, repeated imaging (CT or MRI) during the first days is recommended. (Level of Evidence: C)" |
2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM Guidelines for the Diagnosis and Management of Patients with Thoracic Aortic Disease (DO NOT EDIT) [6]
Screening Tests (DO NOT EDIT)[6]
| Class I |
| "1. Urgent and definitive imaging of the aorta using transesophageal echocardiogram, computed tomographic imaging, or magnetic resonance imaging is recommended to identify or exclude thoracic aortic dissection in patients at high risk for the disease by initial screening. (Level of Evidence: B)" |
Determining the Presence and Measuring the Progression of Thoracic Aortic Disease (DO NOT EDIT)[6]
| Class I |
| "1. For measurements taken by computed tomographic imaging or magnetic resonance imaging, the external diameter should be measured perpendicular to the axis of blood flow. For aortic root measurements, the widest diameter, typically at the mid-sinus level, should be used. (Level of Evidence: C)" |
Takayasu Arteritis and Giant Cell Arteritis (DO NOT EDIT) [6]
| Class I |
| "1. The initial evaluation of Takayasu arteritis or giant cell arteritis should include thoracic aorta and branch vessel computed tomographic imaging or magnetic resonance imaging to investigate the possibility of aneurysm or occlusive disease in these vessels. (Level of Evidence: C)" |
Surveillance of Thoracic Aortic Disease or Previously Repaired Patients (DO NOT EDIT)[6]
| Class IIa |
| "1. Computed tomographic imaging or magnetic resonance imaging of the thoracic aorta is reasonable after a Type A or B aortic dissection or after prophylactic repair of the aortic root/ ascending aorta. (Level of Evidence: C)" |
| "2. Computed tomographic imaging or magnetic resonance imaging of the aorta is reasonable at 1, 3, 6, and 12 months postdissection and, if stable, annually thereafter so that any threatening enlargement can be detected in a timely fashion. (Level of Evidence: C)" |
| "3. When following patients with imaging, utilization of the same modality at the same institution is reasonable, so that similar images of matching anatomic segments can be compared side by side. (Level of Evidence: C)" |
| "4. Surveillance imaging similar to classic aortic dissection is reasonable in patients with intramural hematoma. (Level of Evidence: C)" |
References
- ↑ Case courtesy of A.Prof Frank Gaillard, Radiopaedia.org, rID: 8886
- ↑ Case courtesy of Dr Craig Hacking, Radiopaedia.org, rID: 34693
- ↑ Case courtesy of Prof Cláudio Souza, Radiopaedia.org, rID: 13783
- ↑ Isselbacher EM, Preventza O, Black JH, Augoustides JG, Beck AW, Bolen MA; et al. (2022). "2022 ACC/AHA Guideline for the Diagnosis and Management of Aortic Disease: A Report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines". Circulation. doi:10.1161/CIR.0000000000001106. PMID 36322642 Check
|pmid=value (help). - ↑ Erbel R, Aboyans V, Boileau C, Bossone E, Bartolomeo RD, Eggebrecht H, Evangelista A, Falk V, Frank H, Gaemperli O, Grabenwöger M, Haverich A, Iung B, Manolis AJ, Meijboom F, Nienaber CA, Roffi M, Rousseau H, Sechtem U, Sirnes PA, Allmen RS, Vrints CJ (November 2014). "2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: Document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC)". Eur. Heart J. 35 (41): 2873–926. doi:10.1093/eurheartj/ehu281. PMID 25173340.
- ↑ 6.0 6.1 6.2 6.3 6.4 Hiratzka LF, Bakris GL, Beckman JA; et al. (2010). "2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with Thoracic Aortic Disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine". Circulation. 121 (13): e266–369. doi:10.1161/CIR.0b013e3181d4739e. PMID 20233780. Unknown parameter
|month=ignored (help)
![Another example of Stanford A type dissection[1]](/images/b/be/Type-a-dissection-ct.jpg)
![Aortic dissection Type Stanford A[2]](/images/e/eb/Type-a-aortic-dissection-4.png)
![[3]](/images/5/5f/Aortic-dissection-debakey-type-1.jpg)