Alexander disease: Difference between revisions
Irfan Dotani (talk | contribs) No edit summary |
MoisesRomo (talk | contribs) No edit summary |
||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{SI}} | {{SI}} | ||
{{CMG}}; {{AE}} | {{CMG}}; {{AE}}[[User:MoisesRomo|Moises Romo M.D.]] | ||
'''''Synonyms and keywords:''''' [[Dysmyelogenic leukodystrophy]], [[Dysmyelogenic leukodystrophy-megalobare]], [[Fibrinoid degeneration of astrocytes]], [[Fibrinoid leukodystrophy]], [[Hyaline panneuropathy]], [[Leukodystrophy with Rosenthal fibers]], [[Megalencephaly with hyaline inclusion]], [[Megalencephaly with hyaline panneuropathy]] | '''''Synonyms and keywords:''''' [[Dysmyelogenic leukodystrophy]], [[Dysmyelogenic leukodystrophy-megalobare]], [[Fibrinoid degeneration of astrocytes]], [[Fibrinoid leukodystrophy]], [[Hyaline panneuropathy]], [[Leukodystrophy with Rosenthal fibers]], [[Megalencephaly with hyaline inclusion]], [[Megalencephaly with hyaline panneuropathy]] | ||
| Line 16: | Line 16: | ||
==Historical Perspective== | ==Historical Perspective== | ||
* Alexander disease was first described in 1949 by the New Zealand pathologist William Alexander in London, England under his paper "Progressive Fibrinoid degeneration of fibrillary astrocytes associated with mental retardation in a hydrocephalic infant", where he reported a case of a 16-month old child who died after presenting a history of increasing macrocephaly and developmental delay.<ref name="pmid29478608">{{cite journal |vauthors=Messing A |title=Alexander disease |journal=Handb Clin Neurol |volume=148 |issue= |pages=693–700 |date=2018 |pmid=29478608 |doi=10.1016/B978-0-444-64076-5.00044-2 |url=}}</ref> | |||
* By the decade of 1960´s, the presence of Rosenthal fibers accompanied by progressive neurologic imapairment was recognized as a hallmark of patients with Alexander disease.<ref name="Seil1968">{{cite journal|last1=Seil|first1=Fredrick J.|title=Alexander's Disease in an Adult|journal=Archives of Neurology|volume=19|issue=5|year=1968|pages=494|issn=0003-9942|doi=10.1001/archneur.1968.00480050064006}}</ref><ref name="pmid29478608" /><ref name="BalbiSalvini2010">{{cite journal|last1=Balbi|first1=Pietro|last2=Salvini|first2=Silvana|last3=Fundarò|first3=Cira|last4=Frazzitta|first4=Giuseppe|last5=Maestri|first5=Roberto|last6=Mosah|first6=Dibo|last7=Uggetti|first7=Carla|last8=Sechi|first8=GianPietro|title=The clinical spectrum of late-onset Alexander disease: a systematic literature review|journal=Journal of Neurology|volume=257|issue=12|year=2010|pages=1955–1962|issn=0340-5354|doi=10.1007/s00415-010-5706-1}}</ref> | |||
* In 2001, Brenner et. al discovered that mutations in GFAP encoding for glial fibrillary acidic protein, could be the causant of most of the cases of Alexander disease.<ref name="BrennerLampel1990">{{cite journal|last1=Brenner|first1=Michael|last2=Lampel|first2=Keith|last3=Nakatani|first3=Yoshihiro|last4=Mill|first4=John|last5=Banner|first5=Carl|last6=Mearow|first6=Karen|last7=Dohadwala|first7=Mariam|last8=Lipsky|first8=Robert|last9=Freese|first9=Ernst|title=Characterization of human cDNA and genomic clones for glial fibrillary acidic protein|journal=Molecular Brain Research|volume=7|issue=4|year=1990|pages=277–286|issn=0169328X|doi=10.1016/0169-328X(90)90078-R}}</ref><ref name="pmid29478608" /> | |||
==Classification== | ==Classification== | ||
Revision as of 18:30, 25 July 2020
|
WikiDoc Resources for Alexander disease |
|
Articles |
|---|
|
Most recent articles on Alexander disease Most cited articles on Alexander disease |
|
Media |
|
Powerpoint slides on Alexander disease |
|
Evidence Based Medicine |
|
Cochrane Collaboration on Alexander disease |
|
Clinical Trials |
|
Ongoing Trials on Alexander disease at Clinical Trials.gov Trial results on Alexander disease Clinical Trials on Alexander disease at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Alexander disease NICE Guidance on Alexander disease
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Alexander disease Discussion groups on Alexander disease Patient Handouts on Alexander disease Directions to Hospitals Treating Alexander disease Risk calculators and risk factors for Alexander disease
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Alexander disease |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Moises Romo M.D.
Synonyms and keywords: Dysmyelogenic leukodystrophy, Dysmyelogenic leukodystrophy-megalobare, Fibrinoid degeneration of astrocytes, Fibrinoid leukodystrophy, Hyaline panneuropathy, Leukodystrophy with Rosenthal fibers, Megalencephaly with hyaline inclusion, Megalencephaly with hyaline panneuropathy
Template:DiseaseDisorder infobox
Overview
Alexander disease is a slowly progressing and fatal neurodegenerative disease. It is a very rare disorder which results from a genetic mutation and mostly affects infants and children, causing developmental delay and changes in physical characteristics.
Historical Perspective
- Alexander disease was first described in 1949 by the New Zealand pathologist William Alexander in London, England under his paper "Progressive Fibrinoid degeneration of fibrillary astrocytes associated with mental retardation in a hydrocephalic infant", where he reported a case of a 16-month old child who died after presenting a history of increasing macrocephaly and developmental delay.[1]
- By the decade of 1960´s, the presence of Rosenthal fibers accompanied by progressive neurologic imapairment was recognized as a hallmark of patients with Alexander disease.[2][1][3]
- In 2001, Brenner et. al discovered that mutations in GFAP encoding for glial fibrillary acidic protein, could be the causant of most of the cases of Alexander disease.[4][1]
Classification
Pathophysiology
The cause of Alexander disease is a mutation in the gene encoding glial fibrillary acidic protein.
Alexander disease belongs to leukodystrophies, a group of diseases which affect growth or development of the myelin sheath. The destruction of white matter in the brain is accompanied by the formation of fibrous, eosinophilic deposits known as Rosenthal fibers.
Genetics
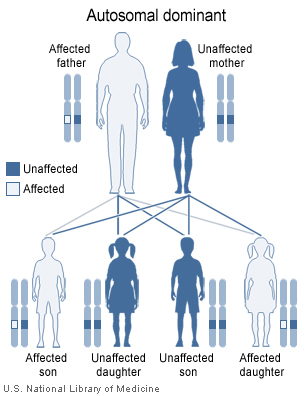
Alexander disease is a genetic disorder affecting the central nervous system (midbrain and cerebellum). It is caused by mutations in the gene for glial fibrillary acidic protein (GFAP) that maps to chromosome 17q21. It is inherited in an autosomal dominant manner.
Causes
Differentiating Alexander disease from Other Diseases
Epidemiology and Demographics
This is a very rare with no more than 300 cases reported. The infantile form (80% of all cases) starts usually at the age of six months or within the first two years. The average duration of the infantile form of the illness is usually about 3 years. Onset of the juvenile form (14% of all cases) presents usually between four to ten years of age. Duration of this form is in most cases about 8 years. In younger patients, seizures, megalencephaly, developmental delay, and spasticity are usually present. Neonatal onset is also reported. Onset in adults is least frequent. In older patients, bulbar or pseudobulbar symptoms and spasticity predominate. Symptoms of the adult form may also resemble multiple sclerosis.
Risk Factors
Screening
Natural History, Complications and Prognosis
The prognosis is generally poor. With early onset, death usually occurs within 10 years after the onset of symptoms. Usually, the later the disease occurs, the slower its course is.
Diagnosis
Diagnostic Criteria
History and Symptoms
- Delays in development of some physical, psychological and behavioral skills
- Progressive enlargement of the head (macrocephaly)
- Seizures
- Spasticity
- Hydrocephalus
- Dementia
- Clumsy movements.
Physical Examination
Laboratory Findings
CT Findings
- Decreased density of white matter
- Frontal lobe predominance
- +/- Dilated lateral ventricles
Imaging Findings
Other Diagnostic Studies
Treatment
There is neither cure nor standard treatment for Alexander disease. All treatment is symptomatic and supportive, for example antibiotics for intercurrent infection and anticonvulsants for seizure control are usually used.
Medical Therapy
Surgery
Prevention
See also
External links
- alexander at NIH/UW GeneTests
- The Stennis Foundation - Registered charity committed to raising awareness and funds for Leukodystrophies research
- The Stennis Foundation's MySpace site
References
- ↑ 1.0 1.1 1.2 Messing A (2018). "Alexander disease". Handb Clin Neurol. 148: 693–700. doi:10.1016/B978-0-444-64076-5.00044-2. PMID 29478608.
- ↑ Seil, Fredrick J. (1968). "Alexander's Disease in an Adult". Archives of Neurology. 19 (5): 494. doi:10.1001/archneur.1968.00480050064006. ISSN 0003-9942.
- ↑ Balbi, Pietro; Salvini, Silvana; Fundarò, Cira; Frazzitta, Giuseppe; Maestri, Roberto; Mosah, Dibo; Uggetti, Carla; Sechi, GianPietro (2010). "The clinical spectrum of late-onset Alexander disease: a systematic literature review". Journal of Neurology. 257 (12): 1955–1962. doi:10.1007/s00415-010-5706-1. ISSN 0340-5354.
- ↑ Brenner, Michael; Lampel, Keith; Nakatani, Yoshihiro; Mill, John; Banner, Carl; Mearow, Karen; Dohadwala, Mariam; Lipsky, Robert; Freese, Ernst (1990). "Characterization of human cDNA and genomic clones for glial fibrillary acidic protein". Molecular Brain Research. 7 (4): 277–286. doi:10.1016/0169-328X(90)90078-R. ISSN 0169-328X.