Addison's disease
| Addison's disease | |
| ICD-10 | E27.1-E27.2 |
|---|---|
| ICD-9 | 255.4 |
| DiseasesDB | 222 |
| MedlinePlus | 000378 |
| MeSH | D000224 |
|
Addison's disease Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Addison's disease On the Web |
|
American Roentgen Ray Society Images of Addison's disease |
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Synonyms and keywords: Autoimmune adrenalitis; Addison disease, autoimmune; primary adrenal insufficiency; chronic adrenocortical insufficiency; adrenocortical hypofunction; hypocortisolism; hypocorticism
Overview
Epidemiology and Demographics
Pathophysiology
Causes
Diagnosis
Symptoms
The symptoms of adrenal insufficiency develop insidiously, usually begin gradually and it may take some time to be recognized. Some have marked cravings for salty foods due to the urinary losses of sodium. Characteristics of the disease are [1]
- Chronic, worsening fatigue
- Muscle weakness
- Loss of appetite
- Weight loss
- Headache
- Sweating
- Changes in mood and personality
- muscle pains
- joint
About 50 percent of the time, one will notice:
Clinical signs
On examination, the following may be noticed:[1]
- Low blood pressure that falls further when standing (orthostatic hypotension)
- Darkening (hyperpigmentation) of the skin, including areas not exposed to the sun; characteristic sites are skin creases (e.g. of the hands), nipples, and the inside of the cheek (buccal mucosa), also old scars may darken.
- Signs of conditions that often occur together with Addison's: goiter and vitiligo
Because the symptoms progress slowly, they are usually ignored until a stressful event like an illness or an accident causes them to become worse. This is called an addisonian crisis, or acute adrenal insufficiency. In most cases, symptoms are severe enough that patients seek medical treatment before a crisis occurs. However, in about 25 percent of patients, symptoms first appear during an addisonian crisis.
Addisonian crisis
An "Addisonian crisis" or "adrenal crisis" is a constellation of symptoms that indicate severe adrenal insufficiency. This may be the result of either previously undiagnosed Addison's disease, a disease process suddenly affecting adrenal function (such as adrenal hemorrhage), or an intercurrent problem (e.g. infection, trauma) in the setting of known Addison's disease. Additionally, this situation may develop in those on long-term oral glucocorticoids who have suddenly ceased taking their medication. It is also a concern in the setting of myxedema coma; thyroxine given in that setting without glucocorticoids may precipitate a crisis.
Untreated, an Addisonian crisis can be fatal. It is a medical emergency, usually requiring hospitalization. Characteristic symptoms are:[2]
- Sudden penetrating pain in the legs, lower back or abdomen
- Severe vomiting and diarrhea, resulting in dehydration
- Low blood pressure
- Loss of consciousness/Syncope
- Hypoglycemia
- Confusion, psychosis
- Convulsions
Laboratory Findings
A diagnosis of Addison's disease is made by laboratory tests. The aim of these tests is first to determine whether levels of cortisol are insufficient and then to establish the cause. X-ray exams of the adrenal and pituitary glands also are useful in helping to establish the cause. In its early stages, adrenal insufficiency can be difficult to diagnose. A review of a patient's medical history based on the symptoms, especially the dark tanning of the skin, will lead a doctor to suspect Addison's disease.
In suspected cases of Addison's disease, one needs to demonstrate that adrenal hormone levels are low even after appropriate stimulation with synthetic pituitary hormone tetracosactide. Two tests are performed, the short and the long test.
The short test compares blood cortisol levels before and after 250 micrograms of tetracosactide (IM/IV) is given. If, one hour later, plasma cortisol exceeds 170 nmol/L and has risen by at least 330 nmol/L to at least 690 nmol/L, adrenal failure is excluded. If the short test is abnormal, the long test is used to differentiate between primary adrenal failure and secondary adrenocortical failure.
The long test uses 1 mg tetracosactide (IM). Blood is taken 1, 4, 8, and 24 hours later. Normal plasma cortisol level should reach 1000 nmol/L by 4 hours. In primary Addison's disease, the cortisol level is reduced at all stages whereas in secondary corticoadrenal insufficiency, a delayed but normal response is seen.
Other tests that may be performed to distinguish between various causes of hypoadrenalism are renin and adrenocorticotropic hormone levels, as well as medical imaging - usually in the form of ultrasound, computed tomography or magnetic resonance imaging (MRI).
ACTH Stimulation Test
This is the most specific test for diagnosing Addison's disease. In this test, blood cortisol, urine cortisol, or both are measured before and after a synthetic form of ACTH is given by injection. In the so-called short, or rapid, ACTH test, measurement of cortisol in blood is repeated 30 to 60 minutes after an intravenous ACTH injection. The normal response after an injection of ACTH is a rise in blood and urine cortisol levels. Patients with either form of adrenal insufficiency respond poorly or do not respond at all.
CRH Stimulation Test
When the response to the short ACTH test is abnormal, a "long" CRH stimulation test is required to determine the cause of adrenal insufficiency. In this test, synthetic CRH is injected intravenously and blood cortisol is measured before and 30, 60, 90, and 120 minutes after the injection. Patients with primary adrenal insufficiency have high ACTHs but do not produce cortisol. Patients with secondary adrenal insufficiency have deficient cortisol responses but absent or delayed ACTH responses. Absent ACTH response points to the pituitary as the cause; a delayed ACTH response points to the hypothalamus as the cause.
In patients suspected of having an addisonian crisis, the doctor must begin treatment with injections of salt, fluids, and glucocorticoid hormones immediately. Although a reliable diagnosis is not possible while the patient is being treated for the crisis, measurement of blood ACTH and cortisol during the crisis and before glucocorticoids are given is enough to make the diagnosis. Once the crisis is controlled and medication has been stopped, the doctor will delay further testing for up to 1 month to obtain an accurate diagnosis.
Suggestive features
Routine investigations may show:[1]
- Hypoglycemia, low blood sugar (worse in children)
- Hyponatraemia (low blood sodium levels)
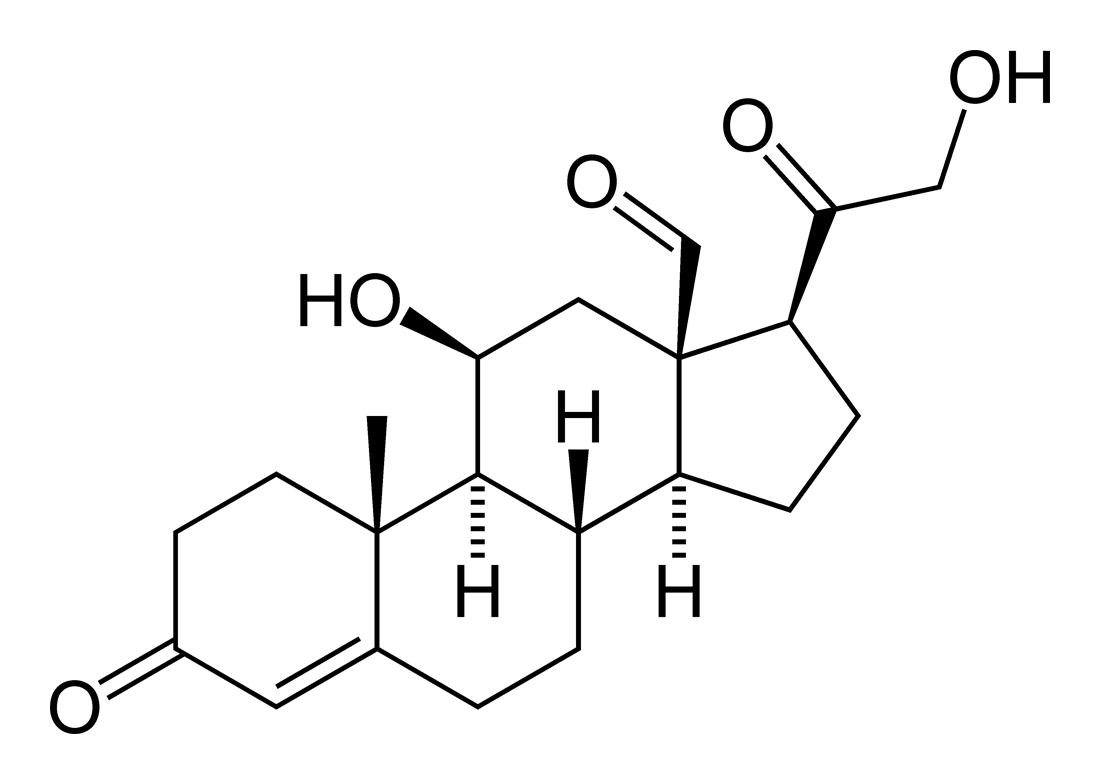
- Hyperkalemia (raised blood potassium levels), due to loss of production of the hormone aldosterone
- Eosinophilia and lymphocytosis (increased number of eosinophils or lymphocytes, two types of white blood cells)
Treatment
Maintenance treatment
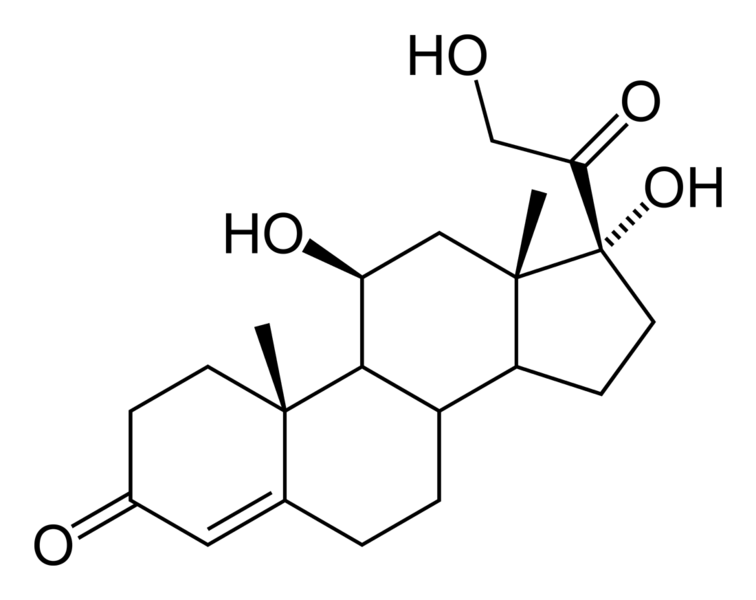
Treatment for Addison's disease involves replacing the missing cortisol (usually in the form of hydrocortisone tablets) in a dosing regimen that mimics the physiological concentrations of cortisol. Treatment must usually be continued for life. In addition, many patients require fludrocortisone as replacement for the missing aldosterone. Caution must be exercised when the person with Addison's disease becomes unwell, has surgery or becomes pregnant. Medication may need to be increased during times of stress, infection, or injury.
Addisonian crisis
Treatment for an acute attack, an Addisonian crisis, usually involves intravenous (into blood veins) injections of:
- Cortisone (cortisol)
- Saline solution (basically a salt water, same clear IV bag as used to treat dehydration)
- Glucose
Surgery
Surgeries may require significant adjustments to medication regimens prior to, during, and following any surgical procedure. The best preparation for any surgery, regardless of how minor or routine it may normally be, is to speak to one's primary physician about the procedure and medication implications well in advance of the surgery.
Pregnancy
Many women with Addison's have given birth successfully and without complication, both through natural labor and through cesarean delivery. Both of these methods will require different preventative measures relating to Addison's medications and dosages. As is always the case, thorough communication with one's primary physician is the best course of action. Occasionally, oral intake of medications will cause debilitating nausea and vomiting, and thus the woman may be switched to injected medications until delivery. [3] Addison's treatment courses by the mother are generally considered safe for baby during pregnancy.
Prognosis
While treatment solutions for Addison's disease are far from precise, overall long-term prognosis is typically good. Because of individual physiological differences, each person with Addison's must work closely with their physician to adjust their medication dosage and schedule to find the most effective routine. Once this is accomplished (and occasional adjustments must be made from time to time, especially during periods of travel, stress, or other medical conditions), symptomology is usually greatly reduced or occasionally eliminated so long as the person continues their dosage schedule.
Patient Education
A person who has adrenal insufficiency should always carry identification stating his or her condition in case of an emergency. The card should alert emergency personnel about the need to inject 100 mg of cortisol if its bearer is found severely injured or unable to answer questions. The card should also include the doctor's name and telephone number and the name and telephone number of the nearest relative to be notified. When traveling, a needle, syringe, and an injectable form of cortisol should be carried for emergencies. A person with Addison's disease also should know how to increase medication during periods of stress or mild upper respiratory infections. Immediate medical attention is needed when severe infections, vomiting, or diarrhea occur. These conditions can precipitate an addisonian crisis. A patient who is vomiting may require injections of hydrocortisone.
People with medical problems may wish to wear a descriptive warning bracelet or neck chain to alert emergency personnel. A number of companies manufacture medical identification products.
See also
References
- ↑ 1.0 1.1 1.2
- ↑ Addison's Disease National Endocrine and Metabolic Diseases Information Service. Retrieved on 26 October, 2007.
- ↑ "addison's disease".
Additional Resources
- Chrousos GP. Glucocorticoid therapy. In: Felig P, Frohman L, eds. Endocrinology and Metabolism. 4th ed. New York: McGraw-Hill; 2001: 609–632.
- Miller W, Chrousos GP. The adrenal cortex. In: Felig P, Frohman L, eds. Endocrinology and Metabolism. 4th ed. New York: McGraw-Hill; 2001: 387–524.
- Stewart PM. The adrenal cortex. In: Larsen P, ed. Williams Textbook of Endocrinology. 10th ed. Philadelphia: Saunders; 2003: 491–551.
- Ten S, New M, Maclaren N. Clinical Review 130: Addison's disease 2001. Journal of Clinical Endocrinology & Metabolism. 2001;86(7):2909–2922.
External links
- Overview of Addison's Disease from the Mayo Clinic
- Addison's Disease Research Today - monthly online journal summarizing recent primary literature on Addison's disease
- National Adrenal Diseases Foundation
- Addison's information from MedicineNet
- "Addison's Disease: The Facts You Need to Know (MedHelp.org)
- The Addison & Cushing International Federation (ACIF)
- Addison's disease info from SeekWellness.com
- Information about Addison's disease in canines (dogs)
- Antibodies to adrenal gland
- Immunofluorescence images
- Endocrine and Metabolic Diseases Information Service
Support groups
- Addison's Disease Self Help Group (ADSHG) - UK support group
- Australian Addison's Disease Association - Australian support and information group
- Nederlandse Vereniging voor Addison en Cushing Patiënten - Dutch support and information group with information and documentation in English
- Addresses of patient organisations and support groups around the world
bg:Адисонова болест cs:Addisonova choroba da:Addisons sygdom de:Nebennierenrindeninsuffizienz it:Morbo di Addison he:מחלת אדיסון ms:Penyakit Addison nl:Ziekte van Addison sk:Addisonova choroba fi:Addisonin tauti sv:Addisons sjukdom