Sandbox:Nasrin: Difference between revisions
Jump to navigation
Jump to search
mNo edit summary |
No edit summary |
||
| Line 19: | Line 19: | ||
=[[AKI pathophysiology|Pathophysiology]]= | =[[AKI pathophysiology|Pathophysiology]]= | ||
*Angiotensin-converting enzyme 2 ([[ACE2]]), which is a primary receptor for [[SARS-CoV-2]] entry into cells, mostly presents in | *Angiotensin-converting enzyme 2 ([[ACE2]]), which is a primary receptor for [[SARS-CoV-2]] entry into cells, mostly presents in renal tubular epithelial cells as well as lungs and heart.<ref name="MalhaMueller2020">{{cite journal|last1=Malha|first1=Line|last2=Mueller|first2=Franco B.|last3=Pecker|first3=Mark S.|last4=Mann|first4=Samuel J.|last5=August|first5=Phyllis|last6=Feig|first6=Peter U.|title=COVID-19 and the Renin-Angiotensin System|journal=Kidney International Reports|volume=5|issue=5|year=2020|pages=563–565|issn=24680249|doi=10.1016/j.ekir.2020.03.024}}</ref> | ||
*Despite kidney injury following [[COVID-19]] infection is less frequent than severe lung injury, [[ACE2]]: [[ACE]] ratio is higher in the kidneys compared to the respiratory system. (1:1 in the kidneys VS 1:20 in the respiratory system)<ref name="MalhaMueller2020">{{cite journal|last1=Malha|first1=Line|last2=Mueller|first2=Franco B.|last3=Pecker|first3=Mark S.|last4=Mann|first4=Samuel J.|last5=August|first5=Phyllis|last6=Feig|first6=Peter U.|title=COVID-19 and the Renin-Angiotensin System|journal=Kidney International Reports|volume=5|issue=5|year=2020|pages=563–565|issn=24680249|doi=10.1016/j.ekir.2020.03.024}}</ref> | *Despite kidney injury following [[COVID-19]] infection is less frequent than severe lung injury, [[ACE2]]: [[ACE]] ratio is higher in the kidneys compared to the respiratory system. (1:1 in the kidneys VS 1:20 in the respiratory system)<ref name="MalhaMueller2020">{{cite journal|last1=Malha|first1=Line|last2=Mueller|first2=Franco B.|last3=Pecker|first3=Mark S.|last4=Mann|first4=Samuel J.|last5=August|first5=Phyllis|last6=Feig|first6=Peter U.|title=COVID-19 and the Renin-Angiotensin System|journal=Kidney International Reports|volume=5|issue=5|year=2020|pages=563–565|issn=24680249|doi=10.1016/j.ekir.2020.03.024}}</ref> | ||
* After [[SARS-CoV-2]] enters through the nasal cavity, it may travel to the kidneys and enters the bloodstream leading to severe inflammatory response activation and cytokine storm. | |||
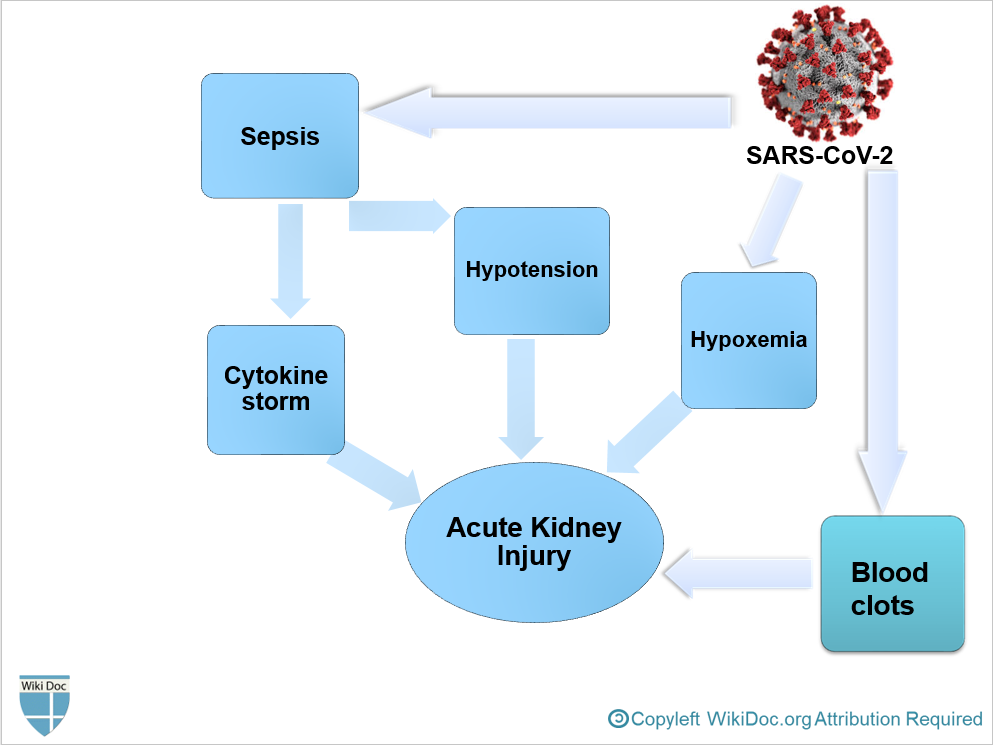
*It is thought that [[AKI]] following COVID-19 is the result of<ref name="MalhaMueller2020">{{cite journal|last1=Malha|first1=Line|last2=Mueller|first2=Franco B.|last3=Pecker|first3=Mark S.|last4=Mann|first4=Samuel J.|last5=August|first5=Phyllis|last6=Feig|first6=Peter U.|title=COVID-19 and the Renin-Angiotensin System|journal=Kidney International Reports|volume=5|issue=5|year=2020|pages=563–565|issn=24680249|doi=10.1016/j.ekir.2020.03.024}}</ref> | *It is thought that [[AKI]] following COVID-19 is the result of<ref name="MalhaMueller2020">{{cite journal|last1=Malha|first1=Line|last2=Mueller|first2=Franco B.|last3=Pecker|first3=Mark S.|last4=Mann|first4=Samuel J.|last5=August|first5=Phyllis|last6=Feig|first6=Peter U.|title=COVID-19 and the Renin-Angiotensin System|journal=Kidney International Reports|volume=5|issue=5|year=2020|pages=563–565|issn=24680249|doi=10.1016/j.ekir.2020.03.024}}</ref> | ||
**[[Sepsis]] | **[[Sepsis]] | ||
**Hypotension | **Hypotension | ||
**Hypoxemia | |||
[[File:AKI physiopathology COVID.PNG|600px|center]] | |||
=[[AKI epidemiology and demographics|Epidemiology and Demographics]]= | =[[AKI epidemiology and demographics|Epidemiology and Demographics]]= | ||
| Line 57: | Line 62: | ||
'''Laboratory Findings''' | '''Laboratory Findings''' | ||
*Laboratory findings consistent with the diagnosis of [[AKI]] include: | |||
**Elevated [[BUN]] level | |||
**Based on KDIGO definition for the diagnosis of AKI<ref name="pmid22890468">{{cite journal| author=Khwaja A| title=KDIGO clinical practice guidelines for acute kidney injury. | journal=Nephron Clin Pract | year= 2012 | volume= 120 | issue= 4 | pages= c179-84 | pmid=22890468 | doi=10.1159/000339789 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22890468 }} </ref>: | |||
***Elevated serum Creatinine by ≥0.3 mg/dl (≥26.5 μmol/l) within 48 hours; or | |||
***Elevated serum Creatinine to ≥1.5 times baseline within the previous 7 days; or | |||
***Urine volume < 0.5 ml/kg/h for >6 hours | |||
'''Electrocardiogram''' | '''Electrocardiogram''' | ||
*There are no specific ECG findings associated with AKI. However, electrolyte disturbances such as hyperkalemia might lead to various ECG findings. | |||
'''Ultrasound Finding''' | '''Ultrasound Finding''' | ||
| Line 66: | Line 78: | ||
=Treatment= | =Treatment= | ||
*Management of [[AKI]] following [[COVID-19]] includes treatment of infection, identifying electrolyte disorders, and [[intravenous fluid]] administration. | |||
'''AKI Medical Therapy''' | '''AKI Medical Therapy''' | ||
==References== | |||
{{Reflist|2}} | |||
[[Category:Disease]] | [[Category:Disease]] | ||
Revision as of 22:48, 20 June 2020
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Nasrin Nikravangolsefid, MD-MPH [2]
Complication 1: Acute Kidney Injury in COVID-19
For patient information, click here
Synonyms and keywords: Acute Kidney Injury, Acute Renal Failure, AKI, ARF
Overview
Pathophysiology
- Angiotensin-converting enzyme 2 (ACE2), which is a primary receptor for SARS-CoV-2 entry into cells, mostly presents in renal tubular epithelial cells as well as lungs and heart.[1]
- Despite kidney injury following COVID-19 infection is less frequent than severe lung injury, ACE2: ACE ratio is higher in the kidneys compared to the respiratory system. (1:1 in the kidneys VS 1:20 in the respiratory system)[1]
- After SARS-CoV-2 enters through the nasal cavity, it may travel to the kidneys and enters the bloodstream leading to severe inflammatory response activation and cytokine storm.
- It is thought that AKI following COVID-19 is the result of[1]
- Sepsis
- Hypotension
- Hypoxemia
Epidemiology and Demographics
- Early reports from china revealed that COVID-19 rarely involves the kidneys, as Acute Renal Failure was not seen among COVID-19 hospitalized patients and mild BUN or creatinine rise [10.8%] and mild proteinuria [7.2%] occurred. [2]
- However, recent study found 75.4% of hospitalized patients with COVID-19 pneumonia developed hematuria, proteinuria, and AKI. [3] But, these findings are not significantly different from other critical diseases.
Natural history
- Severe COVID-19 pneumonia and severe acute respiratory distress syndrome are associated with developing AKI.[3]
- Approximately half of the new AKI cases following COVID-19 is mild with good short-term prognosis.
- If no improvement occurs during follow-up, it is contributed to higher mortality.[3]
History and Symptoms
- Patients in the early stages of kidney failure may be asymptomatic. If left untreated, patients may progress to develop Azotemia and Uremia, which occur due to the buildup of waste materials in the blood.
History and Symptoms
- Symptoms of kidney injury include[4]:
- Nausea and Vomiting
- Weakness
- Fatigue
- Confusion
- Weight loss
- Loss of appetite
- Oliguria or Anuria
- Fluid retention, leading edema and swelling of face, extremities
- Electrolyte imbalance; High level of Potassium which leads to cardiac arrhythmia
Physical Examination
Diagnosis
Laboratory Findings
- Laboratory findings consistent with the diagnosis of AKI include:
Electrocardiogram
- There are no specific ECG findings associated with AKI. However, electrolyte disturbances such as hyperkalemia might lead to various ECG findings.
Ultrasound Finding
Other Diagnostic Studies
Treatment
- Management of AKI following COVID-19 includes treatment of infection, identifying electrolyte disorders, and intravenous fluid administration.
AKI Medical Therapy
References
- ↑ 1.0 1.1 1.2 Malha, Line; Mueller, Franco B.; Pecker, Mark S.; Mann, Samuel J.; August, Phyllis; Feig, Peter U. (2020). "COVID-19 and the Renin-Angiotensin System". Kidney International Reports. 5 (5): 563–565. doi:10.1016/j.ekir.2020.03.024. ISSN 2468-0249.
- ↑ Wang, Luwen; Li, Xun; Chen, Hui; Yan, Shaonan; Li, Dong; Li, Yan; Gong, Zuojiong (2020). "Coronavirus Disease 19 Infection Does Not Result in Acute Kidney Injury: An Analysis of 116 Hospitalized Patients from Wuhan, China". American Journal of Nephrology. 51 (5): 343–348. doi:10.1159/000507471. ISSN 0250-8095.
- ↑ 3.0 3.1 3.2 Pei, Guangchang; Zhang, Zhiguo; Peng, Jing; Liu, Liu; Zhang, Chunxiu; Yu, Chong; Ma, Zufu; Huang, Yi; Liu, Wei; Yao, Ying; Zeng, Rui; Xu, Gang (2020). "Renal Involvement and Early Prognosis in Patients with COVID-19 Pneumonia". Journal of the American Society of Nephrology. 31 (6): 1157–1165. doi:10.1681/ASN.2020030276. ISSN 1046-6673.
- ↑ Skorecki K, Green J, Brenner BM (2005). "Chronic renal failure". In Kasper DL, Braunwald E, Fauci AS, et al. Harrison's Principles of Internal Medicine (16th ed.). New York, NY: McGraw-Hill. pp. 1653–63. ISBN 978-0-07-139140-5.
- ↑ Khwaja A (2012). "KDIGO clinical practice guidelines for acute kidney injury". Nephron Clin Pract. 120 (4): c179–84. doi:10.1159/000339789. PMID 22890468.