Medulloblastoma pathophysiology: Difference between revisions
| Line 28: | Line 28: | ||
::* Present among older children | ::* Present among older children | ||
::* Cytogenetic markers include classic [[monosomy]] 6 | ::* Cytogenetic markers include classic [[monosomy]] 6 | ||
::* Molecular markers include [[ | ::* Molecular markers include [[beta-catenin]] | ||
:* SHH subgroup: | :* SHH subgroup: | ||
::* Present among 25% of medulloblastoma patients | ::* Present among 25% of medulloblastoma patients | ||
Revision as of 01:16, 30 September 2015
|
Medulloblastoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case studies |
|
Medulloblastoma pathophysiology On the Web |
|
American Roentgen Ray Society Images of Medulloblastoma pathophysiology |
|
Risk calculators and risk factors for Medulloblastoma pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Haytham Allaham, M.D. [2]
Overview
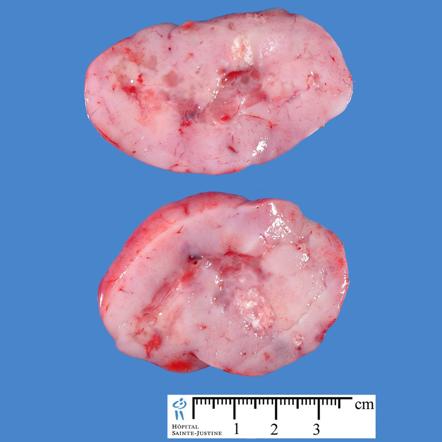
Medulloblastoma arises from the cerebellar stem cells, which are normally involved in the anatomical development of the cerebellum and other posterior fossa structures. Medulloblastoma is an invasive and rapidly growing tumor which frequently metastasize to different organs of the body. Genes involved in the pathogenesis of medulloblastoma include CTNNB1 gene, PTCH1 gene, MLL2 gene, SMARCA4 gene, DDX3X gene, CTDNEP1 gene, KDM6A gene, and TBR1 gene. Medullobastomas is associated with a number of syndromes that include Gorlin syndrome and Turcot syndrome.[1] On gross pathology, a pink, solid, and well circumscribed mass is a characteristic finding of medulloblastoma. On microscopic histopathological analysis, round tumor cells, elevated mitotic rate, increased nucleus:cytoplasm ratio, and presence of Homer-Wright rosettes are characteristic findings of medulloblastoma.[2]
Pathogenesis
- Medulloblastoma arises from the cerebellar stem cells, which are normally involved in the anatomical development of the cerebellum and other posterior fossa structures.[1]
- Medulloblastoma is usually located at the infratentorial region, where it forms a mass between the brain stem and the cerebellum in the vicinity of the fourth ventricle.[1]
- Medulloblastoma is an invasive and rapidly growing tumor.[1]
- Unlike most brain tumors, medulloblastoma may spread through the cerebrospinal fluid and metastasize to different organs of the body.[1]
Genetics
- Development of medulloblastoma is the result of multiple genetic mutations.[1]
- Genes involved in the pathogenesis of medulloblastoma include:[1]
- CTNNB1 gene on chromosome 3
- PTCH1 gene located on chromosome 9
- MLL2 gene located on chromosome 12
- SMARCA4 gene located on chromosome 19
- DDX3X gene located on X chromosome
- CTDNEP1 gene located on chromosome 17
- KDM6A gene located on X chromosome
- TBR1 gene located on chromosome 2
- Molecular subtypes of medulloblastoma include:[3]
- WNT subgroup:
- Present among 10% of medulloblastoma patients
- Present among older children
- Cytogenetic markers include classic monosomy 6
- Molecular markers include beta-catenin
- SHH subgroup:
- Present among 25% of medulloblastoma patients
- Present among infants and adults
- Cytogenetic markers include chromosome 9q loss
- Molecular markers include SFRP1 or GAB1
- Group 3 medulloblastoma:
- Present among 30% of medulloblastoma patients
- Present among younger younger children
- Cytogenetic markers include isochromosome 17q
- Molecular markers include MYC activation in 50% of this subtype
- Group 4 medulloblastoma:
- Present among 35% of medulloblastoma patients
- Present among younger younger children
- Cytogenetic markers include isochromosome 17q
- Molecular markers are still under investigation
Associated Conditions
Gross Pathology
- On gross pathology, a pink, solid, and well circumscribed mass is a characteristic finding of medulloblastoma.[1]
- The following image demonstrates the gross pathology observed in medulloblastoma:
-
Image courtesy of Dr Frank Gaillard Radiopaedia(original file "here"). Creative Commons BY-SA-NC
Mircoscopic Pathology
- On microscopic histopathological analysis, round tumor cells, elevated mitotic rate, increased nucleus:cytoplasm ratio, and presence of Homer-Wright rosettes are characteristic findings of medulloblastoma.[2]
- Shown below is a series of microscopic images observed in medulloblastoma:
-
Medulloblastoma smear[2]
-
Medulloblastoma smear [2]
-
Medulloblastoma smear demonstrating Homer-Wright rosettes[2]
-
Medulloblastoma smear demonstrating cerebellar infiltrative growth[2]
-
Anaplastic large cell medulloblastoma smear[2]
-
Medulloblastoma smear[2]
-
Desmoplastic medulloblastoma on MIB-1 immunostaining[2]
-
Medulloblastoma smear demonstrating partial MAP2 immunoreactivity[2]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 Medulloblastoma. Wikipedia(2015) https://en.wikipedia.org/wiki/Medulloblastoma Accessed on September 2015
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 Medulloblastoma. Librepathology(2015) http://librepathology.org/wiki/index.php/Medulloblastoma Accessed on September, 28th 2015
- ↑ Leary SE, Olson JM (2012) The molecular classification of medulloblastoma: driving the next generation clinical trials. Curr Opin Pediatr 24 (1):33-9. DOI:10.1097/MOP.0b013e32834ec106 PMID: 22189395
- ↑ Medulloblastoma. Radiopaedia(2015) http://radiopaedia.org/articles/medulloblastoma Accessed on September, 28th 2015
![Medulloblastoma smear[2]](/images/8/8c/Medulloblsatoma.JPG)
![Medulloblastoma smear [2]](/images/1/1c/Medulloblsatoma_2.JPG)
![Medulloblastoma smear demonstrating Homer-Wright rosettes[2]](/images/7/77/Medulloblastoma_3.jpg)
![Medulloblastoma smear demonstrating cerebellar infiltrative growth[2]](/images/b/b8/Medulloblastoma_4.jpg)
![Medullloblastoma smear demonstrating demsomplastic nodular growth[2]](/images/6/63/Medulloblastoma_5.jpg)
![Anaplastic large cell medulloblastoma smear[2]](/images/e/e5/Medulloblastoma_6.jpg)
![Medulloblastoma smear[2]](/images/5/5c/Medulloblastoma_7.jpg)
![Desmoplastic medulloblastoma smear on reticulin stain demonstrating "pale islands"[2]](/images/c/c9/Medulloblastoma_8.jpg)
![Desmoplastic medulloblastoma on MIB-1 immunostaining[2]](/images/d/d2/Medulloblastoma_9.jpg)
![Medulloblastoma smear demonstrating areas of geographic necrosis[2]](/images/2/25/Medulloblastoma_Areas_of_geographic_necrosis..jpg)
![Medulloblastoma smear demonstrating epitheloid ribboning and nuclear moulding of tumor cells[2]](/images/9/9e/Medulloblastoma_Epitheloid_ribboning_and_nuclear_moulding_of_tumor_cells..jpg)
![Medulloblastoma smear demonstrating partial MAP2 immunoreactivity[2]](/images/d/dd/Medulloblastoma_Partial_MAP2_immunoreactivity..jpg)