Aortic dissection pathophysiology: Difference between revisions
| (70 intermediate revisions by 10 users not shown) | |||
| Line 1: | Line 1: | ||
<div style="-webkit-user-select: none;"> | |||
__NOTOC__ | |||
{{Template:Aortic dissection}} | {{Template:Aortic dissection}} | ||
{{CMG}}; {{AE}} {{CZ}} {{Sahar}} | |||
==Overview== | |||
[[Aortic]] dissection begins as a tear in the [[aortic]] wall in > 95% of patients. The tear is usually transverse, extends through the [[intima]] and halfway through the [[tunica media|media]] and involves ~50% of the [[aortic]] circumference. Two thirds of dissections originate in the [[ascending aorta]], and 20% are in the [[proximal]] [[descending aorta]]. | |||
==Pathophysiology== | |||
===Normal Anatomy of the Aorta=== | |||
As with all other [[artery|arteries]], the [[aorta]] is made up of three layers. The layer that is in direct contact with the flow of blood is the [[tunica intima]], commonly called the [[intima]]. This layer is made up of mainly [[endothelial cell]]s. Just deep to this layer is the [[tunica media]], known as the [[tunica media|media]]. This middle layer is made up of [[smooth muscle]] cells and [[elastic tissue]]. The outermost layer (furthest from the flow of blood) is known as the [[tunica adventitia]] or the [[adventitia]]. This layer is composed of [[connective tissue]].[[Image:AoDissect Schema 01a.png|left|thumb|Blood penetrates the [[intima]] and enters the [[tunica media|media]] layer.]] | |||
===Pathogenesis=== | |||
====Initial Intimal Tear==== | |||
== | * [[Aortic]] dissection begins as a tear in the [[aortic]] wall in > 95% of patients. | ||
*It is usually transverse, extends through the [[intima]] and halfway through the [[tunica media|media]] and involves ~50% of the [[aortic]] circumference. | |||
====Location of Dissections==== | |||
:*The initial tear is usually within 100 mm of the [[aortic valve]]. | |||
:*65% of dissections originate in the [[ascending aorta]], distal to the [[aortic valve]] and [[coronary]] [[ostium|ostia]] | |||
:*10% arise in the [[transverse aortic arch]] | |||
:*20% in the [[proximal]] [[descending aorta]] | |||
:*5% in the more [[distal]] [[descending aorta]] | |||
== | ====Propagation of the Intimal Tear==== | ||
In an [[aortic]] dissection, blood penetrates the ''[[intima]]'' and enters the ''[[tunica media|media]]'' layer. The high pressure rips the [[biological tissue|tissue]] of the ''[[tunica media|media]]'' apart, allowing more blood to enter. This can propagate along the length of the aorta for a variable distance, dissecting either towards or away from the [[heart]] or both. | |||
Once a tear develops, blood then passes into the [[tunica media|media]], and a [[false lumen]] is dissected in the outer layer of [[aortic]] [[tunica media|media]] involving ~50% of the [[aortic]] circumference. This [[false lumen]] can enlarge, and compress the true [[lumen]], as well as extend [[proximal]]ly or [[distal]]ly and occlude [[aortic]] branches. For some unknown reason, the right [[lateral]] wall of the [[ascending aorta]] is the most common site for dissection. The [[right coronary artery]] can become occluded as a result of this propagation. | |||
Separating the [[false lumen]] from the true [[lumen]] is a layer of [[intima]]l [[tissue]]. This [[tissue]] is known as the ''[[intima]]l flap''. As blood flows down the [[false lumen]], it may cause secondary tears in the [[intima]]. Through these secondary tears, the blood can re-enter the true [[lumen]]. | |||
== | ====Aortic Dissection in the Absence of an Intimal Tear==== | ||
In about 13% of [[aortic]] dissections, there is no evidence of an [[intima]]l tear. It is believed that in these cases the inciting event is an intramural [[hematoma]] (caused by [[hemorrhage]] within the [[tunica media|media]]). Since there is no direct connection between the true [[lumen]] and the [[false lumen]] in these cases, it is difficult to diagnose an [[aortic]] dissection by [[aortography]] if the [[etiology]] is an intramural [[hematoma]]. An [[aortic]] dissection secondary to an intramural [[hematoma]] should be treated the same as one caused by an [[intimal]] tear. | |||
An [[aortic]] intramural [[hematoma]] can form when the [[vasa vasorum]] ruptures into the [[aortic]] wall. This is distinguished from dissection by the lack of an [[intima]]l tear. This disorder parallels [[aortic]] dissection in terms of [[prognosis]] when the [[ascending aorta]] or [[aortic arch]] is involved, and rapid [[surgery|surgical]] intervention is indicated. Involvement of the [[descending aorta]], however, carries a better [[prognosis]] than dissection, and outcome tends to be similar with medical or [[surgery|surgical]] [[therapy]]. | |||
== | ==Genetics== | ||
[[Genes]] involved in the [[pathogenesis]] of aortic dissection include:<ref name="PinardJones2019">{{cite journal|last1=Pinard|first1=Amélie|last2=Jones|first2=Gregory T.|last3=Milewicz|first3=Dianna M.|title=Genetics of Thoracic and Abdominal Aortic Diseases|journal=Circulation Research|volume=124|issue=4|year=2019|pages=588–606|issn=0009-7330|doi=10.1161/CIRCRESAHA.118.312436}}</ref><ref name="VerhagenKempers2018">{{cite journal|last1=Verhagen|first1=Judith M.A.|last2=Kempers|first2=Marlies|last3=Cozijnsen|first3=Luc|last4=Bouma|first4=Berto J.|last5=Duijnhouwer|first5=Anthonie L.|last6=Post|first6=Jan G.|last7=Hilhorst-Hofstee|first7=Yvonne|last8=Bekkers|first8=Sebastiaan C.A.M.|last9=Kerstjens-Frederikse|first9=Wilhelmina S.|last10=van Brakel|first10=Thomas J.|last11=Lambermon|first11=Eric|last12=Wessels|first12=Marja W.|last13=Loeys|first13=Bart L.|last14=Roos-Hesselink|first14=Jolien W.|last15=van de Laar|first15=Ingrid M.B.H.|title=Expert consensus recommendations on the cardiogenetic care for patients with thoracic aortic disease and their first-degree relatives|journal=International Journal of Cardiology|volume=258|year=2018|pages=243–248|issn=01675273|doi=10.1016/j.ijcard.2018.01.145}}</ref> | |||
*[[FBN1]] ([[fibrillin-1]]) | |||
*[[Lysyl oxidase|LOX]] ([[lysyl oxidase]]) | |||
*[[MYH11]] (smooth muscle myosin heavy chain 11) | |||
*[[ACTA2]] (smooth muscle α-actin 2) | |||
*[[MYLK]] (myosin light chain kinase) | |||
*[[PRKG1]] (protein kinase cGMP-dependent type 1) | |||
*[[COL3A1]] (α-1 procollagen, type III) | |||
*[[TGFBR1]] (TGF-β receptor type I) | |||
*[[TGFBR2]] (TGF-β receptor type II) | |||
*TGFB2 | |||
*[[SMAD3]] (mothers against decapentaplegic drosophila homolog 3) | |||
==Associated Conditions== | |||
[[Conditions]] associated with aortic dissection include:<ref name="PinardJones2019">{{cite journal|last1=Pinard|first1=Amélie|last2=Jones|first2=Gregory T.|last3=Milewicz|first3=Dianna M.|title=Genetics of Thoracic and Abdominal Aortic Diseases|journal=Circulation Research|volume=124|issue=4|year=2019|pages=588–606|issn=0009-7330|doi=10.1161/CIRCRESAHA.118.312436}}</ref> | |||
*[[Aortic aneurysm]] | |||
*Smooth muscle dysfunction syndrome | |||
*[[Marfan syndrome]] | |||
*[[Vascular Ehlers-Danlos syndrome]] | |||
*[[Loeys-Dietz syndrome|Loeys-Dietz syndromes]] | |||
==Gross Pathology== | |||
[http://www.peir.net Images shown below are courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology] | |||
<div align="left"> | |||
<gallery heights="225" widths="225"> | |||
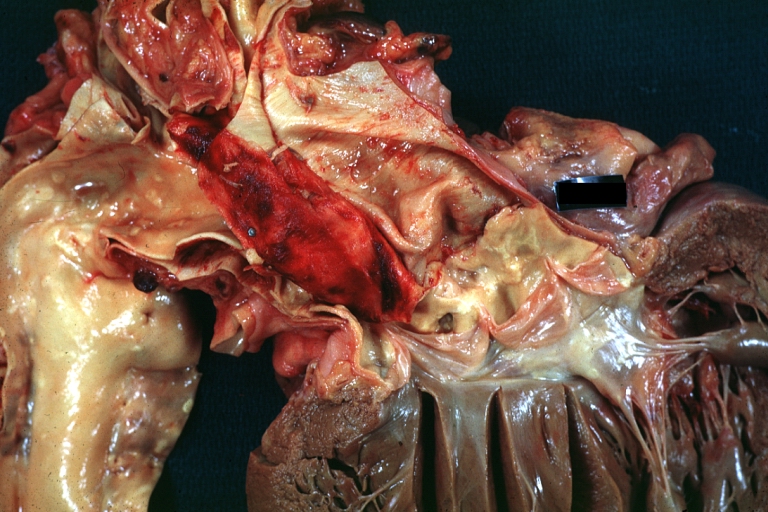
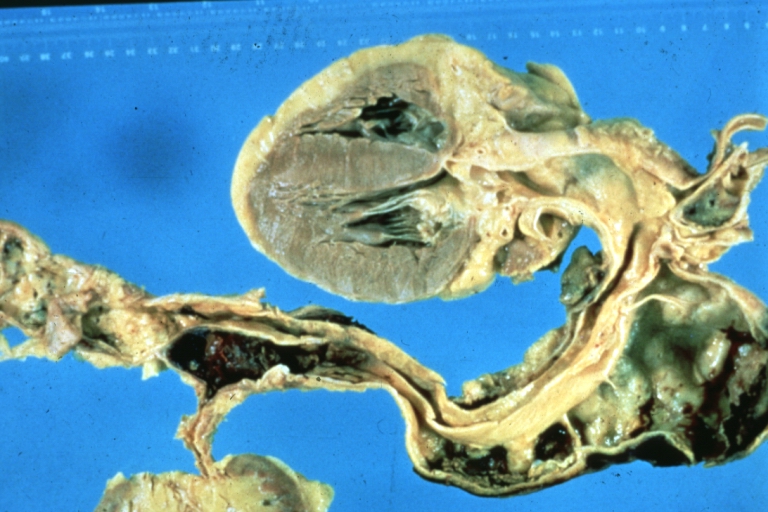
Image:Aortic dissection 1.jpg|Dissecting [[Aneurysm]]: Gross fixed tissue external view of heart [[aortic arch]] and [[descending aorta]] showing dilated first and second portion of arch from [[anterior]] projection. | |||
Image:Aortic aneurysm 8.jpg|Dissecting [[Aneurysm]]: Gross, a very good example of dissection beginning just above [[aortic]] ring. | |||
Image:Aortic aneurysm 24.jpg|Dissecting [[Aneurysm]]: Gross dissection first portion of arch fixed [[specimen]] (a good example). | |||
</gallery> | |||
</div> | |||
<div align="left"> | |||
<gallery heights="175" widths="175"> | |||
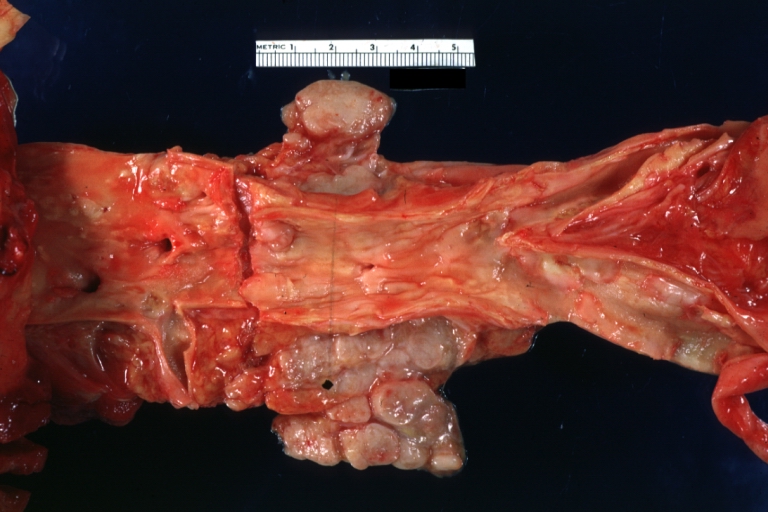
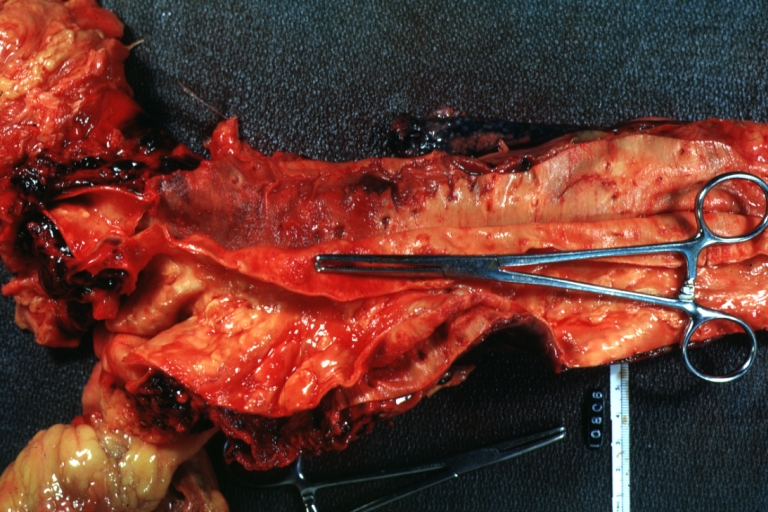
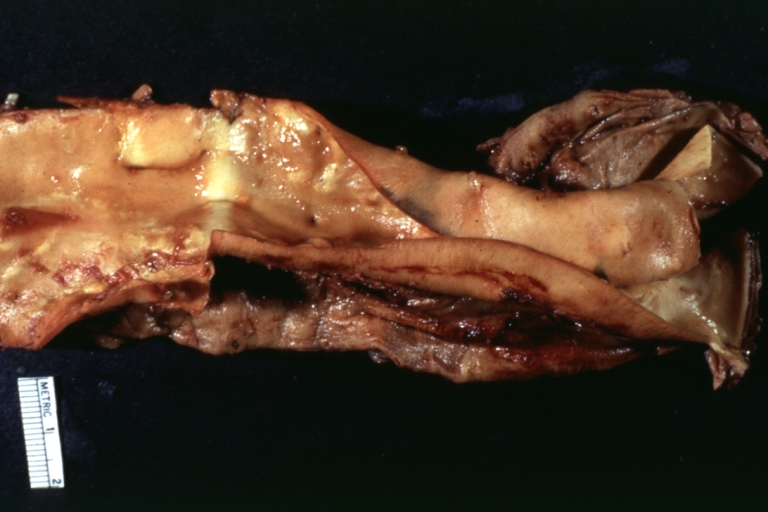
Image:Aortic aneurysm 1.jpg|Dissecting [[Aneurysm]]: Gross very good example dissected channel has been opened. | |||
Image:Aortic aneurysm 2.jpg|Dissecting [[Aneurysm]]: Gross external view good appearance from [[adventitia]]. | |||
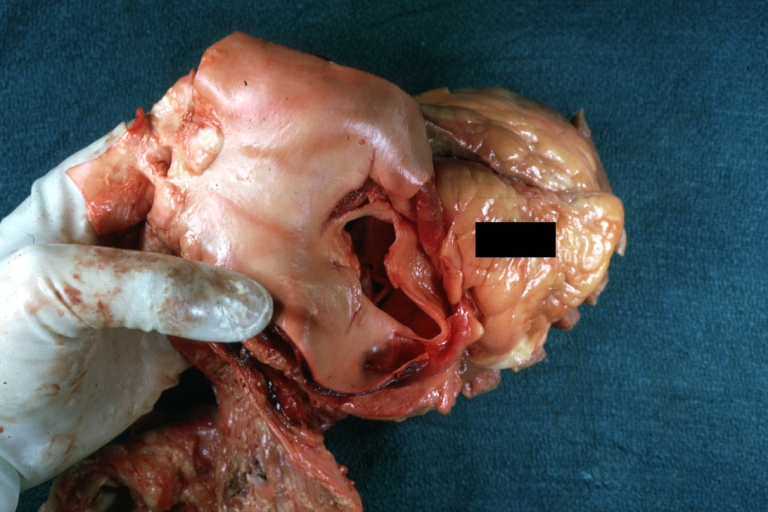
Image:Aortic aneurysm 3.jpg|Dissecting [[Aneurysm]]: Gross opened false channel. | |||
</gallery> | |||
</div> | |||
== | <div align="left"> | ||
<gallery heights="175" widths="175"> | |||
Image:Aortic aneurysm 4.jpg|Dissecting [[Aneurysm]]: Gross good example dissection beginning at third portion [[aortic arch]]. | |||
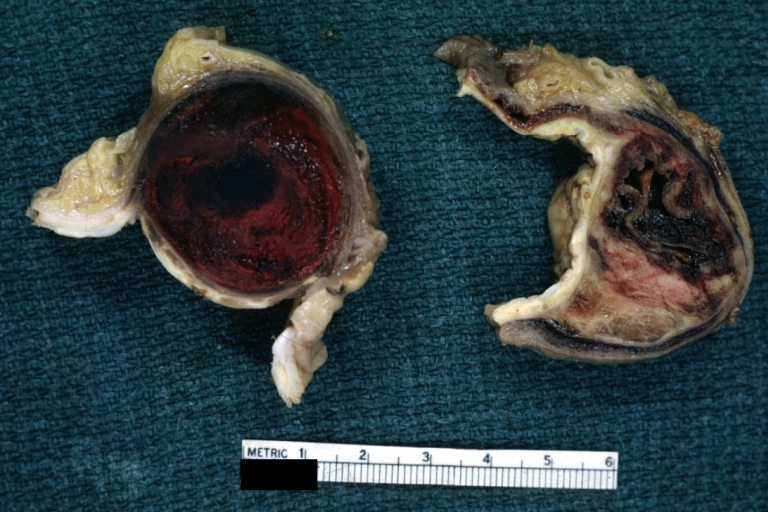
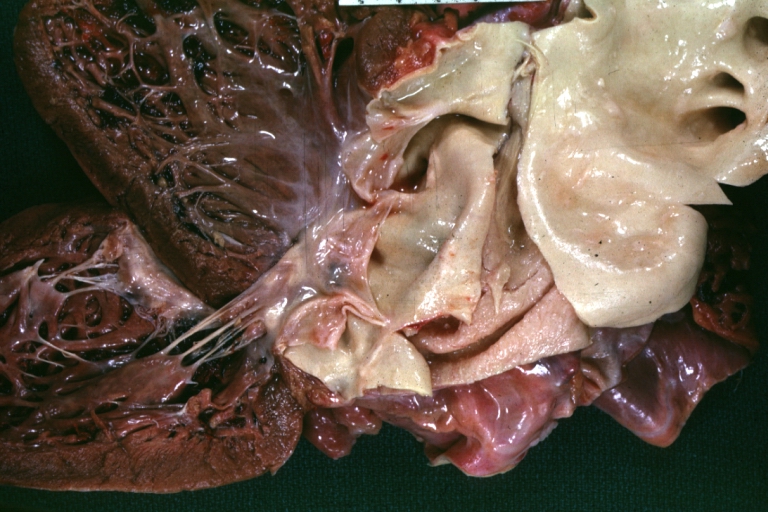
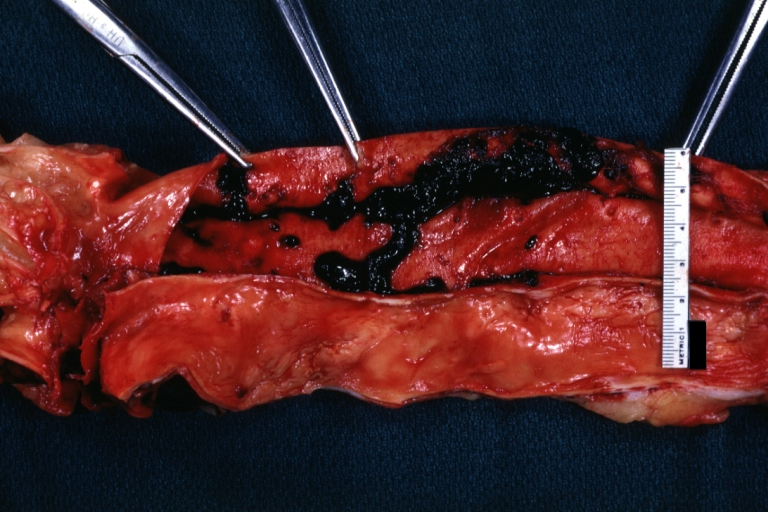
Image:Aortic aneurysm 5.jpg|Dissecting [[Aneurysm]]: Gross cross sections showing [[thrombus]] in [[false lumen]]. True [[lumen]] has been opened longitudinally. | |||
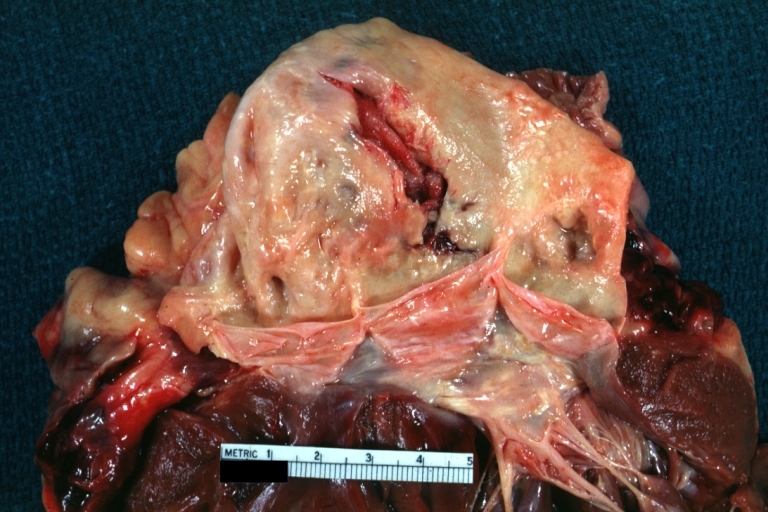
Image:Aortic aneurysm 6.jpg|Dissecting [[Aneurysm]]: Gross shows origin just above [[aortic valve]] false channel shown in [[descending aorta|descending]] [[thoracic aorta]] (very good example). | |||
</gallery> | |||
</div> | |||
<div align="left"> | |||
<gallery heights="175" widths="175"> | |||
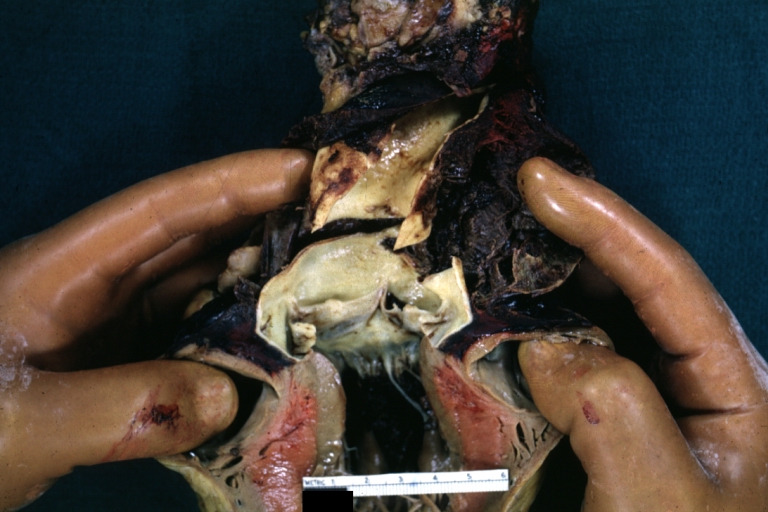
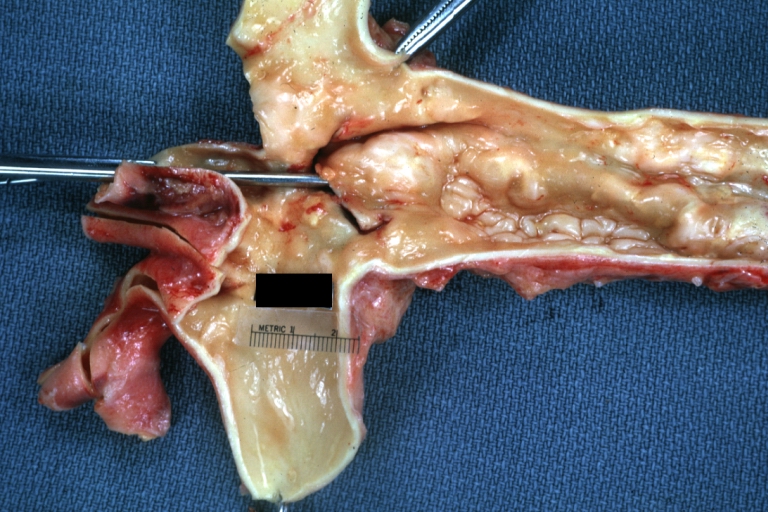
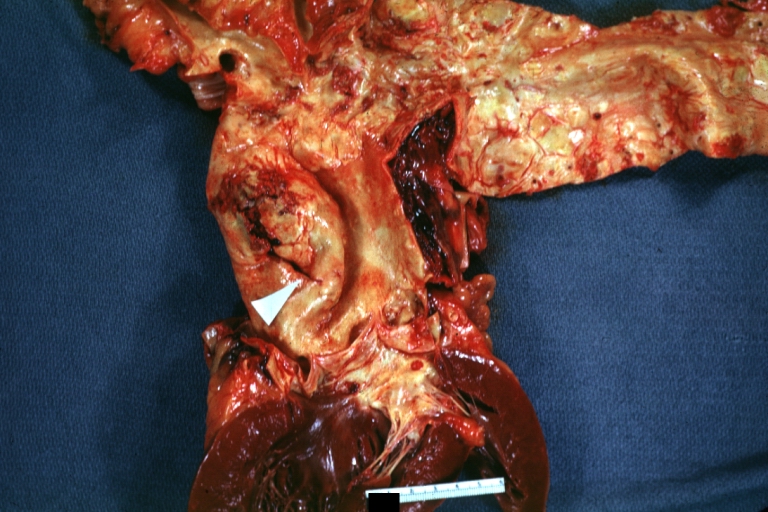
Image:Aortic aneurysm 10.jpg|Dissecting [[Aneurysm]]: Gross, an excellent example, starting just above the [[aortic valve]] with reflection of [[aorta]] to show the dissection tract and some [[thrombus]] | |||
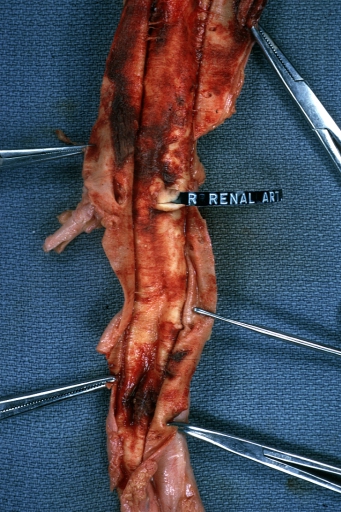
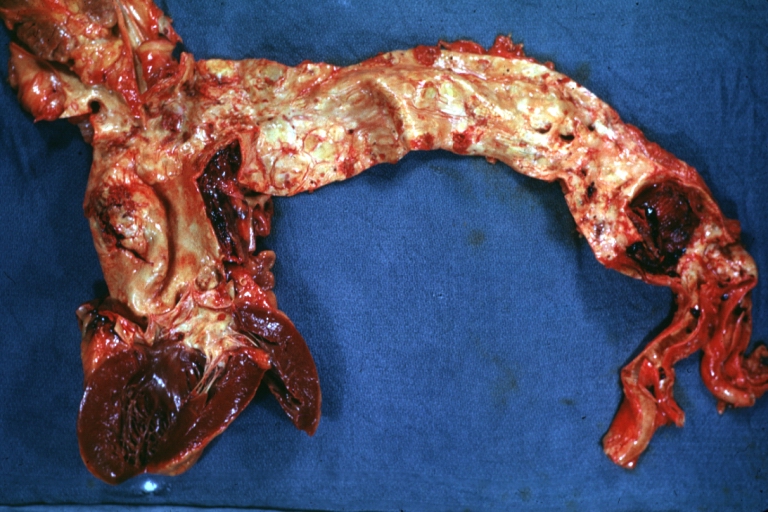
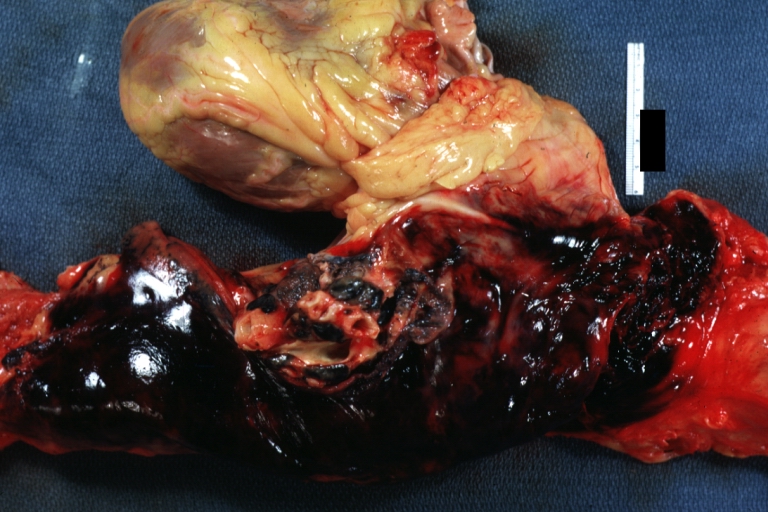
: | Image:Aortic aneurysm 11.jpg|Dissecting [[Aneurysm]]: Gross shows dilated [[aorta]] with extensive [[atherosclerosis]] dissection is seen, a small [[abdominal aorta]] [[atherosclerotic]] [[aneurysm]] is present good for association of [[dilation]] with dissection | ||
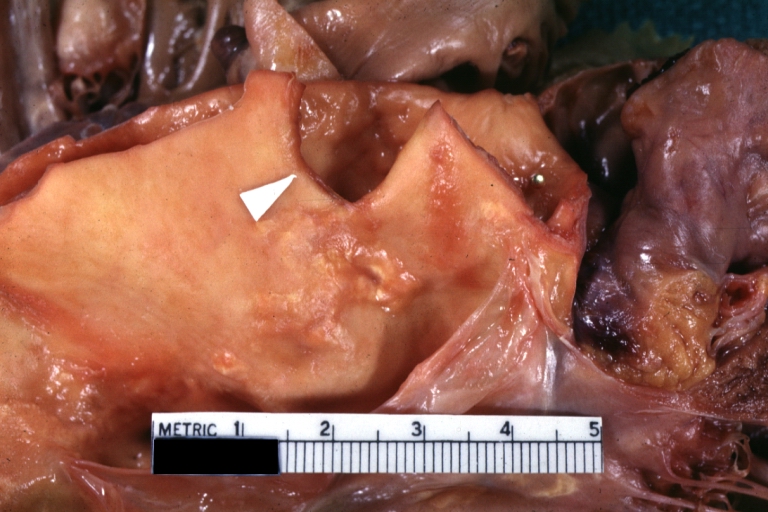
: | Image:Aortic aneurysm 12.jpg|Dissecting [[Aneurysm]]: Gross arrow points to start of dissection in first portion [[aortic arch]] good but not the best example shows [[dilation]] | ||
Image:Aortic aneurysm 13.jpg|Dissecting [[Aneurysm]]: Gross, very good to show start of dissection above [[aortic valve]] and blood in false channel. | |||
</gallery> | |||
:: | </div> | ||
Aortic | <div align="left"> | ||
<gallery heights="175" widths="175"> | |||
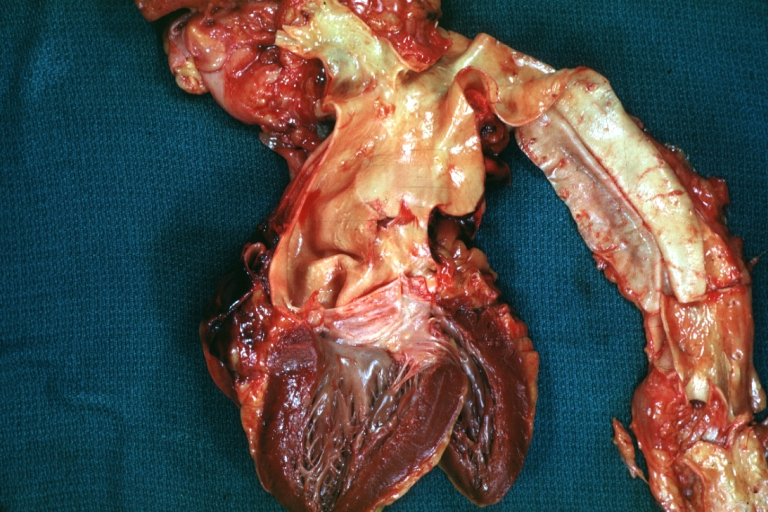
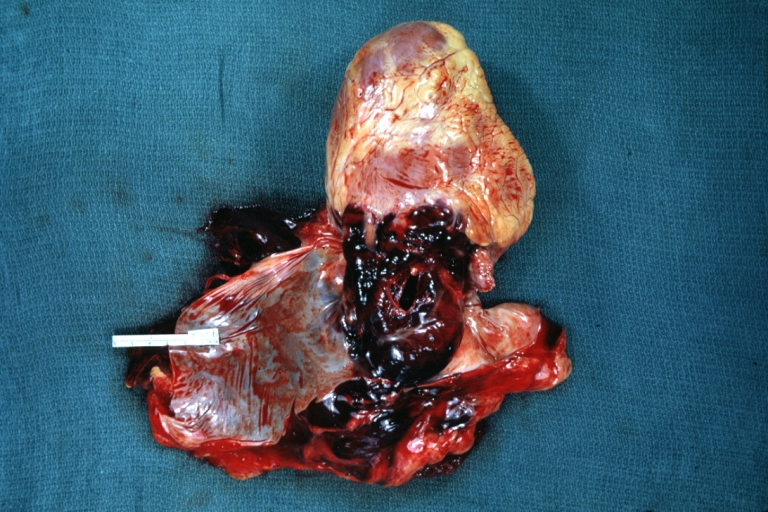
Image:Aortic aneurysm 14.jpg|Dissecting [[Aneurysm]]: Gross, heart with root of [[aorta]] to show [[hemorrhage]] into [[pericardium]] (a very good example). | |||
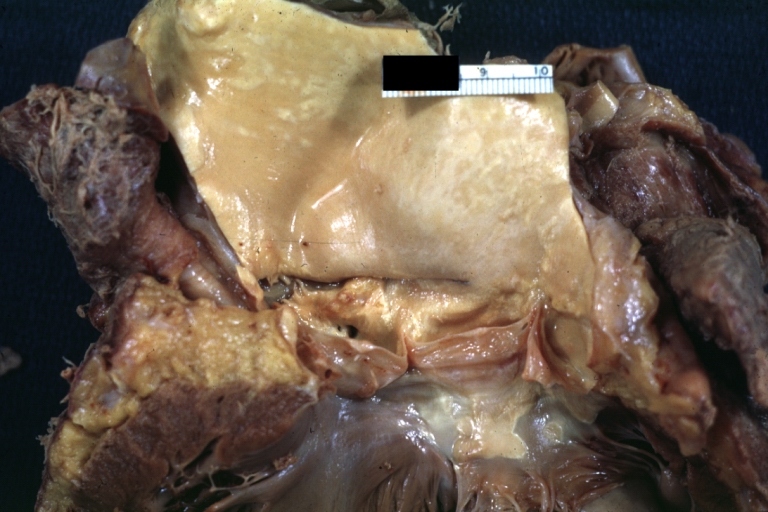
Image:Aortic aneurysm 15.jpg|Dissecting [[Aneurysm]]: Gross, of heart and [[aorta]] with dissection and large false channel (a good example). | |||
Image:Aortic aneurysm 16.jpg|Dissecting [[Aneurysm]]: Gross cross section of [[aorta]] with two channels (a good example). | |||
Image:Aortic aneurysm 19.jpg|Dissecting [[Aneurysm]]: Gross good example angular tear above [[aortic valve]]. | |||
</gallery> | |||
</div> | |||
<div align="left"> | |||
<gallery heights="175" widths="175"> | |||
Image:Aortic aneurysm 18.jpg|Dissecting [[Aneurysm]]: Gross good example of typical angular tear above [[aortic valve]]. | |||
Image:Aortic aneurysm 25.jpg|Dissecting [[Aneurysm]]: Gross, rather well shown dissection in first portion of the [[aortic arch]] | |||
Image:Aortic aneurysm 26.jpg|Dissecting [[Aneurysm]]: Gross, rather well shown dissection in first portion of the [[aortic arch]] | |||
Image:Aortic aneurysm 27.jpg|Dissecting [[Aneurysm]]: Gross, an excellent example of type I [[lesion]] | |||
</gallery> | |||
</div> | |||
[[ | <div align="left"> | ||
<gallery heights="175" widths="175"> | |||
Image:Aortic aneurysm 28.jpg|Dissecting [[Aneurysm]]: Gross, external view, an excellent example | |||
Image:Aortic aneurysm 29.jpg|Dissecting [[Aneurysm]]: Gross, Type I shows false channel | |||
Image:Aortic aneurysm 30.jpg|Dissecting [[Aneurysm]]: Gross, opened to show false channel (good example) | |||
Image:Aortic aneurysm 36.jpg|Dissecting [[Aneurysm]]: Gross, large tear in first portion of [[aortic arch]], [[annuloaortic ectasia]] | |||
</gallery> | |||
</div> | |||
[[ | <div align="left"> | ||
<gallery heights="175" widths="175"> | |||
Image:Aortic aneurysm 32.jpg|Dissecting [[Aneurysm]]: Gross, coagulum of blood in false channel | |||
Image:Aortic aneurysm 33.jpg|Dissecting [[Aneurysm]]: Gross, [[aortic valve]] area dissection (well shown, typical lesion) | |||
Image:Aortic aneurysm 37.jpg|Dissecting [[Aneurysm]]: Gross, external view of heart and first portion of [[aortic arch]], [[annuloaortic ectasia]], [[hemorrhage]] beneath [[adventitia]] is evidence of dissection | |||
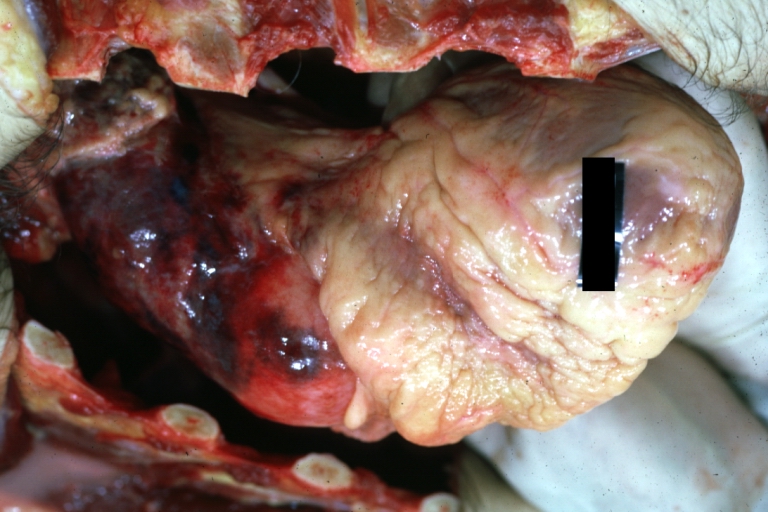
Image:Aortic aneurysm 41.jpg|Dissecting [[Aneurysm]] in a patient with [[Marfan's syndrome]] | |||
</gallery> | |||
</div> | |||
<div align="left"> | |||
<gallery heights="175" widths="175"> | |||
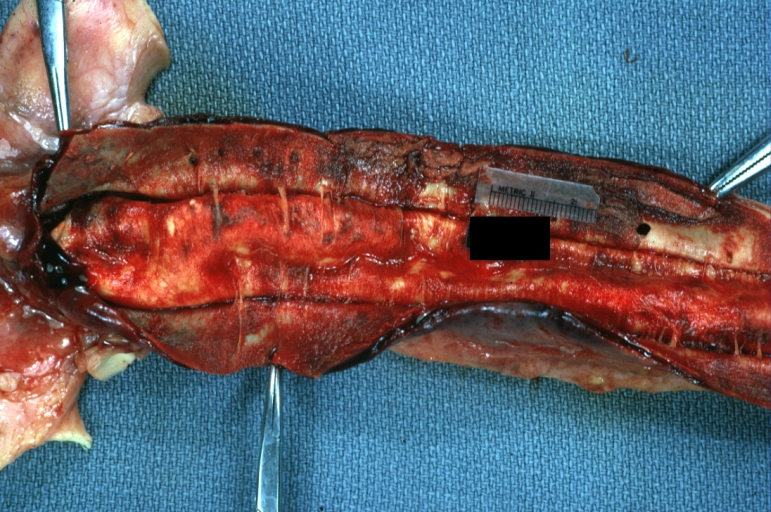
Image:Aortic aneurysm 44.jpg|Dissecting [[Aneurysm]]: Gross, fixed tissue, [[descending aorta|descending]] [[thoracic aorta|thoracic]] segment dissection opened to show the false channel. The true surface is also visible | |||
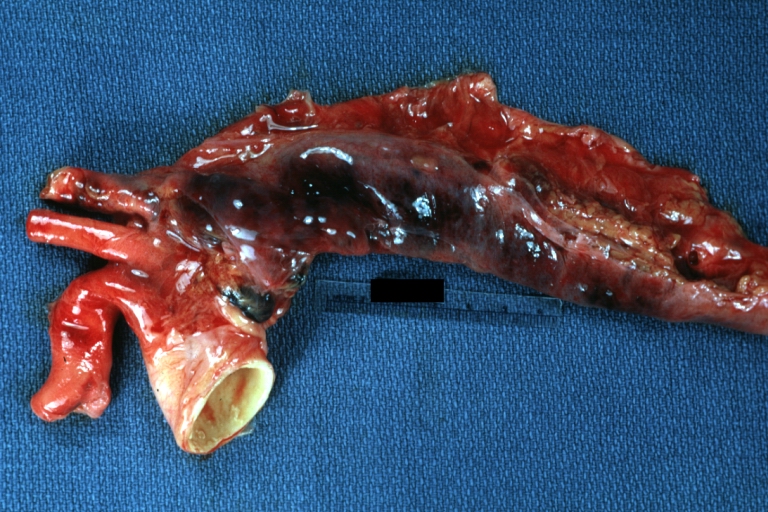
Image:Aortic aneurysm 48.jpg|Dissecting [[Aneurysm]]: Gross natural color [[descending aorta]] opened into false channel | |||
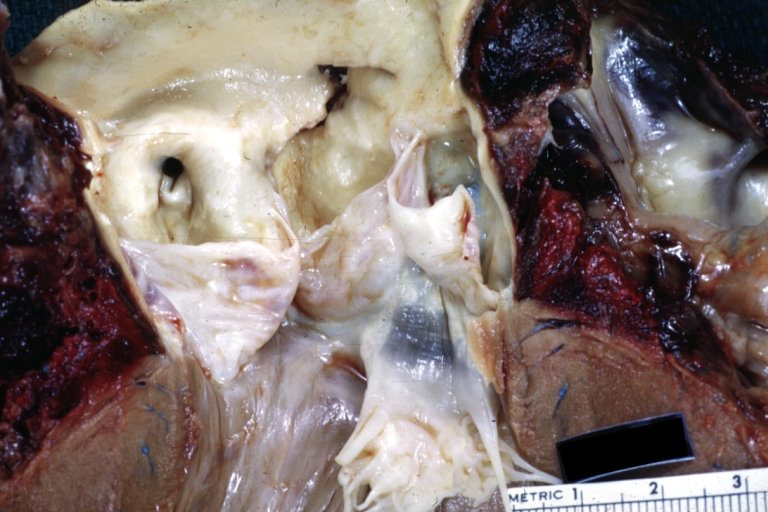
Image:Aortic aneurysm 59.jpg|Dissecting [[Aneurysm]]: Gross natural color close-up view of [[aortic valve]] and [[proximal]] [[aortic arch]] with ruptured [[intima]] rather good illustration of this [[lesion]] | |||
Image:Aortic aneurysm 62.jpg|Dissecting [[Aneurysm]] [[Chronic]]: Gross natural color first portion of [[aortic arch]] with [[intima]]l rent well shown with healed margins and view into false channel that shows a surface looking like [[atherosclerosis]] which is known to develop in a [[chronic]] dissection | |||
Image:Aortic aneurysm 63.jpg|Dissecting [[Aneurysm]] [[Chronic]]: Gross, natural color, closer view of the previous one (a very good example) | |||
</gallery> | |||
</div> | |||
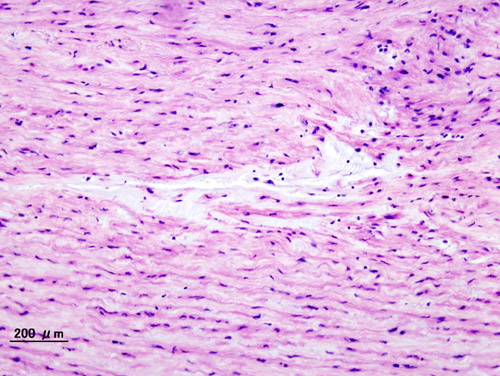
==Microscopic Pathology== | |||
{| align="left" | |||
|[[File:Aortic dissection (2).jpg|thumb|none|200px|<ref>Case courtesy of Wikimedia Commons</ref>]] | |||
|} | |||
== References == | == References == | ||
| Line 49: | Line 145: | ||
{{WH}} | {{WH}} | ||
{{WS}} | {{WS}} | ||
[[CME Category::Cardiology]] | |||
[[Category:Cardiology]] | [[Category:Cardiology]] | ||
[[Category:Emergency medicine]] | [[Category:Emergency medicine]] | ||
[[Category:Intensive care medicine]] | |||
[[Category:Up-To-Date]] | |||
[[Category:Up-To-Date cardiology]] | |||
[[Category:Best pages]] | |||
Latest revision as of 18:07, 21 January 2020
|
Aortic dissection Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Special Scenarios |
|
Case Studies |
|
|
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Cafer Zorkun, M.D., Ph.D. [2] Sahar Memar Montazerin, M.D.[3]
Overview
Aortic dissection begins as a tear in the aortic wall in > 95% of patients. The tear is usually transverse, extends through the intima and halfway through the media and involves ~50% of the aortic circumference. Two thirds of dissections originate in the ascending aorta, and 20% are in the proximal descending aorta.
Pathophysiology
Normal Anatomy of the Aorta
As with all other arteries, the aorta is made up of three layers. The layer that is in direct contact with the flow of blood is the tunica intima, commonly called the intima. This layer is made up of mainly endothelial cells. Just deep to this layer is the tunica media, known as the media. This middle layer is made up of smooth muscle cells and elastic tissue. The outermost layer (furthest from the flow of blood) is known as the tunica adventitia or the adventitia. This layer is composed of connective tissue.
Pathogenesis
Initial Intimal Tear
- Aortic dissection begins as a tear in the aortic wall in > 95% of patients.
- It is usually transverse, extends through the intima and halfway through the media and involves ~50% of the aortic circumference.
Location of Dissections
- The initial tear is usually within 100 mm of the aortic valve.
- 65% of dissections originate in the ascending aorta, distal to the aortic valve and coronary ostia
- 10% arise in the transverse aortic arch
- 20% in the proximal descending aorta
- 5% in the more distal descending aorta
Propagation of the Intimal Tear
In an aortic dissection, blood penetrates the intima and enters the media layer. The high pressure rips the tissue of the media apart, allowing more blood to enter. This can propagate along the length of the aorta for a variable distance, dissecting either towards or away from the heart or both.
Once a tear develops, blood then passes into the media, and a false lumen is dissected in the outer layer of aortic media involving ~50% of the aortic circumference. This false lumen can enlarge, and compress the true lumen, as well as extend proximally or distally and occlude aortic branches. For some unknown reason, the right lateral wall of the ascending aorta is the most common site for dissection. The right coronary artery can become occluded as a result of this propagation.
Separating the false lumen from the true lumen is a layer of intimal tissue. This tissue is known as the intimal flap. As blood flows down the false lumen, it may cause secondary tears in the intima. Through these secondary tears, the blood can re-enter the true lumen.
Aortic Dissection in the Absence of an Intimal Tear
In about 13% of aortic dissections, there is no evidence of an intimal tear. It is believed that in these cases the inciting event is an intramural hematoma (caused by hemorrhage within the media). Since there is no direct connection between the true lumen and the false lumen in these cases, it is difficult to diagnose an aortic dissection by aortography if the etiology is an intramural hematoma. An aortic dissection secondary to an intramural hematoma should be treated the same as one caused by an intimal tear.
An aortic intramural hematoma can form when the vasa vasorum ruptures into the aortic wall. This is distinguished from dissection by the lack of an intimal tear. This disorder parallels aortic dissection in terms of prognosis when the ascending aorta or aortic arch is involved, and rapid surgical intervention is indicated. Involvement of the descending aorta, however, carries a better prognosis than dissection, and outcome tends to be similar with medical or surgical therapy.
Genetics
Genes involved in the pathogenesis of aortic dissection include:[1][2]
- FBN1 (fibrillin-1)
- LOX (lysyl oxidase)
- MYH11 (smooth muscle myosin heavy chain 11)
- ACTA2 (smooth muscle α-actin 2)
- MYLK (myosin light chain kinase)
- PRKG1 (protein kinase cGMP-dependent type 1)
- COL3A1 (α-1 procollagen, type III)
- TGFBR1 (TGF-β receptor type I)
- TGFBR2 (TGF-β receptor type II)
- TGFB2
- SMAD3 (mothers against decapentaplegic drosophila homolog 3)
Associated Conditions
Conditions associated with aortic dissection include:[1]
- Aortic aneurysm
- Smooth muscle dysfunction syndrome
- Marfan syndrome
- Vascular Ehlers-Danlos syndrome
- Loeys-Dietz syndromes
Gross Pathology
-
Dissecting Aneurysm: Gross fixed tissue external view of heart aortic arch and descending aorta showing dilated first and second portion of arch from anterior projection.
-
Dissecting Aneurysm: Gross very good example dissected channel has been opened.
-
Dissecting Aneurysm: Gross external view good appearance from adventitia.
-
Dissecting Aneurysm: Gross opened false channel.
-
Dissecting Aneurysm: Gross good example dissection beginning at third portion aortic arch.
-
Dissecting Aneurysm: Gross cross sections showing thrombus in false lumen. True lumen has been opened longitudinally.
-
Dissecting Aneurysm: Gross shows origin just above aortic valve false channel shown in descending thoracic aorta (very good example).
-
Dissecting Aneurysm: Gross, an excellent example, starting just above the aortic valve with reflection of aorta to show the dissection tract and some thrombus
-
Dissecting Aneurysm: Gross shows dilated aorta with extensive atherosclerosis dissection is seen, a small abdominal aorta atherosclerotic aneurysm is present good for association of dilation with dissection
-
Dissecting Aneurysm: Gross arrow points to start of dissection in first portion aortic arch good but not the best example shows dilation
-
Dissecting Aneurysm: Gross, very good to show start of dissection above aortic valve and blood in false channel.
-
Dissecting Aneurysm: Gross, heart with root of aorta to show hemorrhage into pericardium (a very good example).
-
Dissecting Aneurysm: Gross good example angular tear above aortic valve.
-
Dissecting Aneurysm: Gross good example of typical angular tear above aortic valve.
-
Dissecting Aneurysm: Gross, rather well shown dissection in first portion of the aortic arch
-
Dissecting Aneurysm: Gross, rather well shown dissection in first portion of the aortic arch
-
Dissecting Aneurysm: Gross, external view, an excellent example
-
Dissecting Aneurysm: Gross, Type I shows false channel
-
Dissecting Aneurysm: Gross, opened to show false channel (good example)
-
Dissecting Aneurysm: Gross, large tear in first portion of aortic arch, annuloaortic ectasia
-
Dissecting Aneurysm: Gross, coagulum of blood in false channel
-
Dissecting Aneurysm: Gross, aortic valve area dissection (well shown, typical lesion)
-
Dissecting Aneurysm: Gross, external view of heart and first portion of aortic arch, annuloaortic ectasia, hemorrhage beneath adventitia is evidence of dissection
-
Dissecting Aneurysm in a patient with Marfan's syndrome
-
Dissecting Aneurysm: Gross, fixed tissue, descending thoracic segment dissection opened to show the false channel. The true surface is also visible
-
Dissecting Aneurysm: Gross natural color descending aorta opened into false channel
-
Dissecting Aneurysm: Gross natural color close-up view of aortic valve and proximal aortic arch with ruptured intima rather good illustration of this lesion
-
Dissecting Aneurysm Chronic: Gross natural color first portion of aortic arch with intimal rent well shown with healed margins and view into false channel that shows a surface looking like atherosclerosis which is known to develop in a chronic dissection
Microscopic Pathology
 |
References
- ↑ 1.0 1.1 Pinard, Amélie; Jones, Gregory T.; Milewicz, Dianna M. (2019). "Genetics of Thoracic and Abdominal Aortic Diseases". Circulation Research. 124 (4): 588–606. doi:10.1161/CIRCRESAHA.118.312436. ISSN 0009-7330.
- ↑ Verhagen, Judith M.A.; Kempers, Marlies; Cozijnsen, Luc; Bouma, Berto J.; Duijnhouwer, Anthonie L.; Post, Jan G.; Hilhorst-Hofstee, Yvonne; Bekkers, Sebastiaan C.A.M.; Kerstjens-Frederikse, Wilhelmina S.; van Brakel, Thomas J.; Lambermon, Eric; Wessels, Marja W.; Loeys, Bart L.; Roos-Hesselink, Jolien W.; van de Laar, Ingrid M.B.H. (2018). "Expert consensus recommendations on the cardiogenetic care for patients with thoracic aortic disease and their first-degree relatives". International Journal of Cardiology. 258: 243–248. doi:10.1016/j.ijcard.2018.01.145. ISSN 0167-5273.
- ↑ Case courtesy of Wikimedia Commons