ST elevation myocardial infarction case study two
|
ST Elevation Myocardial Infarction Microchapters |
|
Differentiating ST elevation myocardial infarction from other Diseases |
|
Diagnosis |
|
Treatment |
|
|
Case Studies |
|
ST elevation myocardial infarction case study two On the Web |
|
ST elevation myocardial infarction case study two in the news |
|
Directions to Hospitals Treating ST elevation myocardial infarction |
|
Risk calculators and risk factors for ST elevation myocardial infarction case study two |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Case 2
Medical History, Clinical and Laboratory Findings
A 78-year-old male experienced a posterior myocardial infarction six years prior to this admission.
Recently, he had begun to experience occasional angina.
Four days prior to death, he experienced anterior chest pain and discomfort which he regarded as not too distressing.
However, EKGs showed a classic acute anterior myocardial infarction in addition to the healed posterior infarct.
The patient progressively deteriorated with left ventricular failure and died with arrhythmias and pulmonary edema. Pertinent laboratory data are:
- Aspartate aminotransferase (AST) 60 IU/L.
- Total creatine phosphokinase (CPK) 165 IU/L. All of the activity was due to CPK III (MM) isoenzyme fraction; no CPK (MB) activity was detectable.
- Lactate dehydrogenase (LDH) 720 IU/L. LD1 fraction was greater than LD2.
Autopsy Findings
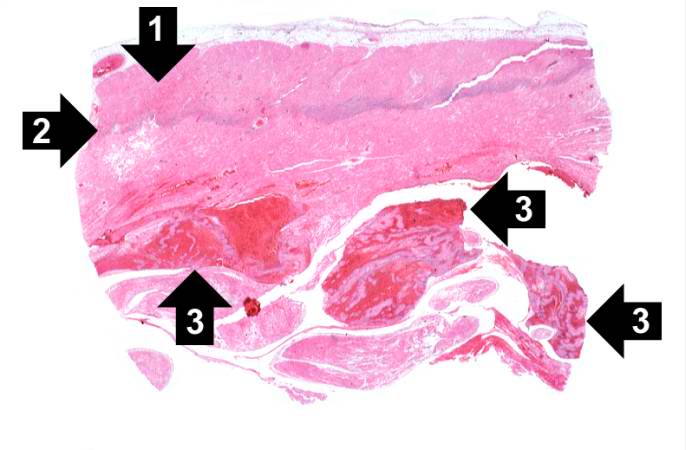
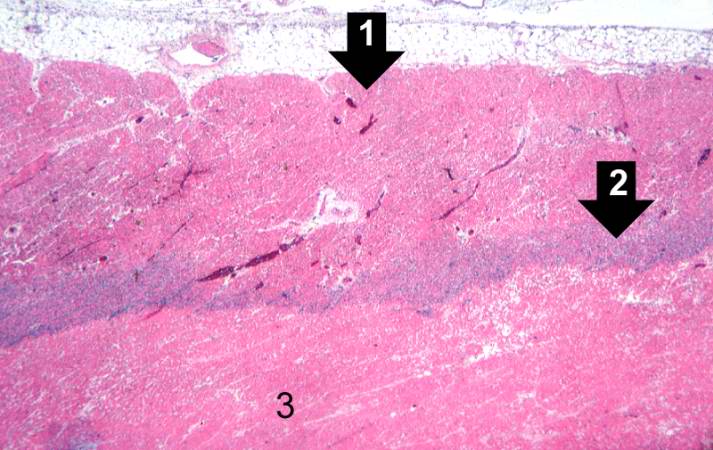
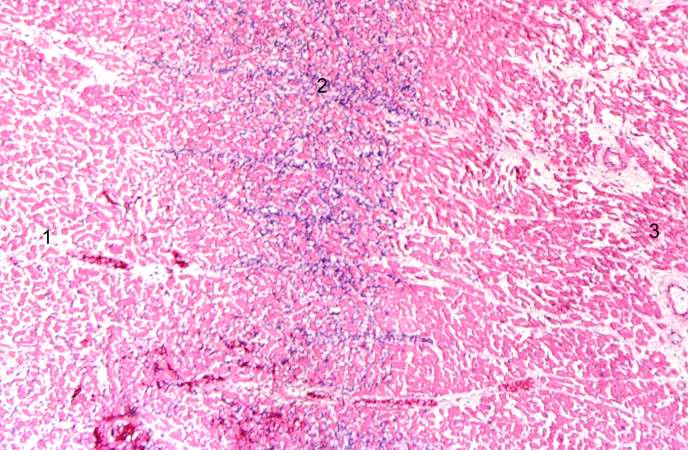
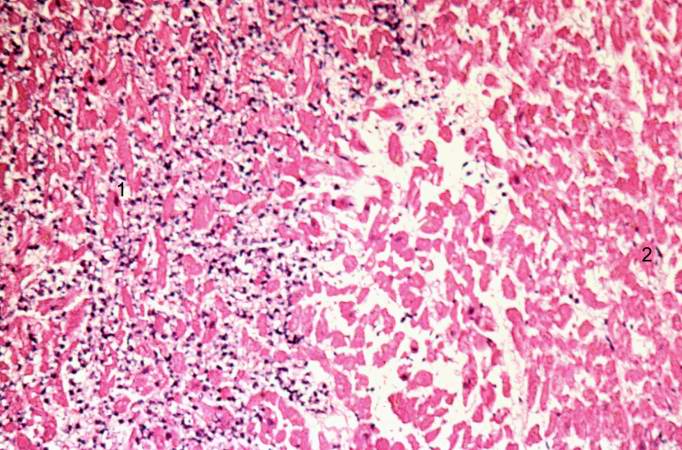
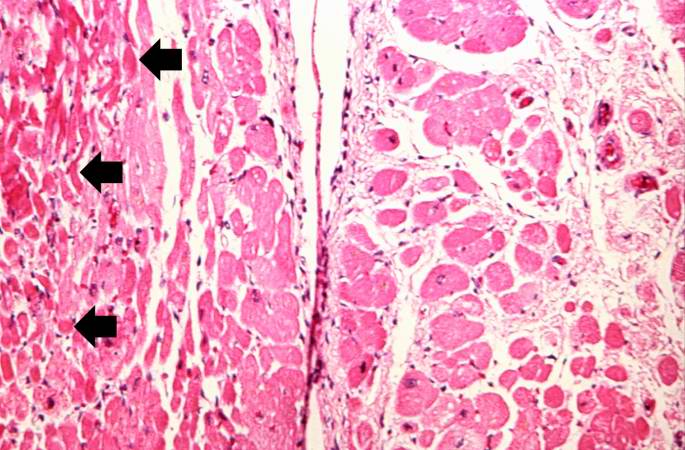
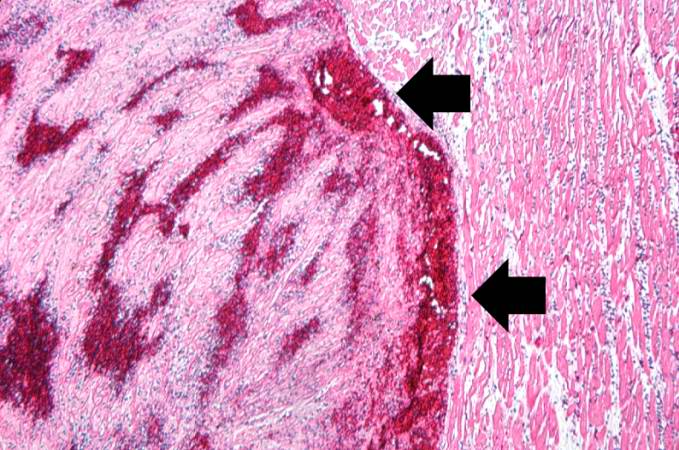
Examination of the heart showed a healed posterior infarct. The right coronary artery was completely occluded but partially recanalized. The left main coronary artery had severe atherosclerotic stenosis and a thrombus filling the lumen. The entire anterolateral aspect of the left ventricle was soft with variegated areas appearing hyperemic or pale.
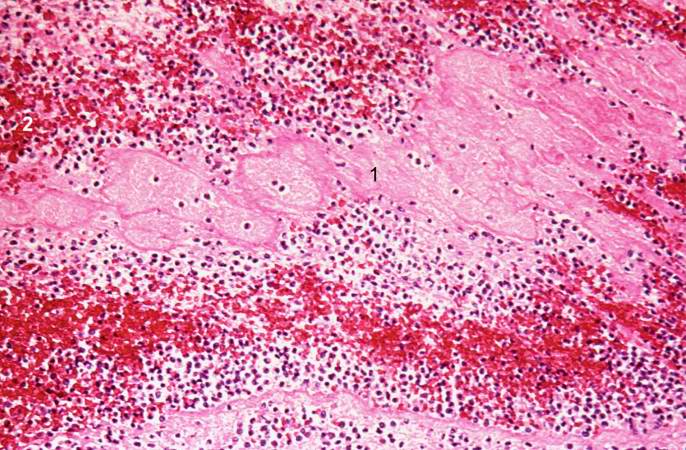
There was extensive mural thrombosis and reactive pericarditis.
Histopathologic Findings