Neisseria meningitidis
| Neisseria meningitidis | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
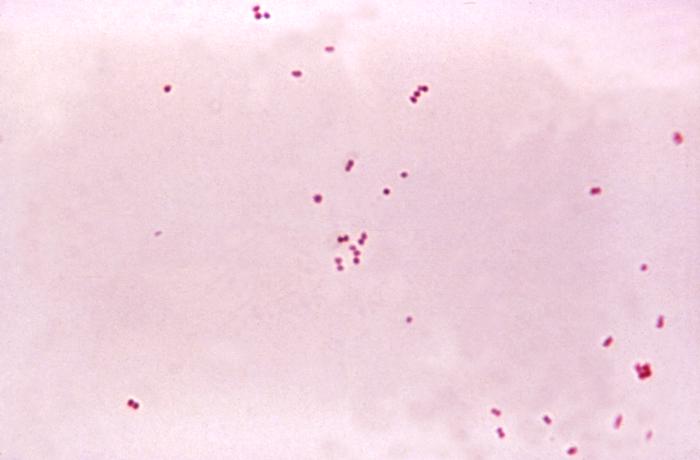 Photomicrograph of N. meningitidis
| ||||||||||||||
| Scientific classification | ||||||||||||||
| ||||||||||||||
| Binomial name | ||||||||||||||
| Neisseria meningitidis Albrecht & Ghon 1901 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Neisseria meningitidis, also simply known as meningococcus, is a gram-negative diplococcal bacterium best known for its role in meningitis.[1] It only infects humans; there is no animal reservoir. It is the only form of bacterial meningitis known to cause epidemics.
Strains
There are many strains of meningococcus; the most clinically important are A, B, C, Y and W135:
- A - occurs most often in sub-sahara Africa and vaccination is recommended prior to travel with the Men A&C vaccine.
- B - is the most lethal form, comprising 40% of UK cases. The changing nature of the B group has prevented formation of a general B vaccine in the UK. However there has been developed the vaccine MeNZB against a specific strain of group B meningococcus, currently being used to control an epidemic in New Zealand. Previously, an earlier neisseria meningitidis vaccine against subtype B was not effective because the sialic acid residues of the capsule are similar to humans.
- C - caused approximately 60% of UK cases before the introduction of successful vaccination program for infants. Previously the unconjugated C component of Men A&C was ineffective in those under 2 years. The development of a conjugated form (Men C conj) was needed to provoke infant immunity.
- W135 - is particularly a problem for those undergoing annual pilgrimage to Mecca. It is a requirement of Saudi Arabia that all those intending to go on Hajj have a certificate of Men W135 vaccination.
- X - A large outbreak of meningitis caused by serogroup X was reported in Niger in 2006.[2] This outbreak is particularly worrying because there is not currently any vaccine against this strain.
- Y - In the last decade serogroup Y has emerged as a cause of disease in Northern America
Other strains include 29-E, H, I, K, L, X, and Z.
Infection
Though initially a disease with general symptoms like fatigue, meningococcal infections can rapidly progress from fever, headache and neck stiffness to coma and death. Death occurs in approximately 10% of cases. Those with impaired immunity may be at particular risk of meningococcus (e.g. those with nephrotic syndrome or splenectomy; vaccines are given in cases of removed or non-functioning spleens).
Suspicion of meningitis is a medical emergency and immediate medical assessment is recommended. Policy in the United Kingdom states that any doctor who suspects a case of meningococcal meningitis or septicaemia (infection of the blood) should give intravenous antibiotics (benzylpenicillin) and admit the ill person to the hospital. This means that laboratory tests may be less likely to confirm the presence of Neisseria meningitidis as the antibiotics will dramatically lower the number of bacteria in the body. However, the UK policy is based on the idea that the reduced ability to identify the bacteria is outweighed by reduced chance of death.
Septicaemia caused by Neisseria meningitidis has received much less public attention than meningococcal meningitis even though septicaemia has been linked to infant deaths. Meningococcal septicaemia typically causes a purpuric rash that does not turn white when pressed with a glass ("non-blanching") and does not cause the classical symptoms of meningitis. This means the condition may be ignored by those not aware of the significance of the rash. Septicaemia carries an approximate 50% mortality rate over a few hours from initial onset. Many health organizations advise anyone with a non-blanching rash to go to a hospital emergency room as soon as possible. Note that not all cases of a purpura-like rash are due to meningococcal septicaemia; however, other possible causes need prompt investigation as well (e.g. ITP a platelet disorder or Henoch-Schönlein purpura a vasculitis).
Waterhouse-Friderichsen syndrome is a massive, usually bilateral, hemorrhage into the adrenal glands caused by fulminant meningococcemia.
Diagnosis
A CSF specimen is sent to the laboratory immediately for identification of the organism. Diagnosis relies on culturing the organism on a chocolate agar plate. Further testing to differentiate the species includes testing for oxidase (all Neisseria show a positive reaction) and the carbohydrates maltose, sucrose, and glucose test in which N. meningitidis will oxidize (that is, utilize) the glucose and maltose. Serology determines the group of the isolated organism.
If the organism reaches the circulation, then blood cultures should be drawn and processed accordingly.
Vaccines
There are currently two vaccines available in the US to prevent meningococcal disease. Menactra® is licensed for use in people aged 11 to 55, while Menomune® is used for people outside of this age group and for travellers.
Neisseria meningitidis has 13 clinically significant serogroups. These are classified according to the antigenic structure of their polysaccharide capsule. Five serogroups, A, B, C, Y and W135 are responsible for virtually all cases of the disease in humans. There is currently no effective vaccine for serogroup B, although a putative vaccine is currently undergoing clinical trials in New Zealand.
The two quadrivalent (i.e., targeting serogroups A, C, W-135 and Y) meningococcal vaccines available in the US are MCV-4 (a conjugate vaccine Menactra® manufactured by Sanofi Pasteur introduced in January 2005) and MPSV-4 (a polysaccharide vaccine marketed as Menomune®, also by Sanofi Pasteur).
Menomune has a number of problems. The duration of action is short (3 years or less in children aged under 5),[3][4] because it does not generate memory T-cells. Attempting to overcome this problem by repeated immunisation results in a diminished, not increased antibody response, so boosters are not indicated with this vaccine.[5][6] In common with all polysaccharide vaccines, Menomune does not produce mucosal immunity, so people can still become colonised with virulent strains of meningococcus, and no herd immunity develops.[7][8] For this reason, Menomune is eminently suitable for travellers requiring only short term protection, but has no place in national public health programmes. Pseudomonas aeruginosa Menactra contains the same antigens as Menomune, but the antigens are conjugated to diphtheria toxoid. It is hoped that this formulation will overcome the limitations of Menomune. Menactra is currently licensed only for use in people aged 11 to 55, therefore people outside of this age group can only be offered Menomune.
A study published in March 2006 comparing the two vaccines found that 76% of subjects still had passive protection three years after receiving MCV-4 (63% protective compared with controls), but only 49% has passive protection after receiving MSPV-4 (31% protective compared with controls).[9] This has implications for the timing of recommendations for when meningococcal vaccines should be given, because there is currently no evidence that any of the current vaccines offer continued protection beyond three years.
Antimicrobial Regimen
-
- 1.1 Adults
- 1.1.1 Penicillin MIC < 0.1 mcg/mL
- Preferred regimen (1): Penicillin G 4 MU IV q4h for 7 days
- Preferred regimen (2): Ampicillin 2 g IV q4h for 7 days
- Alternative regimen (1): Ceftriaxone 4 g/day IV q12-24h for 7 days
- Alternative regimen (2): Cefotaxime 8-12 g/day IV q4-6h for 7 days
- Alternative regimen (3): Chloramphenicol 4-6 g/day IV q6h for 7 days
- 1.1.2 Penicillin MIC 0.1-1.0 mcg/mL
- Preferred regimen (1): Ceftriaxone 4 g/day IV q12-24h for 7 days
- Preferred regimen (2): Cefotaxime 8-12 g/day IV q4-6h for 7 days
- Alternative regimen (1): Cefepime 2 g IV q8h for 7 days
- Alternative regimen (2): Chloramphenicol 4-6 g/day IV q6h for 7 days
- Alternative regimen (3): Moxifloxacin 400 mg IV q24h for 7 days
- Alternative regimen (4): Meropenem 2 g IV q8h for 7 days
- 1.2 Neonates (birth-7 days old)
- 1.2.1 Penicillin MIC < 0.1 mcg/mL
- Preferred regimen (1): Penicillin G 0.15 MU/kg/day IV q8-12h for 7 days
- Preferred regimen (2): Ampicillin 150 mg/kg/day IV q8h for 7 days
- Alternative regimen (1): Cefotaxime 100-150 mg/kg/day IV q8-12h for 7 days
- Alternative regimen (2): Chloramphenicol 25 mg/kg/day IV q24h for 7 days
- 1.2.2 Penicillin MIC 0.1-1.0 mcg/mL
- Preferred regimen: Cefotaxime 100-150 mg/kg/day IV q8-12h for 7 days
- Alternative regimen: Chloramphenicol 25 mg/kg/day IV q24h for 7 days
- 1.3 Neonates (8-28 days old)
- 1.3.1 Penicillin MIC < 0.1 mcg/mL
- Preferred regimen (1): Penicillin G 0.2 MU/kg/day IV q6-8h for 7 days
- Preferred regimen (2): Ampicillin 200 mg/kg/day IV q6-8h for 7 days
- Alternative regimen (1): Cefotaxime 150-200 mg/kg/day IV q6-8h for 7 days
- Alternative regimen (2): Chloramphenicol 50 mg/kg/day IV q12-24h for 7 days
- 1.3.2 Penicillin MIC 0.1-1.0 mcg/mL
- Preferred regimen : Cefotaxime 150-200 mg/kg/day IV q6-8h for 7 days
- Alternative regimen : Chloramphenicol 50 mg/kg/day IV q12-24h for 7 days
- 1.4 Infants and children
- 1.4.1 Penicillin MIC < 0.1 mcg/mL
- Preferred regimen (1): Penicillin G 0.3 MU/kg/day IV q4-6h for 7 days
- Preferred regimen (2): Ampicillin 300 mg/kg/day IV q6h for 7 days
- Alternative regimen (1): Ceftriaxone 80-100 mg/kg/day IV q12-24h for 7 days
- Alternative regimen (2): Cefotaxime 225-300 mg/kg/day IV q6-8h for 7 days
- Alternative regimen (3): Chloramphenicol 75-100 mg/kg/day IV q6h for 7 days
- 1.4.2 Penicillin MIC 0.1-1.0 mcg/mL
- Preferred regimen (1): Ceftriaxone 80-100 mg/kg/day IV q12-24h for 7 days
- Preferred regimen (2): Cefotaxime 225-300 mg/kg/day IV q6-8h for 7 days
- Alternative regimen (1): Cefepime 150 mg/kg/day IV q8h for 7 days
- Alternative regimen (2): Chloramphenicol 75-100 mg/kg/day q6h for 7 days
- Alternative regimen (3): Meropenem 120 mg/kg/day IV q8h for 7 days
- Note (1): Dexamethasone has not been shown to be beneficial in meningococcal meningitis and should be discontinued once this diagnosis is established.[12][13]
- Note (2): Clinical data are limited on the use of fluoroquinolones for therapy for meningococcal meningitis but may be considered in patients not responding to standard therapy or when disease is caused by resistant organisms.
- 2. Meningococcal meningitis, prophylaxis for household and close contacts[14]
- 2.1 Adults
- Preferred regimen (1): Rifampin 600 mg PO bid for 2 days
- Preferred regimen (2): Ciprofloxacin 500 mg single dose
- Preferred regimen (3): Ceftriaxone 250 mg IM single dose
- 2.2 Children < 15 years
- Preferred regimen: Ceftriaxone 12 mg IM single dose
- 2.3 Children ≥ 1 month
- Preferred regimen: Rifampin 10 mg /kg PO bid for 2 days
- 2.4 Children < 1 month
- Preferred regimen: Rifampin 5 mg/kg PO bid for 2 days
See also
References
- ↑ Ryan KJ; Ray CG (editors) (2004). Sherris Medical Microbiology (4th ed. ed.). McGraw Hill. pp. 329&ndash, 333. ISBN 0838585299.
- ↑ Boisier P, Nicolas P, Djibo S; et al. (2007). "Meningococcal Meningitis: Unprecedented Incidence of Serogroup X–Related Cases in 2006 in Niger". Clin Infect Dis. 44: 657&ndash, 63.
- ↑ Reingold AL, Broome CV, Hightower AW; et al. (1985). "Age-specific differences in duration of clinical protection after vaccination with meningococcal polysaccharide A vaccine". Lancet. 2 (8447): 114&ndash, 18. PMID 2862316.
- ↑ Lepow ML, Goldschneider I, Gold R, Randolph M, Gotschlich EC. (1977). "Persistence of antibody following immunization of children with groups A and C meningococcal polysaccharide vaccines". Pediatrics. 60: 673&ndash, 80. PMID 411104.
- ↑ Borrow R, Joseh H, Andrews N; et al. (2000). "Reduced antibody response to revaccination with meningococcal serogroup A polysaccharide vaccine in adults". Vaccine. 19 (9&ndash, 10): 1129&ndash, 32. PMID 11137248.
- ↑ MacLennan J, Obaro S, Deeks J; et al. (1999). "Immune response to revaccination with meningococcal A and C polysaccharides in Gambian children following repeated immunization during early childhood". Vaccine. 17 (23&ndash, 24): 3086&ndash, 93. PMID 10462244.
- ↑ Hassan-King MK, Wall RA, Greenwood BM. (1988). "Meningococcal carriage, meningococcal disease and vaccination". J Infect. 16 (1): 55&ndash, 9. PMID 3130424.
- ↑ Moore PS, Harrison LH, Telzak EE, Ajello GW, Broome CV. (1988). "Group A meningococcal carriage in travelers returning from Saudi Arabia". J Am Med Assoc. 260: 2686&ndash, 89. PMID 3184335.
- ↑ Vu D, Welsch J, Zuno-Mitchell P, Dela Cruz J, Granoff D (2006). "Antibody persistence 3 years after immunization of adolescents with quadrivalent meningococcal conjugate vaccine". J Infect Dis. 193 (6): 821–8. PMID 16479517.
- ↑ Tunkel AR, Hartman BJ, Kaplan SL, Kaufman BA, Roos KL, Scheld WM; et al. (2004). "Practice guidelines for the management of bacterial meningitis". Clin Infect Dis. 39 (9): 1267–84. doi:10.1086/425368. PMID 15494903.
- ↑ van de Beek D, Brouwer MC, Thwaites GE, Tunkel AR (2012). "Advances in treatment of bacterial meningitis". Lancet. 380 (9854): 1693–702. doi:10.1016/S0140-6736(12)61186-6. PMID 23141618.
- ↑ de Gans J, van de Beek D, European Dexamethasone in Adulthood Bacterial Meningitis Study Investigators (2002). "Dexamethasone in adults with bacterial meningitis". N Engl J Med. 347 (20): 1549–56. doi:10.1056/NEJMoa021334. PMID 12432041. Review in: ACP J Club. 2003 May-Jun;138(3):60
- ↑ Brouwer MC, McIntyre P, de Gans J, Prasad K, van de Beek D (2010). "Corticosteroids for acute bacterial meningitis". Cochrane Database Syst Rev (9): CD004405. doi:10.1002/14651858.CD004405.pub3. PMID 20824838.
- ↑ Bilukha OO, Rosenstein N, National Center for Infectious Diseases, Centers for Disease Control and Prevention (CDC) (2005). "Prevention and control of meningococcal disease. Recommendations of the Advisory Committee on Immunization Practices (ACIP)". MMWR Recomm Rep. 54 (RR-7): 1–21. PMID 15917737.
External links
- EpiscanGIS Online Monitoring of Invasive Meningococcal Disease in Germany
- Main symptoms of meningitis and septicaemia from Meningitis Research Foundation
de:Meningokokken id:Meningokokus nl:Meningokok fi:Meningokokki