Lanreotide
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Rabin Bista, M.B.B.S. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Lanreotide is a somatostatin analog that is FDA approved for the treatment of acromegalic patients who have had an inadequate response to or cannot be treated with surgery and/or radiotherapy. Common adverse reactions include diarrhea, cholelithiasis, abdominal pain, nausea and injection site reactions.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indications
- Somatuline Depot (lanreotide) Injection 60 mg, 90 mg and 120 mg is indicated for the long-term treatment of acromegalic patients who have had an inadequate response to surgery and/or radiotherapy, or for whom surgery and/or radiotherapy is not an option.
- The goal of treatment in acromegaly is to reduce growth hormone (GH) and insulin growth factor-1 (IGF-1) levels to normal.
Dosage
- Patients should begin treatment with Somatuline Depot 90 mg given via the deep subcutaneous route, at 4 week intervals for 3 months.
- After 3 months dosage may be adjusted as follows:
- GH >1 to ≤ 2.5 ng/mL, IGF-1 normal and clinical symptoms controlled: maintain Somatuline Depot dose at 90 mg every 4 weeks.
- GH > 2.5 ng/mL, IGF-1 elevated and/or clinical symptoms uncontrolled, increase Somatuline Depot dose to 120 mg every 4 weeks.
- GH ≤ 1 ng/mL, IGF-1 normal and clinical symptoms controlled: reduce Somatuline Depot dose to 60 mg every 4 weeks.
- Thereafter, the dose should be adjusted according to the response of the patient as judged by a reduction in serum GH and /or IGF-1 levels; and/or changes in symptoms of acromegaly.
- Somatuline Depot should be injected via the deep subcutaneous route in the superior external quadrant of the buttock. The skin should not be folded and the needle should be inserted perpendicular to the skin, rapidly and to its full length. The injection site should alternate between the right and left side.
- The starting dose in patients with moderate and severe renal or moderate and severe hepatic impairment should be 60 mg via the deep subcutaneous route, at 4 week intervals for 3 months followed by dose adjustment as described above
DOSAGE FORMS AND STRENGTHS
- 60, 90 and 120 mg sterile, single-use, pre-filled syringes. The pre-filled syringes contain a white to pale yellow, semi-solid formulation.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Lanreotide in adult patients.
Non–Guideline-Supported Use
- Portal hypertension[1]
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding FDA-Labeled Use of Lanreotide in pediatric patients.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Lanreotide in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Lanreotide in pediatric patients.
Contraindications
- None
Warnings
Cholethiasis and Gallbladder Sludge
Lanreotide may reduce gallbladder motility and lead to gallstone formation therefore, patients may need to be monitored periodically.
Hyperglycemia and Hypoglycemia
- Pharmacological studies in animals and humans show that lanreotide, like somatostatin and other somatostatin analogs, inhibits the secretion of insulin and glucagon. Hence, patients treated with Somatuline Depot may experience hypoglycemia or hyperglycemia. Blood glucose levels should be monitored when lanreotide treatment is initiated, or when the dose is altered, and antidiabetic treatment should be adjusted accordingly.
Thyroid function Abnormalities
- Slight decreases in thyroid function have been seen during treatment with lanreotide in acromegalic patients, though clinical hypothyroidism is rare (<1%). Thyroid function tests are recommended where clinically indicated.
Cardiovascular Abnormalities
- The most common overall cardiac adverse reactions observed in three pooled Somatuline Depot Cardiac Studies in patients with acromegaly were sinus bradycardia (12/217, 5.5%), bradycardia (6/217, 2.8%) and hypertension (12/217, 5.6%).
- In patients without underlying cardiac disease, lanreotide may lead to a decrease in heart rate without necessarily reaching the threshold of bradycardia. In patients suffering from cardiac disorders prior to lanreotide treatment, sinus bradycardia may occur. Care should be taken when initiating treatment with lanreotide in patients with bradycardia.
Drug Interactions
- The pharmacological gastrointestinal effects of Somatuline Depot may reduce the intestinal absorption of concomitant drugs.
- Lanreotide may decrease the relative bioavailability of cyclosporine. Concomitant administration of Somatuline Depot and cyclosporine may necessitate the adjustment of cyclosporine dose to maintain therapeutic levels.
Monitoring: Laboratory Tests
- Serum GH and IGF-1 levels are useful markers of the disease and the effectiveness of treatment
Adverse Reactions
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Clinical Studies Experience
- The data described below reflect exposure to Somatuline Depot in 416 acromegalic patients in seven studies. One study was a fixed-dose pharmacokinetic study. The other six studies were open-label or extension studies, one had a placebo controlled run-in period and another had an active control. The population was mainly Caucasian (329/353, 93%) with a median age of 53.0 years of age (range 19-84 years). Fifty-four subjects (13%) were age 66-74 and eighteen subjects (4.3%) were ≥ 75 years of age. Patients were evenly matched for gender (205 males and 211 females). The median average monthly dose was 91.2 mg (e.g., 90 mg injected via the deep subcutaneous route every 4 weeks) over 385 days with a median cumulative dose of 1290 mg. Of the patients reporting acromegaly severity at baseline (N=265), serum GH levels were < 10 ng/mL for 69% (183/265) of the patients and ≥ 10 ng/mL for 31% (82/265) of the patients.
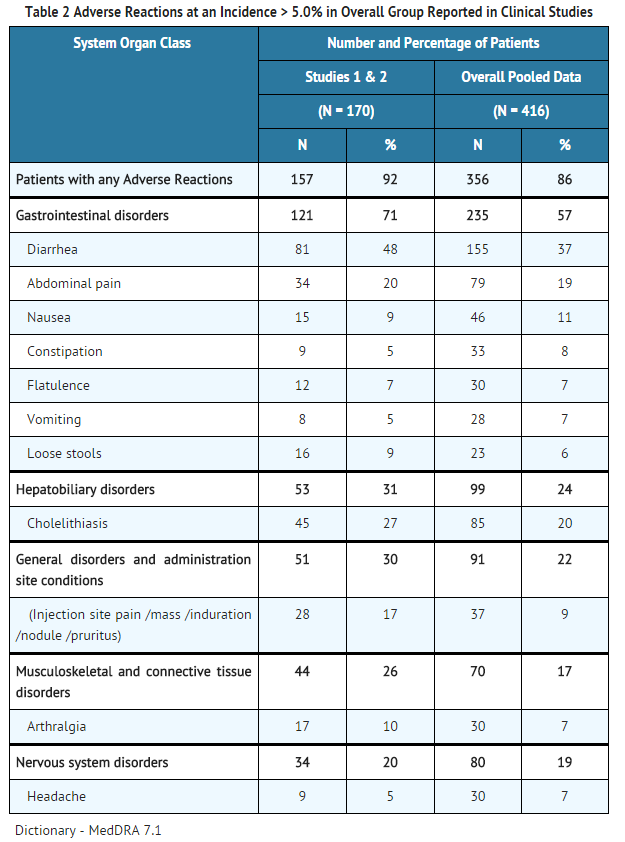
- The most commonly reported adverse reactions reported by > 5% of patients who received Somatuline Depot (N=416) in the overall pooled safety studies in acromegaly patients were gastrointestinal disorders (diarrhea, abdominal pain, nausea, constipation, flatulence, vomiting, loose stools), cholelithiasis and injection site reactions.
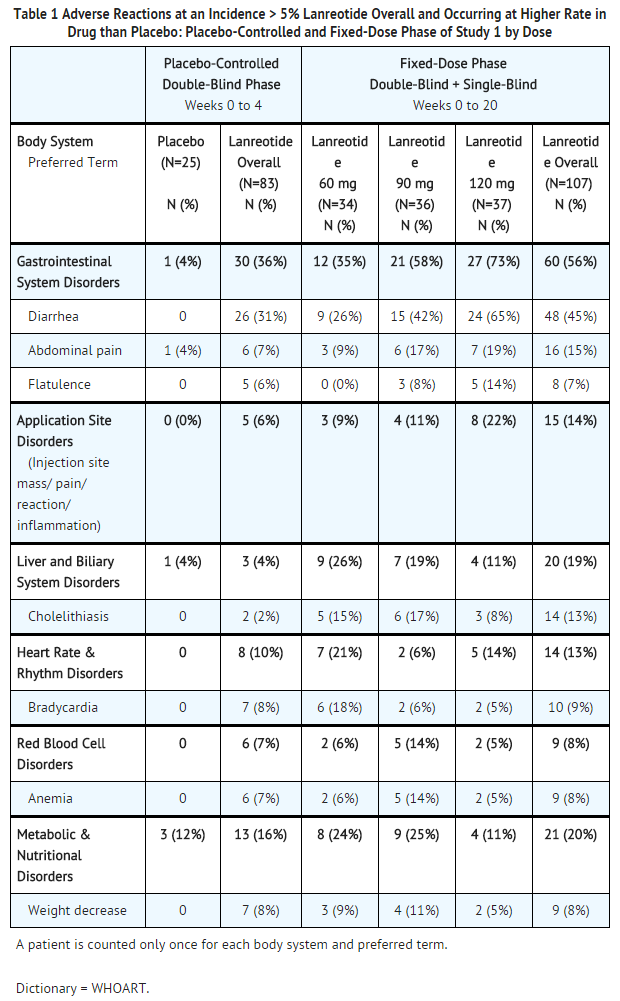
- TABLES 1 and 2 present adverse reaction data from clinical studies with Somatuline Depot in acromegalic patients. The tables include data from a single clinical study and pooled data from seven clinical studies.
Adverse Reactions in Parallel Fixed-Dose Phase of Study 1
- The incidence of treatment-emergent adverse reactions for Somatuline Depot 60 mg, 90 mg, and 120 mg by dose as reported during the first 4 months (fixed-dose phase) of Study 1 , are provided in TABLE 1.
- In Study 1, the adverse reactions of diarrhea, abdominal pain and flatulence increased in incidence with increasing dose of Somatuline Depot.
Adverse Reactions in Long-Term Clinical Trials
- TABLE 2 provides the most common adverse reactions that occurred in 416 acromegalic patients treated with Somatuline Depot in seven studies. The analysis of safety compares adverse reaction rates of patients at baseline from the two efficacy studies, to the overall pooled data from seven studies. Patients with elevated GH and IGF-1 levels were either naive to somatostatin analog therapy or had undergone a 3-month washout
- In addition to the adverse reactions listed in TABLE 2, the following reactions were also seen:
- Sinus bradycardia occurred in 7% (12) of patients in the pooled Study 1 and 2 and in 3% (13) of patients in the overall pooled studies.
- Hypertension occurred in 7% (11) of patients in the pooled Study 1 and 2 and in 5% (20) of patients in the overall pooled studies.
- Anemia occurred in 7% (12) of patients in the pooled Study 1 and 2 and in 3% (14) of patients in the overall pooled studies.
Gastrointestinal Adverse Reactions
- In the pooled clinical studies of Somatuline Depot therapy, a variety of gastrointestinal reactions occurred, the majority of which were mild to moderate in severity. One percent of acromegalic patients treated with Somatuline Depot in the pooled clinical studies discontinued treatment because of gastrointestinal reactions.
Gallbladder Adverse Reactions
- In clinical studies involving 416 acromegalic patients treated with Somatuline Depot, cholelithiasis and gallbladder sludge were reported in 20% of the patients. Among 167 acromegalic patients treated with Somatuline Depot who underwent routine evaluation with gallbladder ultrasound, 17.4% had gallstones at baseline. New cholelithiasis was reported in 12.0% of patients. Cholelithiasis may be related to dose or duration of exposure.
Injection Site Reactions
- In the pooled clinical studies, injection site pain (4.1%) and injection site mass (1.7%) were the most frequently reported local adverse drug reactions that occurred with the administration of Somatuline Depot. In a specific analysis 20 of 413 patients (4.8%) presented indurations at the injection site. Injection site adverse reactions were more commonly reported soon after the start of treatment and were less commonly reported as treatment continued. Such adverse reactions were usually mild or moderate but did lead to withdrawal from clinical studies in two subjects.
Glucose Metabolism Adverse Reactions
- In the clinical studies in acromegalic patients treated with Somatuline Depot, adverse reactions of dysglycemia (hypoglycemia, hyperglycemia, diabetes) were reported by 14% (47/332) of patients and were considered related to study drug in 7% (24/332) of patients.
Cardiac Adverse Reactions
- In the pooled clinical studies, sinus bradycardia (3.1%) was the most frequently observed heart rate and rhythm disorder. All other cardiac adverse drug reactions were observed in < 1% of patients. The relationship of these events to Somatuline Depot could not be established because many of these patients had underlying cardiac disease.
- A comparative echocardiography study of lanreotide and another somatostatin analog demonstrated no difference in the development of new or worsening valvular regurgitation between the two treatments over one year. The occurrence of clinically significant mitral regurgitation (i.e., moderate or severe in intensity) or of clinically significant aortic regurgitation (i.e., at least mild in intensity) was low in both groups of patients throughout the study.
Other Adverse Reactions
- For the most commonly occurring adverse reactions in the pooled analysis, diarrhea, abdominal pain and cholelithiasis, there was no apparent trend for increasing incidence with age. GI disorders and renal and urinary disorders were more common in patients with documented hepatic impairment; however, the incidence of cholelithiasis was similar between groups.
- Laboratory investigations of acromegalic patients treated with Somatuline Depot in clinical studies show that the percentage of patients with putative antibodies at any time point after treatment is low (<1% to 4% of patients in specific studies whose antibodies were tested). The antibodies did not appear to affect the efficacy or safety of Somatuline Depot.
Postmarketing Experience
- As adverse reactions experienced post approval use are reported voluntarily from a population of uncertain size it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- The profile of reported adverse reactions for Somatuline Depot was consistent with that observed for treatment-related adverse reactions in the clinical studies. Those reported most frequently being gastrointestinal disorders (abdominal pain and diarrhea) and general disorders and administration site conditions (injection site reactions).
Drug Interactions
Insulin and Oral Hypoglycemic Drugs
- Lanreotide, like somatostatin and other somatostatin analogs, inhibits the secretion of insulin and glucagon. Therefore, blood glucose levels should be monitored when lanreotide treatment is initiated or when the dose is altered and antidiabetic treatment should be adjusted accordingly.
Cyclosporine
- Concomitant administration of cyclosporine with lanreotide may decrease the relative bioavailability of cyclosporine and, therefore, may necessitate adjustment of cyclosporine dose to maintain therapeutic levels.
Other Concomitant Drug Therapy
- The pharmacological gastrointestinal effects of Somatuline Depot may reduce the intestinal absorption of concomitant drugs. Limited published data indicate that concomitant administration of a somatostatin analog and bromocriptine may increase the availability of bromocriptine.
- Concomitant administration of bradycardia inducing drugs (e.g. beta-blockers) may have an additive effect on the reduction of heart rate associated with lanreotide. Dose adjustments of concomitant medication may be necessary.
- Vitamin K absorption was not affected when concomitantly administered with lanreotide.
Drug Metabolism Interactions
- The limited published data available indicate that somatostatin analogs may decrease the metabolic clearance of compounds known to be metabolized by cytochrome P450 enzymes, which may be due to the suppression of growth hormone. Since it cannot be excluded that lanreotide may have this effect, other drugs mainly metabolized by CYP3A4 and which have a low therapeutic index (e.g. quinidine, terfenadine) should therefore be used with caution. Drugs metabolized by the liver may be metabolized more slowly during lanreotide treatment and dose reductions of the concomitantly administered medications should be considered.
Use in Specific Populations
Pregnancy
- Lanreotide has been shown to have an embryocidal effect in rats and rabbits. There are no adequate and well controlled studies in pregnant women. Somatuline Depot should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
- Reproductive studies in pregnant rats given 30 mg/kg by subcutaneous injection every 2 weeks (5-times the human dose based on body surface area comparisons) resulted in decreased embryo/fetal survival. Studies in pregnant rabbits given subcutaneous injections of 0.45 mg/kg/day, 2-times the human therapeutic exposures at the maximum recommended dose of 120 mg based on comparisons of relative body surface area shows decreased fetal survival and increased fetal skeletal/soft tissue abnormalities.
- Australian Drug Evaluation Committee (ADEC) Pregnancy Category
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Lanreotide in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Lanreotide during labor and delivery.
Nursing Mothers
It is not known whether lanreotide is excreted in human milk. Many drugs are excreted in human milk. As a result of serious adverse reactions in animals and potential in nursing infants from Somatuline, a decision should be made whether to discontinue nursing or discontinue the drug taking into account the importance of the drug to the mother.
Pediatric Use
- Safety and effectiveness in pediatric patients have not been established.
Geriatic Use
- No overall differences in safety or effectiveness were observed between elderly patients compared with younger patients, and the other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. It is not necessary to alter the starting dose in elderly patients as expected lanreotide serum concentrations in the elderly are well within the range of serum concentrations safely tolerated in healthy young subjects. Similarly, it is not necessary to alter the titration or maintenance doses of Somatuline Depot as dose selection is based on therapeutic response
Gender
There is no FDA guidance on the use of Lanreotide with respect to specific gender populations.
Race
There is no FDA guidance on the use of Lanreotide with respect to specific racial populations.
Renal Impairment
- Lanreotide has not been studied in patients with mild, moderate and severe renal failure. It is recommended that patients with moderate and severe renal impairment receive a starting dose of lanreotide of 60 mg
Hepatic Impairment
- It is recommended that patients with moderate and severe hepatic impairment receive a starting dose of lanreotide of 60 mg
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Lanreotide in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Lanreotide in patients who are immunocompromised.
Administration and Monitoring
Administration
- Subcutaneous Injection
Monitoring
- Lanreotide may reduce gallbladder motility and lead to gallstone formation therefore, patients may need to be monitored periodically
- Blood glucose levels should be monitored when lanreotide treatment is initiated, or when the dose is altered, and antidiabetic treatment should be adjusted accordingly
- Serum GH and IGF-1 levels are useful markers of the disease and the effectiveness of treatment
IV Compatibility
There is limited information regarding IV Compatibility of Lanreotide in the drug label.
Overdosage
- If overdose occurs, symptomatic management is indicated.
- There are no confirmed postmarketing cases of overdose with lanreotide that were serious or led to an adverse reaction.
- Up-to-date information about the treatment of overdose can often be obtained from the National Poison Control Center at phone number 1-800-222-1222.
Pharmacology
Mechanism of Action
- Lanreotide, the active component of Somatuline Depot is an octapeptide analog of natural somatostatin. The mechanism of action of lanreotide is believed to be similar to that of natural somatostatin.
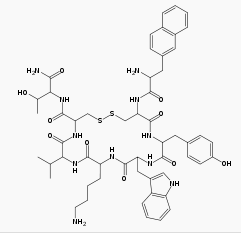
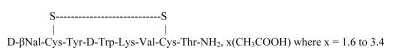
Structure
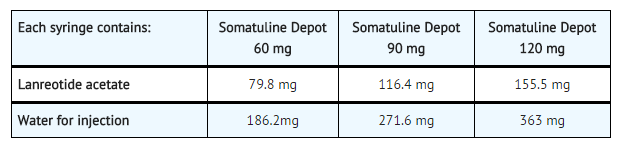
- Lanreotide acetate is a synthetic cyclical octapeptide analog of the natural hormone, somatostatin. Lanreotide acetate is chemically known as [cyclo S-S]-3-(2-naphthyl)-D-alanyl-L-cysteinyl-L-tyrosyl-D-tryptophyl-L-lysyl-L-valyl-L-cysteinyl-L-threoninamide, acetate salt. Its molecular weight is 1096.34 (base) and its amino acid sequence is:
- Somatuline Depot (lanreotide) Injection 60, 90 and 120 mg is a prolonged-release formulation for deep subcutaneous injection containing the drug substance lanreotide acetate, a synthetic octapeptide with a biological activity similar to naturally occurring somatostatin, and water for injection.
- Somatuline Depot is available as sterile, ready-to-use, pre-filled syringes containing lanreotide supersaturated bulk solution of 24.6% w/w lanreotide base.
Pharmacodynamics
- Lanreotide has a high affinity for human somatostatin receptors (SSTR) 2 and 5 and a reduced binding affinity for human SSTR1, 3, and 4. Activity at human SSTR 2 and 5 is the primary mechanism believed responsible for GH inhibition. Like somatostatin, lanreotide is an inhibitor of various endocrine, neuroendocrine, exocrine and paracrine functions.
- The primary pharmacodynamic effect of lanreotide is a reduction of GH and/or IGF-1 levels enabling normalization of levels in acromegalic patients [see Clinical Studies (14)]. In acromegalic patients, lanreotide reduces GH levels in a dose-dependent way. After a single injection of Somatuline Depot, plasma GH levels fall rapidly and are maintained for at least 28 days.
- Lanreotide inhibits the basal secretion of motilin, gastric inhibitory peptide and pancreatic polypeptide, but has no significant effect on the secretion of secretin. Lanreotide inhibits post-prandial secretion of pancreatic polypeptide, gastrin and cholecystokinin (CCK). In healthy subjects, lanreotide produces a reduction and a delay in post-prandial insulin secretion, resulting in transient, mild glucose intolerance.
- Lanreotide inhibits meal-stimulated pancreatic secretions, and reduces duodenal bicarbonate and amylase concentrations, and produces a transient reduction in gastric acidity.
- Lanreotide has been shown to inhibit gallbladder contractility and bile secretion in healthy subjects.
- In healthy subjects, lanreotide inhibits meal-induced increases in superior mesenteric artery and portal venous blood flow, but has no effect on basal or meal-stimulated renal blood flow. Lanreotide has no effect on renal plasma flow or renal vascular resistance. However, a transient decrease in glomerular filtration rate (GFR) and filtration fraction has been observed after a single injection of lanreotide.
- In healthy subjects, non-significant reductions in glucagon levels were seen after lanreotide administration. In diabetic non-acromegalic subjects receiving a continuous infusion (21 day) of lanreotide, serum glucose concentrations were temporarily decreased by 20-30% after the start and end of the infusion. Serum glucose concentrations returned to normal levels within 24 hours. A significant decrease in insulin concentrations was recorded between baseline and Day 1 only.
- Lanreotide inhibits the nocturnal increase in thyroid-stimulating hormone (TSH) seen in healthy subjects. Lanreotide reduces prolactin levels in acromegalic patients treated on a long-term basis.
Pharmacokinetics
- Somatuline Depot is thought to form a drug depot at the injection site due to the interaction of the formulation with physiological fluids. The most likely mechanism of drug release is a passive diffusion of the precipitated drug from the depot towards the surrounding tissues, followed by the absorption to the blood stream.
- After a single deep, subcutaneous administration, the mean absolute bioavailability of Somatuline Depot in healthy subjects was 73.4, 69.0 and 78.4%, for the 60, 90 and 120 mg doses, respectively. Mean Cmax values ranged from 4.3 to 8.4 ng/mL during the first day. Single-dose linearity was demonstrated with respect to AUC and Cmax, and showed high inter-subject variability. Somatuline Depot showed sustained release of lanreotide with a half-life of 23 to 30 days. Mean serum concentrations were > 1 ng/mL throughout 28 days at 90 mg and 120 mg and > 0.9 ng/mL with 60 mg.
- In a repeat-dose administration pharmacokinetics (PK) study in acromegalic patients, rapid initial release was seen giving peak levels during the first day after administration. At doses of Somatuline Depot between 60 and 120 mg linear pharmacokinetics were observed in acromegalic patients. At steady state mean Cmax values were 3.8 ± 0.5, 5.7 ± 1.7 and 7.7 ± 2.5 ng/mL increasing linearly with dose. The mean accumulation ratio index was 2.7 which is in line with the range of values for the half life of Somatuline Depot. The steady-state trough serum lanreotide concentrations in patients receiving Somatuline Depot every 28 days were 1.8 ± 0.3; 2.5 ± 0.9 and 3.8 ± 1.0 ng/mL at 60, 90 and 120 mg doses respectively. A limited initial burst effect and a low peak to trough fluctuation (81% to 108%) of the serum concentration at the plateau was observed.
- For the same doses, similar values were obtained in clinical studies after at least four administrations (2.3 ± 0.9, 3.2 ± 1.1 and 4.0 ± 1.4 ng/mL, respectively).
- Somatuline Depot has not been studied in special populations. For completeness, information on studies with an immediate-release formulation (IRF) of lanreotide administered intravenously is provided. A lthough some changes in elimination or distribution have been observed after IRF administration, no changes in the apparent half-life are expected with Somatuline Depot as the terminal phase is controlled by the release of lanreotide from the formulation.
- Subjects with end-stage renal disease requiring dialysis showed an approximate 2-fold decrease in total serum clearance of lanreotide, with a consequent 2-fold increase in half-life and AUC.
- Studies in healthy elderly subjects showed an 85% increase in half-life and a 65% increase in mean residence time (MRT) of lanreotide compared to those seen in healthy young subjects; however, there was no change in either AUC or Cmax of lanreotide in elderly as compared to healthy young subjects.
- In moderately to severely hepatically-impaired subjects, a 30% reduction in clearance of lanreotide was observed.
- Patients with moderate to severe renal impairment or moderate to severe hepatic impairment should begin treatment with Somatuline Depot 60 mg.
- In studies evaluating excretion, <5% of lanreotide was excreted in urine and less than 0.5% was recovered unchanged in feces, indicative of some biliary excretion.
Nonclinical Toxicology
Carcinogenicity, Mutagenicity, Impairment of Fertility
- Standard lifetime carcinogenicity bioassays were conducted in mice and rats. Mice were given daily subcutaneous doses of lanreotide acetate at 0.5, 1.5, 5, 10 and 30 mg/kg for 104 weeks. Cutaneous and subcutaneous tumors of fibrous connective tissues at the injection sites were observed at the high dose of 30 mg/kg/day. Fibrosarcomas in both genders and malignant fibrous histiocytomas were observed in males at 30mg/kg/day resulting in exposures 3-times higher than the clinical therapeutic exposure at the maximum therapeutic dose of 120 mg given by monthly subcutaneous injection based on the AUC values. Rats were given daily subcutaneous doses of lanreotide acetate at 0.1, 0.2, and 0.5 mg/kg for 104 weeks. Increased cutaneous and subcutaneous tumors of fibrous connective tissues at the injection sites were observed at the dose of 0.5mg/kg/day resulting in exposures less than the clinical therapeutic exposure at 120 mg given by monthly subcutaneous injection. The increased incidence of injection site tumors in rodents is likely related to the increased dosing frequency (daily) in animals compared to monthly dosing in humans and therefore may not be clinically relevant.
- Lanreotide was not genotoxic in tests for gene mutations in a bacterial mutagenicity (Ames) assay, or mouse lymphoma cell assay with or without metabolic activation. Lanreotide was not genotoxic in tests for the detection of chromosomal aberrations in a human lymphocyte and in vivo mouse micronucleus assay.
- Subcutaneous dosing (30mg/kg/2 wks) before mating and continuing into gestation in rats at doses 5 times the human clinical exposure (120 mg every 4 weeks) based on mg/m2 had reduced fertility. Gestation length was statistically significantly increased suggesting some delay in parturition at 3 times human exposure. The reduction in fertility in non-acromegalic animals is likely related to the pharmacologic activity (decreased growth hormone secretion) of lanreotide acetate.
Clinical Studies
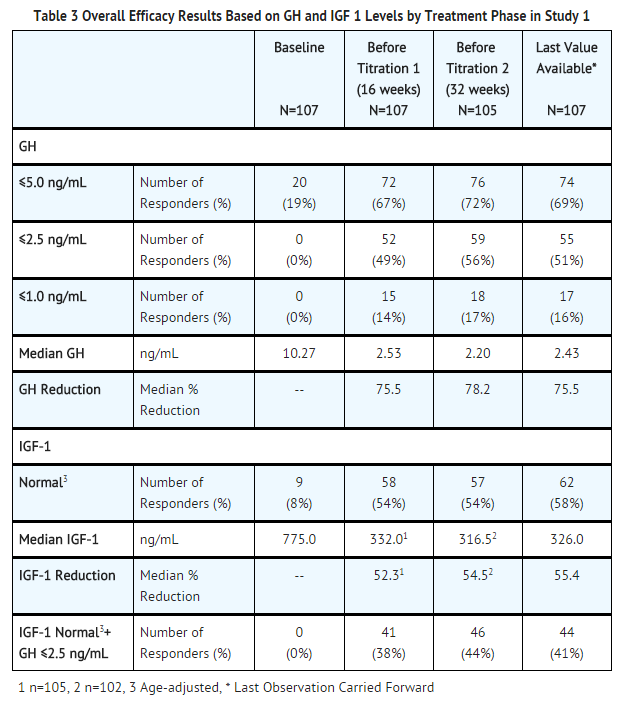
- The effect of Somatuline Depot on reducing GH and IGF-levels and control of symptoms in patients with acromegaly was studied in two long-term, multiple-dose, randomized multicenter studies.
Study 1
- This one-year study included a 4-week double-blind, placebo-controlled phase, a 16-week single-blind, fixed-dose phase, and a 32-week open-label dose-titration phase. Patients with active acromegaly based on biochemical tests and medical history entered a 12-week washout period if there was previous treatment with a somatostatin analog or a dopaminergic agonist.
- Upon entry, patients were randomly allocated to receive a single deep subcutaneous injection of Somatuline Depot 60, 90 or 120 mg or placebo. Four weeks later, patients entered a fixed-dose phase where they received 4 injections of Somatuline Depot followed by a dose-titration phase of 8 injections for a total of 13 injections over 52 weeks (including the placebo phase). Injections were given at 4-week intervals. During the dose-titration phase of the study, the dose was titrated twice (every fourth injection), as needed, according to individual GH and IGF-1 levels.
- A total of 108 patients (51 males, 57 females) were enrolled in the initial placebo-controlled phase of the study. Half (54/108) of the patients had never been treated with a somatostatin analog or dopamine agonist, or had stopped treatment for at least 3 months prior to their participation in the study and were required to have a mean GH level > 5 ng/mL at their first visit. The other half of the patients had received prior treatment with a somatostatin analog or a dopamine agonist before study entry and at study entry were to have a mean GH concentration >3 ng/mL and at least a 100% increase in mean GH concentration after washout of medication.
- One hundred and seven (107) patients completed the placebo-controlled phase, 105 patients completed the fixed-dose phase and 99 patients completed the dose-titration phase. Patients not completing withdrew due to adverse events (5) or lack of efficacy (4).
- In the double-blind phase of study 1, a total of 52 (63%) of the 83 lanreotide-treated patients had a > 50% decrease in mean GH from baseline to Week 4 including 52%, 44% and 90% of patients in the 60, 90 and 120 mg groups, respectively, compared to placebo (0%, 0/25). In the fixed-dose phase at Week 16, 72% of all 107 lanreotide-treated patients had a decrease from baseline in mean GH of > 50% including 68% (23/34), 64% (23/36) and 84% (31/37) of patients in the 60, 90 and 120 mg lanreotide treatment groups, respectively. Efficacy achieved in the first 16 weeks was maintained for the duration of the study (see TABLE 3).
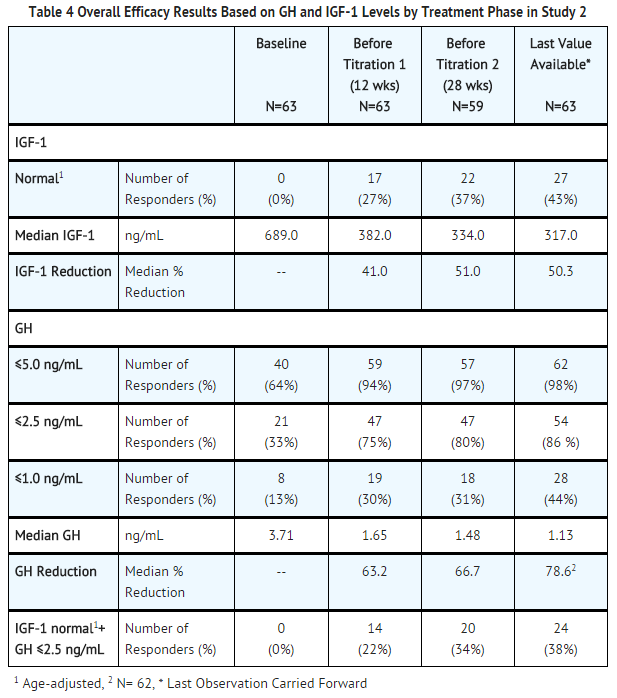
Study 2
- This was a 48-week, open-label, uncontrolled multicenter study which enrolled patients who had an IGF-1 concentration ≥ 1.3 times the upper limit of the age-adjusted normal range. Patients receiving treatment with a somatostatin analog (other than Somatuline Depot) or a dopaminergic agonist had to attain this IGF-1 concentration after a washout period of up to 3 months.
- Patients were initially enrolled in a 4-month fixed-dose phase where they received four deep subcutaneous injections of Somatuline Depot, 90 mg, at 4-week intervals. Patients then entered a dose-titration phase where the dose of Somatuline Depot was adjusted based on GH and IGF-1 levels at the beginning of the dose-titration phase and, if necessary, again after another 4 injections. Patients titrated up to the maximum dose (120 mg) were not allowed to titrate down again.
- A total of 63 patients (38 males, 25 females) entered the fixed-dose phase of the trial and 57 patients completed 48-weeks of treatment. Six patients withdrew due to adverse reactions (3), other reasons (2), or lack of efficacy (1).
- After 48 weeks of treatment with Somatuline Depot at 4-week intervals, 43% (27/63) of the acromegalic patients in this study achieved normal age-adjusted IGF-1 concentrations. Mean IGF-1 concentrations after treatment completion were 1.3 ± 0.7 times the upper limit of normal compared to 2.5 ± 1.1 times the upper limit of normal at baseline.
- The reduction in IGF-1 concentrations over time correlated with a corresponding marked decrease in mean GH concentrations. The proportion of patients with mean GH concentrations < 2.5 ng/mL increased significantly from 35% to 77% after the fixed-dose phase and 85% at the end of the study. At the end of treatment, 24/63 (38%) of patients had both normal IGF-1 concentrations and a GH concentration of ≤ 2.5 ng/mL (see TABLE 4) and 17/63 patients (27%) had both normal IGF-1 concentrations and a GH concentration of <1 ng/mL.
- Examination of age and gender subgroups did not identify differences in response to Somatuline Depot among these subgroups. The limited number of patients in the different racial subgroups did not raise any concerns regarding efficacy of Somatuline Depot in these subgroups.
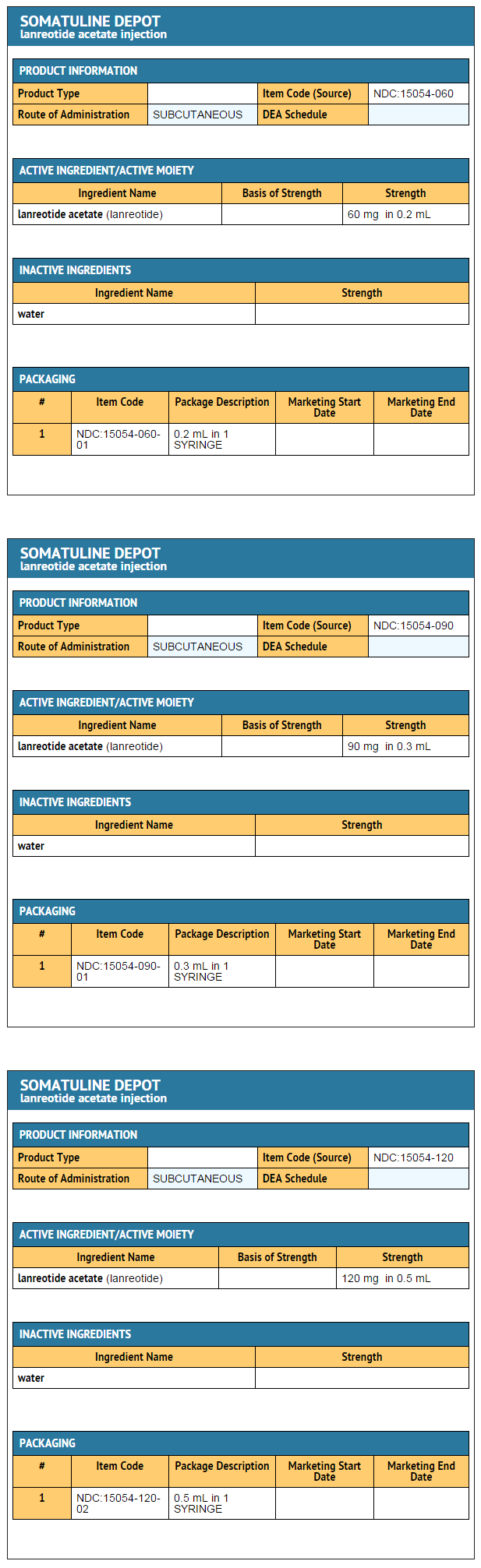
How Supplied
- Somatuline Depot is supplied in strengths of 60 mg, 90 mg and 120 mg in a single, sterile, pre-filled, ready-to-use, polypropylene syringe fitted with a 20 mm needle covered by a dry natural rubber sheath. Each pre-filled syringe is sealed in a laminated pouch and packed in a carton.
- NDC 15054-060-01 60-mg, sterile, pre-filled syringe
- NDC 15054-090-01 90-mg, sterile, pre-filled syringe
- NDC 15054-120-02 120-mg, sterile,pre-filled syringe
Storage
- Somatuline Depot must be stored in a refrigerator at 2°C to 8°C (36°F to 46°F) and protected from light in its original package. Thirty (30) minutes prior to injection, remove sealed pouch of Somatuline Depot from refrigerator and allow it to come to room temperature. Keep pouch sealed until injection.
- Each syringe is intended for single use. Do not use beyond the expiration date on the packaging.
Images
Drug Images
{{#ask: Page Name::Lanreotide |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
Ingredientd and Appearance
{{#ask: Label Page::Lanreotide |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- The physician should provide a copy of the FDA-Approved Patient Labeling and review the contents with the patient. Patients should be advised to inform their doctor or pharmacist if they develop any unusual symptoms, or if any known symptom persists or worsens.
- Patients should be advised that response to Somatuline Depot should be monitored by periodic measurements of GH and IGF-1 levels, with a goal of decreasing these levels to the normal range.
SUPPLEMENTAL PATIENT MATERIAL
Patient Labeling
Somatuline® Depot (So-mah-tu-leen Dee-Poh )
- (lanreotide) Injection
- Read the Patient Information that comes with Somatuline® Depot before you receive the first injection and before each monthly injection. There may be new information. This leaflet does not take the place of talking with your doctor about your medical condition or your treatment.
What is Somatuline® Depot?
- Somatuline® Depot is an injectable medicine used for the long-term treatment of patients with acromegaly:
- when surgery or radiotherapy have not worked well enough
- who are not able to have surgery or radiotherapy
- Somatuline® Depot contains the medicine lanreotide, which is similar to the hormone somatostatin (which is made in the body). Somatuline® Depot, like somatostatin, lowers the levels of certain hormones in the body such as growth hormone (GH) and insulin-like growth factor-1 (IGF-1). Lowering these hormone levels can help treat patients with acromegaly.
- Somatuline Depot has not been studied in children.
What should I tell my doctor before receiving Somatuline® Depot?
- Tell your doctor about all of your medical conditions, including if you:
- have diabetes.
- have liver or kidney problems.
- have ever had heart problems.
- are allergic to latex or natural dry rubber. The pre-filled syringe needle cover contains rubber.
- are pregnant or can become pregnant. It is not known if Somatuline Depot could harm your unborn baby.
- are breast-feeding or planning to breast-feed. It is not known if Somatuline® Depot passes into your breast milk. Talk to your doctor about the best way to feed your baby if you receive Somatuline® Depot.
- Tell your doctor about all the medicines you take, including prescription and non-prescription medicines, vitamins and herbal supplements. Somatuline® Depot and other medicines may affect each other causing side effects. Somatuline® Depot may affect the way other medicines work, and other medicines may affect how Somatuline® Depot works. The dose of Somatuline® Depot or your other medicines may need to be adjusted.
- Especially tell your doctor if you take:
- insulin or other diabetes medicines
- medicines that lower your heart rate such as beta blockers
- Cyclosporine (Gengraf, Neoral, Sandimmune)
- Bromocriptine (Parlodel)
- Know the medicines you take. Keep a list of your medicines and show it to your doctor..
How will I receive Somatuline® Depot?
- You will receive a Somatuline® Depot injection every 4 weeks as directed by your doctor. Your doctor will tell you how long you need to receive Somatuline Depot.
- Somatuline® Depot is injected deep under the skin of the upper outer area of your buttock.
- The injection site should change (alternate) between your right and left side each time you receive an injection of Somatuline® Depot.
- After 3 months, your doctor should check your levels of growth hormone (GH) and insulin-like growth factor-1 (IGF-1), talk to you about your symptoms, and adjust your dose of Somatuline® Depot as needed.
- If you miss an injection, talk with your doctor as soon as possible to advise on another injection.
What are the possible side effects of Somatuline® Depot?
- Side effects include:
- Stomach and Intestinal problems. Diarrhea, stomach (abdominal) pain, nausea, gas, constipation and loose stools can occur. These side effects tend to diminish with continued treatment.
- Gallbladder problems. Gallstones can develop in the gallbladder. Tell your doctor if you get severe pain in the right upper area of your stomach (abdomen), along with nausea and vomiting. The pain may last for several hours.
- Skin reactions. Pain, itching or a lump may occur at the injection site.
- Heart problems including a low heart rate, high blood pressure, and new or worse heart valve problems.
- Change in blood sugar levels. Somatuline® Depot can cause low blood sugar (hypoglycemia) or high blood sugar (hyperglycemia) levels, especially when you first start receiving the injections or if the dose is changed. If you have diabetes, carefully follow your doctor's instructions for monitoring your blood sugar levels. Your diabetes medicines may need to be changed in order to control your blood sugar while you are receiving Somatuline® Depot.
- Other side effects include: headache, joint pain, anemia (decreased red blood cells), tiredness, and weight loss.
- Tell your doctor if you have any side effect that bothers you or that does not go away. These are not all the possible side effects of Somatuline® Depot. Ask your doctor for more information.
General Information about Somatuline® Depot
- Medicines are sometimes prescribed for conditions other than those listed in the patient leaflet. This Patient Information leaflet summarizes the most important information about Somatuline® Depot. If you would like more information about Somatuline® Depot talk with your doctor. You can ask your doctor or healthcare provider for information on Somatuline® Depot that is written for health professionals.
- For more information call TERCICA at 1-866-837-2422 or visit the website at www.somatulinedepot.com.
Precautions with Alcohol
- Alcohol-Lanreotide interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- Somatuline Depot®[2]
Look-Alike Drug Names
There is limited information regarding Lanreotide Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ Schiedermaier P, Harrison P, Arthur M, Grandt D, Sutton R, Drewe J; et al. (2002). "Effect of the somatostatin analogue lanreotide on meal-stimulated portal blood flow in patients with liver cirrhosis". Digestion. 65 (1): 56–60. doi:51932 Check
|doi=value (help). PMID 11961344. - ↑ "Lanreotide Acetate".