Idiopathic interstitial pneumonia natural history, complications and prognosis
|
Idiopathic Interstitial Pneumonia Microchapters |
|
Differentiating Idiopathic interstitial pneumonia from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Idiopathic interstitial pneumonia natural history, complications and prognosis On the Web |
|
American Roentgen Ray Society Images of Idiopathic interstitial pneumonia natural history, complications and prognosis |
|
FDA onIdiopathic interstitial pneumonia natural history, complications and prognosis |
|
CDC on Idiopathic interstitial pneumonia natural history, complications and prognosis |
|
Idiopathic interstitial pneumonia natural history, complications and prognosisin the news |
|
on Idiopathic interstitial pneumonia natural history, complications and prognosis |
|
Directions to Hospitals Treating Idiopathic interstitial pneumonia |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Ahmed Zaghw, M.D. [2]
Overview
The heterogeneous nature of idiopathic interstitial pneumonia with its various clinical picture makes the outcomes and prognosis is different for each subtype. Acute interstitial pneumonia is of sudden onset and extremely rapid respiratory failure with deteriorating hypoxemia with over than 60% mortality in 6 month.[1] However chronic interstitial pneumonia may be nonspecific cellular which would have a long survival period over than 10 years, of better outcome than chronic nonspecific fibrosing.[2] Different quantitative parameters have been suggested and still being validated to assess to severity and predict the outcomes. Patient scoring system is simply a way to involve different clinical, radiological, histopathological and biomarkers parameters to define what will be accurately correlated with the real clinical events.
Natural History and Complications
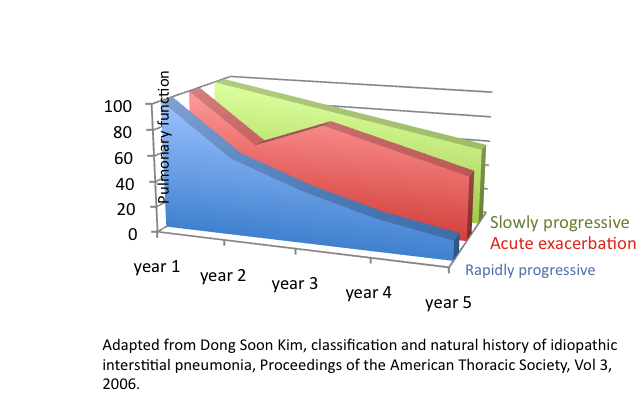
- The diagnosis of acute exacerbation of IIPs requires an evidence of respiratory deterioration and exclusion of common causes, such as infection, pulmonary embolism, heart failure, and pneumothorax.[3] Acute exacerbation of IPF has been associated with increased mortality; in fact, recent studies have suggested mortality rates ranging from 20 to 86% following an acute exacerbation of IPF.[4][5] In addition, a retrospective study showed that 50% of the mortality of IPF patients occurred in the context of an acute deterioration in pulmonary function associated with an acute exacerbation. [6].Shown below is an image depicting different pattern of changes in the pulmonary functions over years after diagnosis.
Predictors for survival
- Controversial debate among the patient age and the baseline pulmonary function, as some studies found that may have predictive significance however other studies found that inconsistent with any prognostic value.
- Histological and radiological parameters were considered over the past decade as an estimate for the patient outcome.
- Conventional radiological findings as mild ground glass attenuation predicts physiologic improvement after steroid treatment.[7] As mild ground glass opacity on CT often regresses on treatment in patients who have histological DIP, but may not decrease as readily in those with histologic UIP.[8] However some areas of ground glass opacity not only regress with treatment, but it may progress to reticular opacity or honeycombing on follow-up evaluation[9] Predominant reticular opacity or honeycombing usually progress despite treatment. The extent of lung fibrosis on CT is an important predictor of survival.[10]
- High resolution Computed Tomography (RCT) has a prognostic value as consistent HRCT findings such as symmetric bilateral reticulation, architectural distortion and lower lobes subpleural lung regions honeycombing are associated with the worst survival with median survival of 2.08, however inconsistent HRCT findings are associated with less mortality with more median survival 5.79.[11]
- Composite index increases the prognostic power as multiple parameters are more accurate than single parameter.
- Composite physiologic index (CPI) from simple spirometry and DlCO and demonstrated that CPI was linked to mortality more closely than the individual pulmonary function test values.[11]
- The CPI score is easier to generate because no radiographic scoring or exercise data are required. But still wide validation studies for CPI are required
Chronic Fibrosing IIPs
- Idiopathic Pulmonary Fibrosis
- The most common and the worst prognosis of chronic IIPs.
- survival time depends on the definition of the diagnosis ( reticular background on conventional X-ray or onset of the symptoms which usually is 2-3 years after the radiological findings)[5]
- 5-yr mortality 80%, median survival 2-3 year
- Mortality is most frequently due to respiratory failure (38.7%); other causes of death include heart failure (14.4%), bronchogenic carcinoma (10.4%), ischemic heart disease (9.5%), infection (6.5%), and pulmonary embolism (3.4%)[12]
- Nonfatal disease-associated complications include pneumothorax, corticosteroid-induced metabolic side effects and myopathy, and therapy-related immunosuppression.
- Idiopathic Nonspecific Interstitial Pneumonia
- Better outcome than IPF.
- Cellular type is more common than Fibrotic type.
- The cellular NSIP is better than fibrosing type of NSIP.
- Larger studies are needed to understand the clinical course of NSIP.
- Cellular NSIP median survival > 10 years, however fibrotic NSIP median survival is 6-8 years.
- Cellular NSIP 5-year mortality is <10%, however fibrotic NSIP 5-year mortality is >10%[2]
- Other studies showed that 10-year survival of fibrotic NSIP is 35%,[13] 5-Yr survival rate is 43%, [14] 25% deterioration of lung function despite treatment.[15]
Acute/Subacute IIPs
- Cryptogenic Organizing Pneumonia
- 5-year mortality < 5%[2]
- Respiratory Bronchiolitis-Interstitial Lung Disease
- No death reported, 5-year mortality < 5%[2]
- Desquamative Interstitial Pneumonia
- No death reported, 5-yr mortality < 5%[2]
Biomarkers
The functional lung capacity, pulmonary functions and mortality have been linked to some biomarkers. For example some studies showed that rapidly deteriorating lung function and higher mortality have been associated with high serum level of epithelial or macrophage-related proteins such as SP-A, SP-D, KL-6 (Krebs von den Lungen-6), CCL18 (chemokine ligand-18), and MMP-7 (matrix metalloproteinase-7)[16][17][18]
References
- ↑ Vourlekis, JS. (2004). "Acute interstitial pneumonia". Clin Chest Med. 25 (4): 739–47, vii. doi:10.1016/j.ccm.2004.07.001. PMID 15564019. Unknown parameter
|month=ignored (help) - ↑ 2.0 2.1 2.2 2.3 2.4 2.5 King, TE. (2005). "Clinical advances in the diagnosis and therapy of the interstitial lung diseases". Am J Respir Crit Care Med. 172 (3): 268–79. doi:10.1164/rccm.200503-483OE. PMID 15879420. Unknown parameter
|month=ignored (help) - ↑ Rice, AJ.; Wells, AU.; Bouros, D.; du Bois, RM.; Hansell, DM.; Polychronopoulos, V.; Vassilakis, D.; Kerr, JR.; Evans, TW. (2003). "Terminal diffuse alveolar damage in relation to interstitial pneumonias. An autopsy study". Am J Clin Pathol. 119 (5): 709–14. doi:10.1309/UVAR-MDY8-FE9F-JDKU. PMID 12760290. Unknown parameter
|month=ignored (help) - ↑ Azuma, A.; Nukiwa, T.; Tsuboi, E.; Suga, M.; Abe, S.; Nakata, K.; Taguchi, Y.; Nagai, S.; Itoh, H. (2005). "Double-blind, placebo-controlled trial of pirfenidone in patients with idiopathic pulmonary fibrosis". Am J Respir Crit Care Med. 171 (9): 1040–7. doi:10.1164/rccm.200404-571OC. PMID 15665326. Unknown parameter
|month=ignored (help) - ↑ 5.0 5.1 5.2 Kim, DS.; Park, JH.; Park, BK.; Lee, JS.; Nicholson, AG.; Colby, T. (2006). "Acute exacerbation of idiopathic pulmonary fibrosis: frequency and clinical features". Eur Respir J. 27 (1): 143–50. doi:10.1183/09031936.06.00114004. PMID 16387947. Unknown parameter
|month=ignored (help) - ↑ Martinez, FJ.; Safrin, S.; Weycker, D.; Starko, KM.; Bradford, WZ.; King, TE.; Flaherty, KR.; Schwartz, DA.; Noble, PW. (2005). "The clinical course of patients with idiopathic pulmonary fibrosis". Ann Intern Med. 142 (12 Pt 1): 963–7. PMID 15968010. Unknown parameter
|month=ignored (help) - ↑ Wells, AU.; Rubens, MB.; du Bois, RM.; Hansell, DM. (1993). "Serial CT in fibrosing alveolitis: prognostic significance of the initial pattern". AJR Am J Roentgenol. 161 (6): 1159–65. doi:10.2214/ajr.161.6.8249719. PMID 8249719. Unknown parameter
|month=ignored (help) - ↑ Hartman, TE.; Primack, SL.; Kang, EY.; Swensen, SJ.; Hansell, DM.; McGuinness, G.; Müller, NL. (1996). "Disease progression in usual interstitial pneumonia compared with desquamative interstitial pneumonia. Assessment with serial CT". Chest. 110 (2): 378–82. PMID 8697837. Unknown parameter
|month=ignored (help) - ↑ Terriff, BA.; Kwan, SY.; Chan-Yeung, MM.; Müller, NL. (1992). "Fibrosing alveolitis: chest radiography and CT as predictors of clinical and functional impairment at follow-up in 26 patients". Radiology. 184 (2): 445–9. doi:10.1148/radiology.184.2.1620845. PMID 1620845. Unknown parameter
|month=ignored (help) - ↑ Gay, SE.; Kazerooni, EA.; Toews, GB.; Lynch, JP.; Gross, BH.; Cascade, PN.; Spizarny, DL.; Flint, A.; Schork, MA. (1998). "Idiopathic pulmonary fibrosis: predicting response to therapy and survival". Am J Respir Crit Care Med. 157 (4 Pt 1): 1063–72. doi:10.1164/ajrccm.157.4.9703022. PMID 9563720. Unknown parameter
|month=ignored (help) - ↑ 11.0 11.1 Flaherty, KR.; Thwaite, EL.; Kazerooni, EA.; Gross, BH.; Toews, GB.; Colby, TV.; Travis, WD.; Mumford, JA.; Murray, S. (2003). "Radiological versus histological diagnosis in UIP and NSIP: survival implications". Thorax. 58 (2): 143–8. PMID 12554898. Unknown parameter
|month=ignored (help) - ↑ Panos, RJ.; Mortenson, RL.; Niccoli, SA.; King, TE. (1990). "Clinical deterioration in patients with idiopathic pulmonary fibrosis: causes and assessment". Am J Med. 88 (4): 396–404. PMID 2183601. Unknown parameter
|month=ignored (help) - ↑ Travis, WD.; Matsui, K.; Moss, J.; Ferrans, VJ. (2000). "Idiopathic nonspecific interstitial pneumonia: prognostic significance of cellular and fibrosing patterns: survival comparison with usual interstitial pneumonia and desquamative interstitial pneumonia". Am J Surg Pathol. 24 (1): 19–33. PMID 10632484. Unknown parameter
|month=ignored (help) - ↑ Nicholson, AG.; Colby, TV.; du Bois, RM.; Hansell, DM.; Wells, AU. (2000). "The prognostic significance of the histologic pattern of interstitial pneumonia in patients presenting with the clinical entity of cryptogenic fibrosing alveolitis". Am J Respir Crit Care Med. 162 (6): 2213–7. doi:10.1164/ajrccm.162.6.2003049. PMID 11112140. Unknown parameter
|month=ignored (help) - ↑ Kondoh, Y.; Taniguchi, H.; Yokoi, T.; Nishiyama, O.; Ohishi, T.; Kato, T.; Suzuki, K.; Suzuki, R. (2005). "Cyclophosphamide and low-dose prednisolone in idiopathic pulmonary fibrosis and fibrosing nonspecific interstitial pneumonia". Eur Respir J. 25 (3): 528–33. doi:10.1183/09031936.05.00071004. PMID 15738299. Unknown parameter
|month=ignored (help) - ↑ Satoh, H.; Kurishima, K.; Ishikawa, H.; Ohtsuka, M. (2006). "Increased levels of KL-6 and subsequent mortality in patients with interstitial lung diseases". J Intern Med. 260 (5): 429–34. doi:10.1111/j.1365-2796.2006.01704.x. PMID 17040248. Unknown parameter
|month=ignored (help) - ↑ Prasse, A.; Probst, C.; Bargagli, E.; Zissel, G.; Toews, GB.; Flaherty, KR.; Olschewski, M.; Rottoli, P.; Müller-Quernheim, J. (2009). "Serum CC-chemokine ligand 18 concentration predicts outcome in idiopathic pulmonary fibrosis". Am J Respir Crit Care Med. 179 (8): 717–23. doi:10.1164/rccm.200808-1201OC. PMID 19179488. Unknown parameter
|month=ignored (help) - ↑ Ishii, H.; Mukae, H.; Kadota, J.; Kaida, H.; Nagata, T.; Abe, K.; Matsukura, S.; Kohno, S. (2003). "High serum concentrations of surfactant protein A in usual interstitial pneumonia compared with non-specific interstitial pneumonia". Thorax. 58 (1): 52–7. PMID 12511721. Unknown parameter
|month=ignored (help)