Galcanezumab-gnlm
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Zach Leibowitz [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Galcanezumab-gnlm is a calcitonin-gene related peptide antagonist that is FDA approved for the preventive treatment of of migraine and the treatment of episodic cluster headache. Common adverse reactions include injection site reactions.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indication
Migraine
- Galcanezumab-gnlm is indicated for the preventive treatment of migraine in adults.
Episodic Cluster Headache
- Galcanezumab-gnlm is indicated for the treatment of episodic cluster headache in adults.
Dosage
Recommended Dosing for Migraine
- 240 mg loading dose (administered as two consecutive injections of 120 mg each), followed by monthly doses of 120 mg.
Recommended Dosing for Episodic Cluster Headache
- 300 mg (administered as three consecutive injections of 100 mg each) at the onset of the cluster period, and then monthly until the end of the cluster period.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding galcanezumab-gnlm Off-Label Guideline-Supported Use and Dosage (Adult) in the drug label.
Non–Guideline-Supported Use
There is limited information regarding galcanezumab-gnlm Off-Label Non-Guideline-Supported Use and Dosage (Adult) in the drug label.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Safety and effectiveness in pediatric patients have not been established.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding galcanezumab-gnlm Off-Label Guideline-Supported Use and Dosage (Pediatric) in the drug label.
Non–Guideline-Supported Use
There is limited information regarding galcanezumab-gnlm Off-Label Non-Guideline-Supported Use and Dosage (Pediatric) in the drug label.
Contraindications
- Galcanezumab-gnlm is contraindicated in patients with serious hypersensitivity to galcanezumab-gnlm or to any of the excipients.
Warnings
Hypersensitivity Reactions
- Hypersensitivity reactions, including anaphylaxis, angioedema, dyspnea, urticaria, and rash, have been reported with galcanezumab-gnlm. If a serious or severe hypersensitivity reaction occurs, discontinue administration of galcanezumab-gnlm and initiate appropriate therapy. Hypersensitivity reactions can occur days after administration and may be prolonged.
Adverse Reactions
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared with rates in clinical trials of another drug and may not reflect the rates observed in clinical practice.
Migraine
- The safety of galcanezumab-gnlm has been evaluated in 2586 patients with migraine who received at least one dose of galcanezumab-gnlm, representing 1487 patient-years of exposure. Of these, 1920 patients were exposed to galcanezumab-gnlm once monthly for at least 6 months, and 526 patients were exposed for 12 months.
- In placebo-controlled clinical studies (Studies 1, 2, and 3), 705 patients received at least one dose of galcanezumab-gnlm 120 mg once monthly, and 1451 patients received placebo, during 3 months or 6 months of double-blind treatment. Of the galcanezumab-gnlm-treated patients, approximately 85% were female, 77% were white, and the mean age was 41 years at study entry.
- The most common adverse reaction was injection site reactions. In Studies 1, 2, and 3, 1.8% of patients discontinued double-blind treatment because of adverse events. TABLE 1 summarizes the adverse reactions that occurred within up to 6 months of treatment in the migraine studies.

Episodic Cluster Headache
- Galcanezumab-gnlm was studied for up to 2 months in a placebo-controlled trial in patients with episodic cluster headache (Study 4). A total of 106 patients were studied (49 on galcanezumab-gnlm and 57 on placebo). Of the galcanezumab-gnlm-treated patients, approximately 84% were male, 88% were white, and the mean age was 47 years at study entry. Two galcanezumab-gnlm-treated patients discontinued double-blind treatment because of adverse events.
- Overall, the safety profile observed in patients with episodic cluster headache treated with galcanezumab-gnlm 300 mg monthly is consistent with the safety profile in migraine patients.
Immunogenicity
- As with all therapeutic proteins, there is potential for immunogenicity. The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease.
- For these reasons, comparison of the incidence of antibodies to galcanezumab-gnlm in the studies described below with the incidence of antibodies in other studies or to other products may be misleading.
- The immunogenicity of galcanezumab-gnlm has been evaluated using an in vitro immunoassay for the detection of binding anti-galcanezumab-gnlm antibodies. For patients whose sera tested positive in the screening immunoassay, an in vitro ligand-binding immunoassay was performed to detect neutralizing antibodies.
- In controlled studies with galcanezumab-gnlm up to 6 months (Study 1, Study 2, and Study 3), the incidence of anti-galcanezumab-gnlm antibody development was 4.8% (33/688) in patients receiving galcanezumab-gnlm once monthly (32 out of 33 of whom had in vitro neutralizing activity). With 12 months of treatment in an open-label study, up to 12.5% (16/128) of galcanezumab-gnlm-treated patients developed anti-galcanezumab-gnlm antibodies, most of whom tested positive for neutralizing antibodies.
- Although anti-galcanezumab-gnlm antibody development was not found to affect the pharmacokinetics, safety or efficacy of galcanezumab-gnlm in these patients, the available data are too limited to make definitive conclusions.
Postmarketing Experience
- The following adverse reactions have been identified during post-approval use of galcanezumab-gnlm. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to galcanezumab-gnlm exposure.
- Immune System Disorders — Anaphylaxis, angioedema.
- Skin and Subcutaneous Tissue Disorders — Rash.
Drug Interactions
There is limited information regarding Galcanezumab-gnlm Drug Interactions in the drug label.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): Risk Summary
- There are no adequate data on the developmental risk associated with the use of galcanezumab-gnlm in pregnant women. Administration of galcanezumab-gnlm to rats and rabbits during the period of organogenesis or to rats throughout pregnancy and lactation at plasma exposures greater than that expected clinically did not result in adverse effects on development (see Animal Data).
- In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% - 4% and 15% - 20%, respectively. The estimated rate of major birth defects (2.2% - 2.9%) and miscarriage (17%) among deliveries to women with migraine are similar to rates reported in women without migraine.
Clinical Considerations
Disease-Associated Maternal and/or Embryo/Fetal Risk
- Published data have suggested that women with migraine may be at increased risk of preeclampsia during pregnancy.
Animal Data
- When galcanezumab-gnlm was administered to female rats by subcutaneous injection in two studies (0, 30, or 100 mg/kg; 0 or 250 mg/kg) prior to and during mating and continuing throughout organogenesis, no adverse effects on embryofetal development were observed. The highest dose tested (250 mg/kg) was associated with a plasma exposure (Cave, ss) 38 or 18 times that in humans at the recommended human dose (RHD) for migraine (120 mg) or episodic cluster headache (300 mg), respectively. Administration of galcanezumab-gnlm (0, 30, or 100 mg/kg) by subcutaneous injection to pregnant rabbits throughout the period of organogenesis produced no adverse effects on embryofetal development. The higher dose tested was associated with a plasma Cave, ss 64 or 29 times that in humans at 120 mg or 300 mg, respectively.
- Administration of galcanezumab-gnlm (0, 30, or 250 mg/kg) by subcutaneous injection to rats throughout pregnancy and lactation produced no adverse effects on pre- and postnatal development. The higher dose tested was associated with a plasma Cave, ss 34 or 16 times that in humans at 120 mg or 300 mg, respectively.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Galcanezumab-gnlm in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Galcanezumab-gnlm during labor and delivery.
Nursing Mothers
Risk Summary
- There are no data on the presence of galcanezumab-gnlm in human milk, the effects on the breastfed infant, or the effects on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for galcanezumab-gnlm and any potential adverse effects on the breastfed infant from galcanezumab-gnlm or from the underlying maternal condition.
Pediatric Use
- Safety and effectiveness in pediatric patients have not been established.
Geriatic Use
- Clinical studies of galcanezumab-gnlm did not include sufficient numbers of patients aged 65 and over to determine whether they respond differently from younger patients.
Gender
There is no FDA guidance on the use of Galcanezumab-gnlm with respect to specific gender populations.
Race
There is no FDA guidance on the use of Galcanezumab-gnlm with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Galcanezumab-gnlm in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Galcanezumab-gnlm in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Galcanezumab-gnlm in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Galcanezumab-gnlm in patients who are immunocompromised.
Administration and Monitoring
Administration
Recommended Dosing for Migraine
- The recommended dosage of galcanezumab-gnlm is 240 mg (two consecutive subcutaneous injections of 120 mg each) once as a loading dose, followed by monthly doses of 120 mg injected subcutaneously.
- If a dose of galcanezumab-gnlm is missed, administer as soon as possible. Thereafter, galcanezumab-gnlm can be scheduled monthly from the date of the last dose.
Recommended Dosing for Episodic Cluster Headache
- The recommended dosage of galcanezumab-gnlm is 300 mg (three consecutive subcutaneous injections of 100 mg each) at the onset of the cluster period, and then monthly until the end of the cluster period.
- If a dose of galcanezumab-gnlm is missed during a cluster period, administer as soon as possible. Thereafter, galcanezumab-gnlm can be scheduled monthly from the date of the last dose until the end of the cluster period.
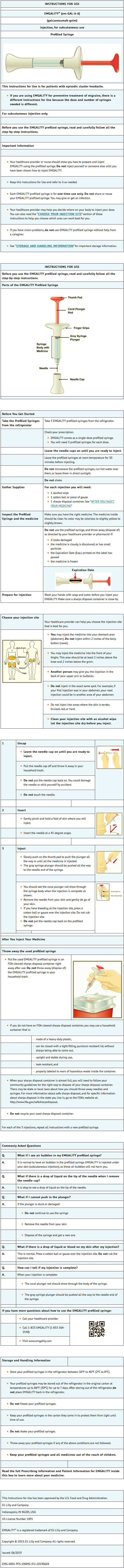
Important Administration Instructions
- Galcanezumab-gnlm is for subcutaneous use only.
- Galcanezumab-gnlm is intended for patient self-administration. Prior to use, provide proper training to patients and/or caregivers on how to prepare and administer galcanezumab-gnlm using the single-dose prefilled pen or single-dose prefilled syringe, including aseptic technique:
- Protect galcanezumab-gnlm from direct sunlight.
- Prior to subcutaneous administration, allow galcanezumab-gnlm to sit at room temperature for 30 minutes. Do not warm by using a heat source such as hot water or a microwave.
- Do not shake the product.
- Inspect galcanezumab-gnlm visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Do not use galcanezumab-gnlm if it is cloudy or there are visible particles.
- Administer galcanezumab-gnlm in the abdomen, thigh, back of the upper arm, or buttocks subcutaneously. Do not inject into areas where the skin is tender, bruised, red, or hard.
- Both the prefilled pen and prefilled syringe are single-dose and deliver the entire contents.
Monitoring
There is limited information regarding Galcanezumab-gnlm Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Galcanezumab-gnlm and IV administrations.
Overdosage
There is limited information regarding Galcanezumab-gnlm overdosage. If you suspect drug poisoning or overdose, please contact the National Poison Help hotline (1-800-222-1222) immediately.
Pharmacology
Mechanism of Action
- Galcanezumab-gnlm is a humanized monoclonal antibody that binds to calcitonin gene-related peptide (CGRP) ligand and blocks its binding to the receptor.
Structure
There is limited information regarding Galcanezumab-gnlm Structure in the drug label.
Pharmacodynamics
- There are no relevant data on the pharmacodynamic effects of galcanezumab-gnlm.
Pharmacokinetics
- Galcanezumab-gnlm exhibits linear pharmacokinetics and exposure increases proportionally with doses between 1 and 600 mg.
- A loading dose of 240 mg achieved the serum galcanezumab-gnlm steady-state concentration after the first dose. A dose of 300 mg monthly would achieve steady-state concentration after the fourth dose. The time to maximum concentration is 5 days, and the elimination half-life is 27 days.
- There was no difference in pharmacokinetic parameters between healthy volunteers, patients with episodic or chronic migraine, and patients with episodic cluster headache.
Absorption
- Following a subcutaneous dose of galcanezumab-gnlm, the time to maximum concentration was about 5 days.
- Injection site location did not significantly influence the absorption of galcanezumab-gnlm.
Distribution
- The apparent volume of distribution (V/F) of galcanezumab-gnlm was 7.3 L (34% Inter Individual Variability [IIV]).
Metabolism and Elimination
- Galcanezumab-gnlm is expected to be degraded into small peptides and amino acids via catabolic pathways in the same manner as endogenous IgG.
- The apparent clearance (CL/F) of galcanezumab-gnlm was 0.008 L/h and the elimination half-life of galcanezumab was approximately 27 days.
Specific Populations
Age, Sex, Weight, Race, Ethnicity
- The pharmacokinetics of galcanezumab-gnlm were not affected by age, sex, race, subtypes of migraine spectrum (episodic or chronic migraine), or headache diagnosis (migraine vs. episodic cluster headache) based on a population pharmacokinetics analysis. Body weight has no clinically relevant effect on the pharmacokinetics of galcanezumab-gnlm.
Patients with Renal or Hepatic Impairment
- Renal and hepatic impairment are not expected to affect the pharmacokinetics of galcanezumab-gnlm. Population pharmacokinetic analysis of integrated data from the galcanezumab-gnlm clinical studies revealed that creatinine clearance did not affect the pharmacokinetics of galcanezumab-gnlm in patients with mild or moderate renal impairment. Patients with severe renal impairment (creatinine clearance <30 mL/min) have not been studied. Based on a population PK analysis, bilirubin concentration did not significantly influence the CL/F of galcanezumab-gnlm.
- No dedicated clinical studies were conducted to evaluate the effect of hepatic impairment or renal impairment on the pharmacokinetics of galcanezumab-gnlm.
Drug Interaction Studies P450 Enzymes
- Galcanezumab-gnlm is not metabolized by cytochrome P450 enzymes; therefore, interactions with concomitant medications that are substrates, inducers, or inhibitors of cytochrome P450 enzymes are unlikely.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
- The carcinogenic potential of galcanezumab-gnlm has not been assessed.
Mutagenesis
- Genetic toxicology studies of galcanezumab-gnlm have not been conducted.
Impairment of Fertility
- When galcanezumab-gnlm (0, 30, or 250 mg/kg) was administered to male rats by subcutaneous injection prior to and during mating, no adverse effects on fertility was observed. The higher dose tested was associated with a plasma exposure (Cave, ss) 8 or 4 times that in humans at the recommended human dose (RHD) for migraine (120 mg) or episodic cluster headache (300 mg), respectively. When galcanezumab-gnlm was administered to female rats by subcutaneous injection in two studies (0, 30, or 100 mg/kg; 0 or 250 mg/kg) prior to and during mating and continuing throughout organogenesis, no adverse effects on fertility were observed. The highest dose tested (250 mg/kg) was associated with a plasma Cave, ss 38 or 18 times that in humans at 120 mg or 300 mg, respectively.
Clinical Studies
Migraine
- The efficacy of galcanezumab-gnlm was evaluated as a preventive treatment of episodic or chronic migraine in three multicenter, randomized, double-blind, placebo-controlled studies: two 6-month studies in patients with episodic migraine (Studies 1 and 2) and one 3-month study in patients with chronic migraine (Study 3).
Episodic Migraine
- Study 1 (NCT02614183) and Study 2 (NCT02614196) included adults with a history of episodic migraine (4 to 14 migraine days per month). All patients were randomized in a 1:1:2 ratio to receive once-monthly subcutaneous injections of galcanezumab-gnlm 120 mg, galcanezumab-gnlm 240 mg, or placebo. All patients in the 120 mg galcanezumab-gnlm group received an initial 240 mg loading dose. Patients were allowed to use acute headache treatments, including migraine-specific medications (i.e., triptans, ergotamine derivatives), NSAIDs, and acetaminophen during the study.
- The studies excluded patients on any other migraine preventive treatment, patients with medication overuse headache, patients with ECG abnormalities compatible with an acute cardiovascular event and patients with a history of stroke, myocardial infarction, unstable angina, percutaneous coronary intervention, coronary artery bypass grafting, deep vein thrombosis, or pulmonary embolism within 6 months of screening.
- The primary efficacy endpoint for Studies 1 and 2 was the mean change from baseline in the number of monthly migraine headache days over the 6-month treatment period. Key secondary endpoints included response rates (the mean percentages of patients reaching at least 50%, 75%, and 100% reduction from baseline in the number of monthly migraine headache days over the 6-month treatment period), the mean change from baseline in the number of monthly migraine headache days with use of any acute headache medication during the 6-month treatment period, and the impact of migraine on daily activities, as assessed by the mean change from baseline in the average Migraine-Specific Quality of Life Questionnaire version 2.1 (MSQ v2.1) Role Function-Restrictive domain score during the last 3 months of treatment (Months 4 to 6). Scores are scaled from 0 to 100, with higher scores indicating less impact of migraine on daily activities.
- In Study 1, a total of 858 patients (718 females, 140 males) ranging in age from 18 to 65 years, were randomized. A total of 703 patients completed the 6-month double-blind phase. In Study 2, a total of 915 patients (781 female, 134 male) ranging in age from 18 to 65 years, were randomized. A total of 785 patients completed the 6-month double-blind phase. In Study 1 and Study 2, the mean migraine frequency at baseline was approximately 9 migraine days per month, and was similar across treatment groups.
- Galcanezumab-gnlm 120 mg demonstrated statistically significant improvements for efficacy endpoints compared to placebo over the 6-month period, as summarized in TABLE 2. Galcanezumab-gnlm treatment with the 240 mg once-monthly dose showed no additional benefit over the galcanezumab-gnlm 120 mg once-monthly dose.



- FIGURE 3 shows the distribution of change from baseline in the mean number of monthly migraine headache days in bins of 2 days, by treatment group, in Study 1. A treatment benefit over placebo for galcanezumab-gnlm is seen across a range of changes from baseline in monthly migraine headache days.

- FIGURE 4 shows the distribution of change from baseline in the mean number of monthly migraine headache days in bins of 2 days, by treatment group, in Study 2. A treatment benefit over placebo for galcanezumab-gnlm is seen across a range of changes from baseline in monthly migraine headache days.

Chronic Migraine
- Study 3 (NCT02614261) included adults with a history of chronic migraine (≥15 headache days per month with ≥8 migraine days per month). All patients were randomized in a 1:1:2 ratio to receive once-monthly subcutaneous injections of galcanezumab-gnlm 120 mg, galcanezumab-gnlm 240 mg, or placebo over a 3-month treatment period. All patients in the 120 mg galcanezumab-gnlm group received an initial 240 mg loading dose.
- Patients were allowed to use acute headache treatments including migraine-specific medications (i.e., triptans, ergotamine derivatives), NSAIDs, and acetaminophen. A subset of patients (15%) was allowed to use one concomitant migraine preventive medication. Patients with medication overuse headache were allowed to enroll.
- The study excluded patients with ECG abnormalities compatible with an acute cardiovascular event, and patients with a history of stroke, myocardial infarction, unstable angina, percutaneous coronary intervention, coronary artery bypass grafting, deep vein thrombosis, or pulmonary embolism within 6 months of screening.
- The primary endpoint was the mean change from baseline in the number of monthly migraine headache days over the 3-month treatment period. The secondary endpoints were response rates (the mean percentages of patients reaching at least 50%, 75% and 100% reduction from baseline in the number of monthly migraine headache days over the 3-month treatment period), the mean change from baseline in the number of monthly migraine headache days with use of any acute headache medication during the 3-month treatment period, and the impact of migraine on daily activities as assessed by the mean change from baseline in the MSQ v2.1 Role Function-Restrictive domain score at Month 3. Scores are scaled from 0 to 100, with higher scores indicating less impact of migraine on daily activities.
- In Study 3, a total of 1113 patients (946 female, 167 male) ranging in age from 18 to 65 years, were randomized. A total of 1037 patients completed the 3-month double-blind phase. The mean number of monthly migraine headache days at baseline was approximately 19.
- Galcanezumab-gnlm 120 mg demonstrated statistically significant improvement for the mean change from baseline in the number of monthly migraine headache days over the 3-month treatment period, and in the mean percentage of patients reaching at least 50% reduction from baseline in the number of monthly migraine headache days over the 3-month treatment period, as summarized in TABLE 3. Galcanezumab-gnlm treatment with the 240 mg once-monthly dose showed no additional benefit over the galcanezumab-gnlm 120 mg once-monthly dose.

- Study 3 utilized a sequential testing procedure to control the Type-I error rate for the multiple secondary endpoints. Once a secondary endpoint failed to reach the required level for statistical significance, formal hypothesis testing was terminated for subsequent endpoints, and p-values were considered nominal only. In Study 3, galcanezumab-gnlm 120 mg was not significantly better than placebo for the proportion of patients with ≥75% or 100% reduction in migraine headache days. Patients treated with galcanezumab-gnlm 120 mg showed a nominally greater reduction in the number of monthly migraine headache days that acute medication was taken (-4.7 for galcanezumab-gnlm 120 mg vs. -2.2 for placebo; nominal p-value <0.001), and the mean change from baseline in the MSQ Role Function-Restrictive Domain score at Month 3 was nominally greater in patients treated with galcanezumab-gnlm 120 mg than in patients on placebo (21.8 for galcanezumab-gnlm 120 mg vs. 16.8 for placebo; nominal p-value <0.001).

- FIGURE 6 shows the distribution of change from baseline in the mean number of monthly migraine headache days for the 3-month study period in bins of 3 days by treatment group. A treatment benefit over placebo for galcanezumab-gnlm is seen across a range of changes from baseline in monthly migraine headache days.

Episodic Cluster Headache
- The efficacy of galcanezumab-gnlm was evaluated for the treatment of episodic cluster headache in a randomized, 8-week, double-blind, placebo-controlled study (Study 4).
- Study 4 (NCT02397473) included adults who met the International Classification of Headache Disorders 3rd edition (beta version) diagnostic criteria for episodic cluster headache and had a maximum of 8 attacks per day, a minimum of one attack every other day, and at least 4 attacks during the prospective 7-day baseline period. All patients were randomized in a 1:1 ratio to receive once-monthly subcutaneous injections of galcanezumab-gnlm 300 mg or placebo. Patients were allowed to use certain specified acute/abortive cluster headache treatments, including triptans, oxygen, acetaminophen, and NSAIDs during the study.
- The study excluded patients on other treatments intended to reduce the frequency of cluster headache attacks; patients with medication overuse headache; patients with ECG abnormalities compatible with an acute cardiovascular event or conduction delay; and patients with a history of myocardial infarction, unstable angina, percutaneous coronary intervention, coronary artery bypass grafting, deep vein thrombosis, or pulmonary embolism within 6 months of screening. In addition, patients with any history of stroke, intracranial or carotid aneurysm, intracranial hemorrhage, or vasospastic angina; clinical evidence of peripheral vascular disease; or diagnosis of Raynaud’s disease were excluded.
- The primary efficacy endpoint for Study 4 was the mean change from baseline in weekly cluster headache attack frequency across Weeks 1 to 3. A secondary endpoint was the percentage of patients who achieved a response (defined as a reduction from baseline of 50% or greater in the weekly cluster headache attack frequency) at Week 3.
- In Study 4, a total of 106 patients (88 males, 18 females) ranging in age from 19 to 65 years were randomized and treated. A total of 90 patients completed the 8-week double-blind phase. In the prospective baseline phase, the mean number of weekly cluster headache attacks was 17.5, and was similar across treatment groups.
- Galcanezumab-gnlm 300 mg demonstrated statistically significant improvements for efficacy endpoints compared to placebo, as summarized in TABLE 4.


- FIGURE 8 shows the distribution of the average percent change from baseline in weekly cluster headache attack frequency across Weeks 1 to 3 in bins of 25%, by treatment group, in Study 4.

How Supplied
- Galcanezumab-gnlm injection is a sterile, preservative-free, clear to opalescent, colorless to slightly yellow to slightly brown solution for subcutaneous administration.
- Galcanezumab-gnlm is not made with natural rubber latex.
- Galcanezumab-gnlm is supplied as follows:

Storage
- Store refrigerated at 2°C to 8°C (36°F to 46°F) in the original carton to protect galcanezumab-gnlm from light until use.
- Do not freeze.
- Do not shake.
- Galcanezumab-gnlm may be stored out of refrigeration in the original carton at temperatures up to 30°C (86°F) for up to 7 days. Once stored out of refrigeration, do not place back in the refrigerator.
- If these conditions are exceeded, galcanezumab-gnlm must be discarded.
- Discard the galcanezumab-gnlm single-dose prefilled pen or syringe after use in a puncture-resistant container.
Images
Drug Images
{{#ask: Page Name::Galcanezumab-gnlm |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel



{{#ask: Label Page::Galcanezumab-gnlm |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- Instructions on Self-Administration: Provide guidance to patients and/or caregivers on proper subcutaneous injection technique, including aseptic technique, and how to use the prefilled pen or prefilled syringe correctly [see Instructions for Use]. Instruct patients and/or caregivers to read and follow the Instructions for Use each time they use galcanezumab-gnlm.
- Hypersensitivity Reactions: Advise patients to seek immediate medical attention if they experience any symptoms of serious or severe hypersensitivity reactions.
- For more information go to www.EMGALITY.com or call 1-833-EMGALITY (1-833-364-2548).
Patient Package Insert

Instructions for Use


Precautions with Alcohol
Alcohol-Galcanezumab-gnlm interaction has not been established. Talk to your doctor regarding the effects of taking alcohol with this medication.
Brand Names
Look-Alike Drug Names
There is limited information regarding Galcanezumab-gnlm Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.