Chronic stable angina treatment blood pressure control
|
Chronic stable angina Microchapters | ||
|
Classification | ||
|---|---|---|
| ||
| ||
|
Differentiating Chronic Stable Angina from Acute Coronary Syndromes | ||
|
Diagnosis | ||
|
Alternative Therapies for Refractory Angina | ||
|
Discharge Care | ||
|
Guidelines for Asymptomatic Patients | ||
|
Case Studies | ||
|
Chronic stable angina treatment blood pressure control On the Web | ||
|
FDA on Chronic stable angina treatment blood pressure control | ||
|
CDC onChronic stable angina treatment blood pressure control | ||
|
Chronic stable angina treatment blood pressure control in the news | ||
|
Blogs on Chronic stable angina treatment blood pressure control | ||
|
to Hospitals Treating Chronic stable angina treatment blood pressure control | ||
|
Risk calculators and risk factors for Chronic stable angina treatment blood pressure control | ||
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: Lakshmi Gopalakrishnan. M.B.B.S.; Aysha Anwar, M.B.B.S[2]
Overview
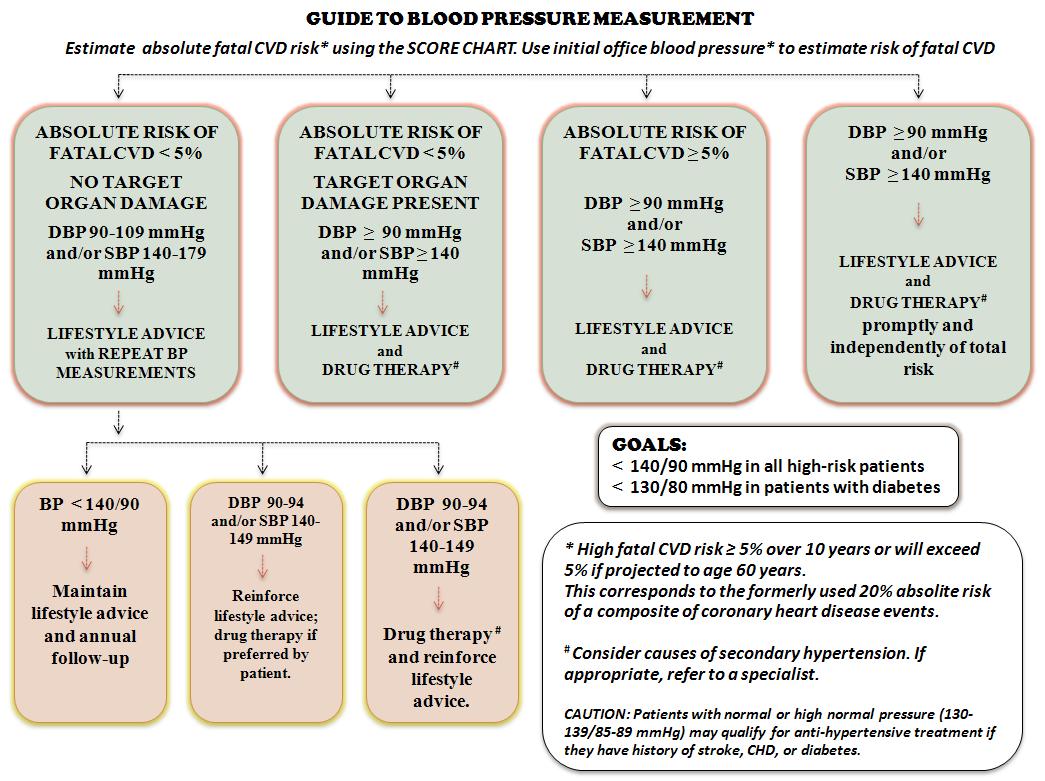
The risk of progression of atherosclerosis is proportional to the increase in elevated blood pressure, hyperglycemia and dyslipidemia. Therefore, the control of hypertension, hyperglycemia and other features of metabolic syndrome deserves special attention in the prevention of mortality and morbidity due to coronary artery disease. In patients with established CAD, concomitant diabetes and/or renal dysfunction, the blood pressure goal is 130/80-85 and the decision to lower blood pressure depends on the total cardiovascular risk and the extent of target organ damage.[1][2] Close monitoring and lifestyle changes may be indicated in low-risk patients without documented target organ damage. However, in high-risk patients with a sustained SBP of ≥140 mm Hg and/or DBP ≥90 mm Hg, the goal is to lower blood pressure less than 140/90 with the help of combined drug therapy and life style modification. Anti-hypertensive therapies that have shown to significantly reduce cardiovascular mortality and morbidity in patients with coronary artery disease include diuretics, beta-blockers, ACEIs, ARBs and calcium channel blockers.
Blood Pressure Control
Guide to Blood Pressure Management adapted from the European Task Force[1]
| “ |
 |
” |
2012 Chronic Angina Guidelines for the Management of Patients With Chronic Stable Angina (DO NOT EDIT)
Blood Pressure Control (DO NOT EDIT)[3]
| Class I |
| "1. All patients should be counseled about the need for lifestyle modification: weight control; increased physical activity; alcohol moderation; sodium reduction; and emphasis on increased consumption of fresh fruits, vegetables, and low-fat dairy products. (Level of Evidence: B)" |
| "2. In patients with SIHD with blood pressure 140/90 mm Hg or higher, antihypertensive drug therapy should be instituted in addition to or after a trial of lifestyle modifications (Level of Evidence: A)" |
| "3. The specific medications used for treatment of high blood pressure should be based on specific patient characteristics and may include angiotensin-converting enzyme (ACE) inhibitors and/or beta blockersblockers, with addition of other drugs, such as thiazide diuretics or calcium channel blockers, if needed to achieve a goal blood pressure of less than 140/90 mm Hg. (Level of Evidence: B)" |
References
- ↑ 1.0 1.1 De Backer G, Ambrosioni E, Borch-Johnsen K, Brotons C, Cifkova R, Dallongeville J et al. (2003) European guidelines on cardiovascular disease prevention in clinical practice. Third Joint Task Force of European and Other Societies on Cardiovascular Disease Prevention in Clinical Practice. Eur Heart J 24 (17):1601-10. PMID: 12964575
- ↑ European Society of Hypertension-European Society of Cardiology Guidelines Committee (2003) 2003 European Society of Hypertension-European Society of Cardiology guidelines for the management of arterial hypertension. J Hypertens 21 (6):1011-53. DOI:10.1097/01.hjh.0000059051.65882.32 PMID: 12777938
- ↑ Fihn SD, Gardin JM, Abrams J, Berra K, Blankenship JC, Dallas AP; et al. (2012). "2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: executive summary: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons". Circulation. 126 (25): 3097–137. doi:10.1161/CIR.0b013e3182776f83. PMID 23166210.