Arcuate uterus
| Arcuate uterus | |
 | |
|---|---|
| Arcuate uterus (Image courtesy of RadsWiki) | |
| ICD-10 | Q51.9 |
| ICD-9 | 752.9 |
|
WikiDoc Resources for Arcuate uterus |
|
Articles |
|---|
|
Most recent articles on Arcuate uterus Most cited articles on Arcuate uterus |
|
Media |
|
Powerpoint slides on Arcuate uterus |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Arcuate uterus at Clinical Trials.gov Trial results on Arcuate uterus Clinical Trials on Arcuate uterus at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Arcuate uterus NICE Guidance on Arcuate uterus
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Arcuate uterus Discussion groups on Arcuate uterus Patient Handouts on Arcuate uterus Directions to Hospitals Treating Arcuate uterus Risk calculators and risk factors for Arcuate uterus
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Arcuate uterus |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
The arcuate uterus is a form of a uterine anomaly or variation where the uterine fundus displays a concave contour towards the uterine cavity. Normally the fundus of the uterus is straight or convex on anterior-posterior imaging but in the arcuate uterus it dips into the cavity and may form a small septation. The distinction between an arcuate uterus and a septate uterus is not standardized.
Etiology
The uterus is formed during embryogenesis by the fusion of the two mullerian ducts. During this fusion a resorption process eliminates the partition between the two ducts to create a single cavity. This process begins caudally and advances cranially, thus an arcuate uterus represents an in the final stage incomplete absorption process.
Prevalence
Most studies of uterine malformations are based on populations of women who have experienced a pregnancy loss and thus do not address the issue of the prevalence in the general population. A screening study by Woelfer at al. of women without a history of reproductive problems found that about 5% of women had an arcuate uterus when they defined an arcuate uterus any fundal protrusion into the cavity that had an apical angle of more than 90 degrees. Accodingly it was the most common uterine anomaly, followed by uterine septum (3%) and bicornuate uterus (0.5%).[1]
Clinical presentation
The condition may not be known to the affected individual and not result in any reproductive problems; thus normal pregnancies occur.[2] Indeed, there is no consensus on the relationship of the arcuate uterus and recurrent pregnancy loss.[3] Accordingly, the condition may be a variation or a pathology.
One view maintains that the condition is associated with a higher risk for miscarriage, premature birth, and malpresentation. Thus a study that evaluated women with uterine bleeding by hysteroscopy found that 6.5 % of subjects displayed the arcuate uterus and had evidence of reproductive impairments. [4] A study based on hysterosalpingraphic detected arcuate lesions documented increased fetal loss and obstetrical complications as a risk for affected women.[5] Woelfer found that the miscarriage risk is more pronounced in the second trimester.[1] In contrast, a study utilizing 3-D ultrasonography to document the prevalence of the arcuate uterus in a gynecological population found no evidnce of increased risk of reproductive loss; in this study 3.1% of women had an arcuate uterus making it the most common uterine anomaly; this prevalence was similar than in women undergoing sterilization and lower than in women with recurrent pregnancy loss.[6]
Diagnosis
A pelvic examination will not reveal the condition. Investigations are usually prompted on the basis of reproductive problems.
Helpful techniques to investigate the uterine structure are transvaginal ultrasonography and sonohysterography, hysterosalpingography, MRI, and hysteroscopy. More recently 3-D ultrasonography has been advocated as an excellent non-invasive method to delineate the condition.[1]
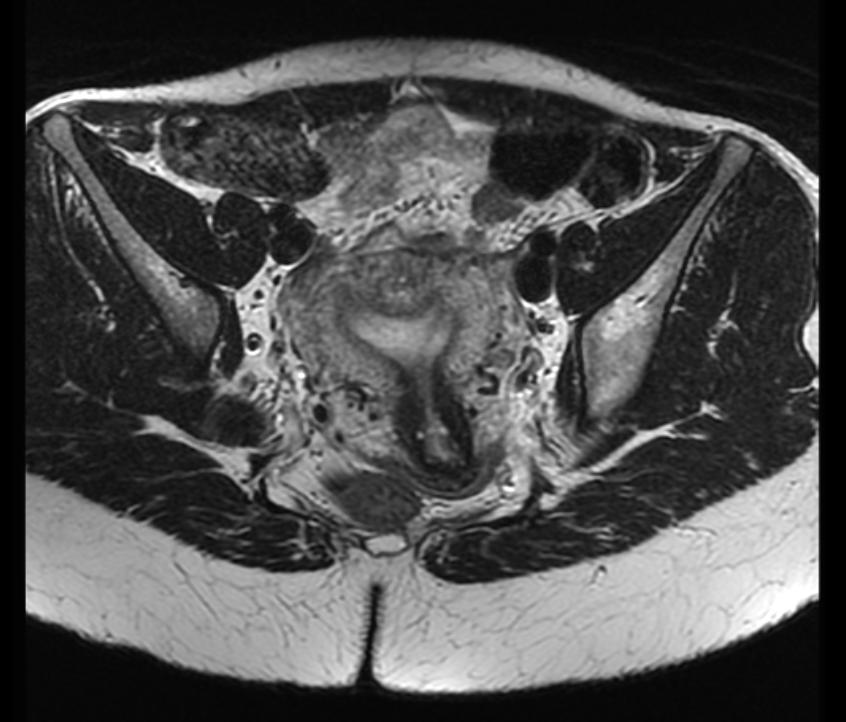
MRI
-
MR image demonstrates an arcuate uterus
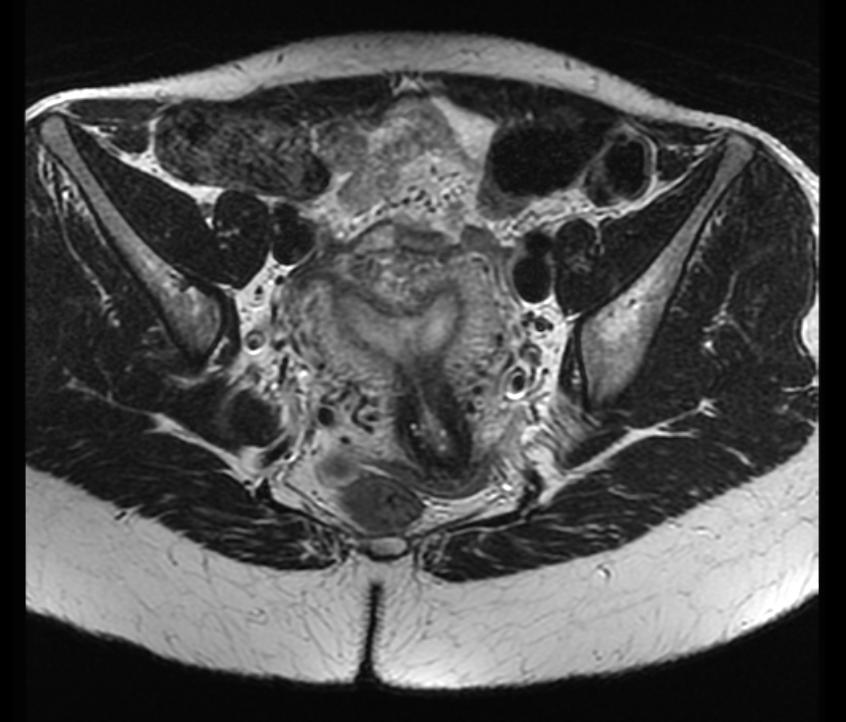
-
MR image demonstrates an arcuate uterus
Management
Many patients with an arcuate uterus will not experience any reproductive problems and do not require any surgery. In patients with recurrent pregnancy loss thought to be caused by an arcuate uterus hysteroscopic resection can be performed.
Differential diagnosis
The major differential diagnosis is the uterine septum. The lack of agreement to separate these two entities makes it difficult to assess the results in the literature.
References
- ↑ 1.0 1.1 1.2 Woelfer B, Salim R, Banerjee S, Elson J, Regan L, Jurkovic D (2001). "Reproductive outcomes in women with congenital uterine anomalies detected by three-dimensional ultrasound screening". Obstet Gynecol. 98 (6): 1099–103. PMID 11755560.
- ↑ Creasy RK, Resnik R. Maternal-Fetal Medicine. Principles and Practice. W.B.Saunders, Philadelphia (1994)p.447. ISNB 0-7216-6590-0
- ↑ ACOG. "Management of Recurrent Early Pregnancy Loss". Practice Bulletin Number 24, 2001, page 3.
- ↑ Maneschi F, Zupi E, Marconi D, Valli E, Romanini C, Mancuso S (1995). "Hysteroscopically detected asymptomatic müllerian anomalies. Prevalence and reproductive implications". J Reprod Med. 40 (10): 684–8. PMID 8551467.
- ↑ Sørensen SS, Trauelsen AG (1987). "Obstetric implications of minor müllerian anomalies in oligomenorrheic women". Am. J. Obstet. Gynecol. 156 (5): 1112–8. PMID 3578421.
- ↑ Jurkovic D, Gruboeck K, Tailor A, Nicolaides KH (1997). "Ultrasound screening for congenital uterine anomalies". Br J Obstet Gynaecol. 104 (11): 1320–1. PMID 9386036.
See Also
- Mullerian duct anomalies classification system
- Bicornuate uterus
- Septate uterus
- Unicornuate uterus
- Uterus didelphys
Additional Resource
- Robert N. Troiano, and Shirley M. McCarthy. Müllerian Duct Anomalies: Imaging and Clinical Issues. Radiology 2004 233: 19-34.