Tularemia laboratory findings: Difference between revisions
(Created page with "__NOTOC__ {{Tularemia}} {{CMG}} ==Laboratory Findings== [[Image:F. tularensis SCHU strain.jpg|thumb|right|F. tularensis SCHU stain on 6% sheep blood agar (SBA), 72 h. Note it...") |
m (Changes made per Mahshid's request) |
||
| (10 intermediate revisions by 2 users not shown) | |||
| Line 3: | Line 3: | ||
{{CMG}} | {{CMG}} | ||
==Overview== | |||
There are a variety of lab diagnostic tests used to diagnose tularemia including [[Gram staining|Gram]] stains, bacteria cultures, [[biochemical]],and [[Fluorescent antibody|antibody fluorescence]] tests. Gram stains and bacteria cultures are useful in identifying F.tularensis. Unfortunately, these diagnostics offer difficult interpretations with extensive procedures. Antibody fluorescence allows for quick and effective testing. This method is extraordinarily important in diagnosing [[Pneumonia (patient information)|pneumonic]] variations of tularemia, as these variations are often associated with a higher mortality rate. | |||
==Laboratory Findings== | ==Laboratory Findings== | ||
===Stains and smears=== | |||
* | ====[[Gram stain]]==== | ||
*Staining of ''F. tularensis'' often reveals the presence of tiny, 0.2-0.5-μm X 0.7-1.0 μm, [[pleomorphic]], poorly staining, [[gram-negative]] [[coccobacilli]] seen mostly as single cells. | |||
*The [[Gram stain]] interpretation may be difficult because the cells are minute and faintly staining. | |||
*F. tularensis cells are smaller than [[Haemophilus influenzae]]. | |||
*Bipolar staining is not a distinctive feature of F. tularensis cells. | |||
*Additional work: Another smear may be prepared for referral to your state public health laboratory. <ref name="ID FT">Protocol for the Presumptive Identification of Francisella tularensis. https://www.ok.gov/health2/documents/Francisella_tularensis%202-15-13.pdf Accessed March 8, 2016. </ref> | |||
===Cultures=== | |||
*Established [[inoculation]] and plating procedures are used. For tissues, established laboratory procedure is used to inoculate media (e.g., grind, touch-preparation, or a sterile wood stick). Plates are taped shut in 2 places to prevent inadvertent opening (alternate to taping is acceptable). | |||
*Incubation of cultures. | |||
*:*Temperature: 35-37°C | |||
*:*Atmosphere: Ambient, use of 5% CO2 is acceptable. | |||
*:*Length of incubation: primary plates are held for 5 days. If it is known that if a patient has been treated with [[bacteriostatic]] antibiotics, then plates are held for up to 7 days to allow bacteria recovery time. | |||
* | *''F. tularensis'' grows in commercial blood culture media. | ||
*These organisms require [[cysteine]] supplementation; therefore, ''F. tularensis'' may at first grow on SBA, but upon subsequent passage will fail to grow on standard SBA. *On cysteine supplemented agar plates, it is a gray-white, opaque colony, usually too small to be seen at 24 h on most general media such as CA, TM, and BCYE. | |||
*After incubation for 48 h or more, colonies are about 1-2 mm in diameter, white to grey to bluish-grey, opaque, flat, with an entire edge, smooth, and have a shiny surface. | |||
*''F. tularensis'' will not grow on [[MacConkey agar|MacConkey]] or [[Eosin methylene blue|Eosin methylene blue agar]] plates. <ref name="ID FT">Protocol for the Presumptive Identification of Francisella tularensis. https://www.ok.gov/health2/documents/Francisella_tularensis%202-15-13.pdf Accessed March 8, 2016. </ref> | |||
{| | |||
|- | |||
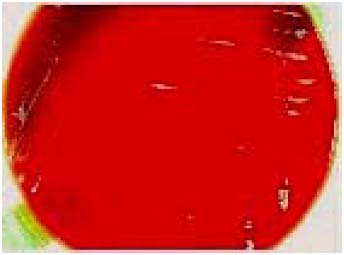
| [[Image:F. tularensis SCHU strain.jpg|thumb|center|F. tularensis SCHU stain on 6% sheep blood agar (SBA), 72 h. Note its inability to grow well on SBA.]] | |||
|| | |||
| [[Image:F. tularensis SCHU strain on chocolate.jpg|thumb|center|F. tularensis SCHU stain on chocolate agar, 72 h]] | |||
|} | |||
* | ===Biochemical reactions/tests=== | ||
*Procedure: Use established laboratory procedures for [[catalase]], [[oxidase]],[[beta-lactamase]], XV (or satellite), and [[urease]] tests. | |||
*Interpretation: According to established laboratory practice. | |||
*Additional notes: Commercial [[biochemical]] identification systems are not recommended at this stage. <ref name="ID FT">Protocol for the Presumptive Identification of Francisella tularensis. https://www.ok.gov/health2/documents/Francisella_tularensis%202-15-13.pdf Accessed March 8, 2016. </ref> | |||
==References== | ==References== | ||
| Line 37: | Line 49: | ||
[[Category:Zoonoses]] | [[Category:Zoonoses]] | ||
[[Category:Biological weapons]] | [[Category:Biological weapons]] | ||
[[Category: | |||
[[Category:Needs overview]] | |||
Latest revision as of 19:04, 18 September 2017
|
Tularemia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Tularemia laboratory findings On the Web |
|
American Roentgen Ray Society Images of Tularemia laboratory findings |
|
Risk calculators and risk factors for Tularemia laboratory findings |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
There are a variety of lab diagnostic tests used to diagnose tularemia including Gram stains, bacteria cultures, biochemical,and antibody fluorescence tests. Gram stains and bacteria cultures are useful in identifying F.tularensis. Unfortunately, these diagnostics offer difficult interpretations with extensive procedures. Antibody fluorescence allows for quick and effective testing. This method is extraordinarily important in diagnosing pneumonic variations of tularemia, as these variations are often associated with a higher mortality rate.
Laboratory Findings
Stains and smears
Gram stain
- Staining of F. tularensis often reveals the presence of tiny, 0.2-0.5-μm X 0.7-1.0 μm, pleomorphic, poorly staining, gram-negative coccobacilli seen mostly as single cells.
- The Gram stain interpretation may be difficult because the cells are minute and faintly staining.
- F. tularensis cells are smaller than Haemophilus influenzae.
- Bipolar staining is not a distinctive feature of F. tularensis cells.
- Additional work: Another smear may be prepared for referral to your state public health laboratory. [1]
Cultures
- Established inoculation and plating procedures are used. For tissues, established laboratory procedure is used to inoculate media (e.g., grind, touch-preparation, or a sterile wood stick). Plates are taped shut in 2 places to prevent inadvertent opening (alternate to taping is acceptable).
- Incubation of cultures.
- Temperature: 35-37°C
- Atmosphere: Ambient, use of 5% CO2 is acceptable.
- Length of incubation: primary plates are held for 5 days. If it is known that if a patient has been treated with bacteriostatic antibiotics, then plates are held for up to 7 days to allow bacteria recovery time.
- F. tularensis grows in commercial blood culture media.
- These organisms require cysteine supplementation; therefore, F. tularensis may at first grow on SBA, but upon subsequent passage will fail to grow on standard SBA. *On cysteine supplemented agar plates, it is a gray-white, opaque colony, usually too small to be seen at 24 h on most general media such as CA, TM, and BCYE.
- After incubation for 48 h or more, colonies are about 1-2 mm in diameter, white to grey to bluish-grey, opaque, flat, with an entire edge, smooth, and have a shiny surface.
- F. tularensis will not grow on MacConkey or Eosin methylene blue agar plates. [1]
 |
 |
Biochemical reactions/tests
- Procedure: Use established laboratory procedures for catalase, oxidase,beta-lactamase, XV (or satellite), and urease tests.
- Interpretation: According to established laboratory practice.
- Additional notes: Commercial biochemical identification systems are not recommended at this stage. [1]
References
- ↑ 1.0 1.1 1.2 Protocol for the Presumptive Identification of Francisella tularensis. https://www.ok.gov/health2/documents/Francisella_tularensis%202-15-13.pdf Accessed March 8, 2016.