Systemic lupus erythematosus (patient information)
For the WikiDoc page for this topic, click here
| Lupus Erythematosus | |
 | |
|---|---|
| Typical "butterfly"-like rash over the cheeks in lupus | |
| ICD-10 | L93, M32 |
| ICD-9 | 710.0 |
| OMIM | 152700 |
| DiseasesDB | 12782 |
| eMedicine | med/ |
| MeSH | D008180 |
|
Systemic lupus erythematosus |
|
Where to find medical care for Systemic lupus erythematosus? |
|---|
|
Systemic lupus erythematosus On the Web |
|
Directions to Hospitals Treating Systemic lupus erythematosus |
|
Risk calculators and risk factors for Systemic lupus erythematosus |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Jinhui Wu, MD Associate Editor-In-Chief: Ujjwal Rastogi, MBBS [2]
Overview
Lupus is an autoimmune disease characterized by acute and chronic inflammation of various tissues of the body. It may affect the skin, joints, kidneys, even brain, heart and lugs. The underlying cause of systemic lupus erythematosus is not clear. Clinical data show it affects nine times as many women as men. Common symptoms include fatigue, low fever, muscle pain, joint pain, lost of appetite, facial butterfly rash, sensitivity to sunlight, chest pain, and swollen lymph nodes. The patient may be diagnosed systemic lupus erythematosus when he/she appears 4 or more of 11 creteria designated by the American College of Rheumatology (ACR). Treatment of systemic lupus erythematosus depends on symptoms. The aim of medications is to relieve the symptoms and decrease the inflammation. Outcomes have improved in recent years. Now the 10-year survival rate for systemic lupus erythematosus patients is greater than 85%.
What are the symptoms?
Symptoms of systemic lupus erythematosus vary from person to person, depending the organs affected. And the symptoms may come and go.
- The most common symptoms of systemic lupus erythematosus
- Fatigue
- Low fever
- Muscle pain
- Joint pain
- Loss of appetite
- Facial butterfly rash
- Sensitivity to sunlight
- Chest pain
- Swollen lymph nodes
- Abnormal blood clotting
- Other symptoms depends on the orgnas affected.
- Headache, new paralysis, or seizures
- Personality change, even psychosis
- Arrhythmias
- Abdominal pain, nausea or vomiting
- Hematuria
-
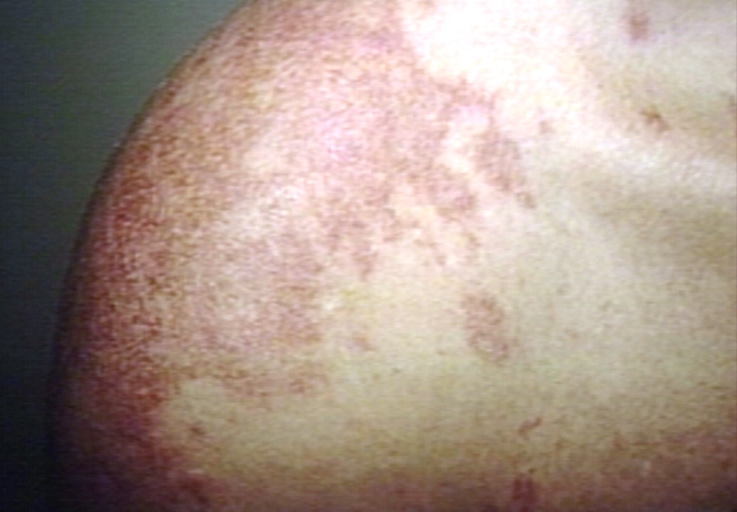
Skin: Lupus, systemic erythematosus; Discoid skin lesion in patient with SLE
-
Skin: ulcer, necrotic; lupus anticoagulant in thigh
-
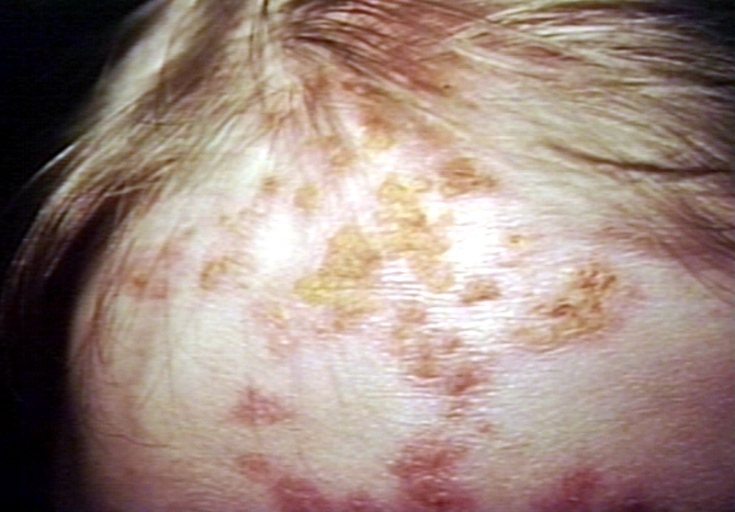
Skin: lupus, erythematosus, subacute; Papulosquamous diseases
-
Skin: lupus, erythematosus; Papulosquamous diseases
-
Skin: lupus, erythematosus; papulosquamous diseases
-
Skin: alopecia, secondary lupus erythematosus; hair loss
-
Skin: discoid lupus, face
Diseases that can have similar symptoms are
Who is at highest risk?
The underlying cause of this autoimmune disease is not clear. Clinical data show the onset of systemic lupus erythematosus is associated with the following factors:
- Female: SLE affects nine times as many women as men.
- Age: From 10 to 50
- Race: African Americans and Asians are affected more often than people from other races.
- Drugs, such as chlorpromazine, hydralazine, isoniazid, methyldopa, penicillamine, procainamide, quinidine and sulfasalazine.
When to seek urgent medical care?
Call your health care provider if you develop symptoms of systemic lupus erythematosus.
Diagnosis
The American College of Rheumatology has designated 11 criteria for classification. If the patient has four or more criteria, he/she can be diagnosed systemic lupus erythematosus.
- Malar rash: This butterfly rash below the eyes may be flat or elevated.
- Discoid rash: These are red, raised patches with scaling of the overlying skin. A subgroup of patients have "discoid lupus" with only skin involvement and do not have systemic lupus erythematosus. All patients with discoid lupus should be screened for systemic involvement.
- Sensitivity to sunligh: A rash develops in response to sun exposure.
- Oral ulcers: The doctor can observe painless sores in the nose or mouth.
- Arthritis: The arthritis of lupus usually demonstrate swelling and tenderness of the joints.
- Serositis: This means an inflammation of various "sacs" or membranes, such as pericarditis, pleurisy or peritonitis. Patients with these inflammations may demonstrate symptoms such as pain, shortness of breath, or forced posture.
- Kidney disease: Patients with lupus may demonstrate persistent loss of protein, or inflammation during analysis of the urine.
- Neurological disorder: Patients with lupus may show paralysis, or seizures, personality change, even psychosis.
- Blood disorder: Patients with lupus may show low blood counts of various blood components.
- Immunologic disorder: Some antibodies tests may be positive in patients with lupus. It includes antibody tests such as anti-double strand (ds) DNA, anti-phospholipid antibodies and anti-smith antibodies.
- Positive antinuclear antibody: It is a very valuable test to rule out lupus. More than 98% of patients with lupus have a positive ANA test result.
Treatment options
Symptoms of systemic lupus erythemtosus may come and go. The aim of treatments is to relieve your symptoms and decrease the inflammation.
- General management:
- Avoid sun exposure: Patients with systemic lupus erythematosus should better prevent from sun exposure. When going out, they are recommended to use sunscreen with higher SPF (at least 15). Wearing protective clothing is also an importsnt way.
- Keep a good sleep quality: This may help decrease fatigue in patients with systemic lupus erythematosus.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): NSAIDs may be used to control inflammation and pain in patients with arthritis or pleurisy with systemic lupus erythematosus. Usual drugs include ibuprofen, naproxen and indomethacin. Usual side effects are pain, bleeding and ulcers in upper gastrointestinal tract.
- Corticosteroids: Corticosteroids can be used to control many symptoms such as pain and rash. Side effects of corticosteroids may include a decreased ability against infection, worse healing in the wound and osteoporosis.
- Cytotoxic drugs: These kind of drugs are used to treat patients without good respond to corticosteroids and always used in active peroid of systemic lupus erythematosus. They may interfere with growth of normal and neoplastic cells by cross-linking of DNA or RNA or proteins. Usual drugs include cyclophosphamide and azathioprine. Side effects include marrow suppression, liver damage, nausea and vomiting.
- For patients with severe organ damage such as heart, central nervous system, kindeys and lungs, treatment team may include the rheumatologist and other specialists.
Where to find medical care for systemic lupus erythematosus?
Directions to Hospitals Treating systemic lupus erythematosus
Prevention of systemic lupus erythematosus
The cause of autoimmue disease is not clear, there is no way to prevent systemic lupus erythematosus.
What to expect (Outlook/Prognosis)?
Outcomes of patients with systemic lupus erythematosus have improved in recent years. Prognosis of systemic lupus erythematosus depends on:
- The results of anti-phospholipid antibodies: Positive results may increase the possibility of pregnancy loss in women with systemic lupus erythematosus.
- Whether the patient is involved of vital organs damage, such as the damages in brain, lungs, heart, and kidney.