|
|
| (22 intermediate revisions by 5 users not shown) |
| Line 1: |
Line 1: |
| | __NOTOC__ |
| | '''For patient information click [[Subdural hematoma (patient information)|here]]''' |
| | |
| {{Infobox_Disease | | | {{Infobox_Disease | |
| Name = {{PAGENAME}} | | | Name = {{PAGENAME}} | |
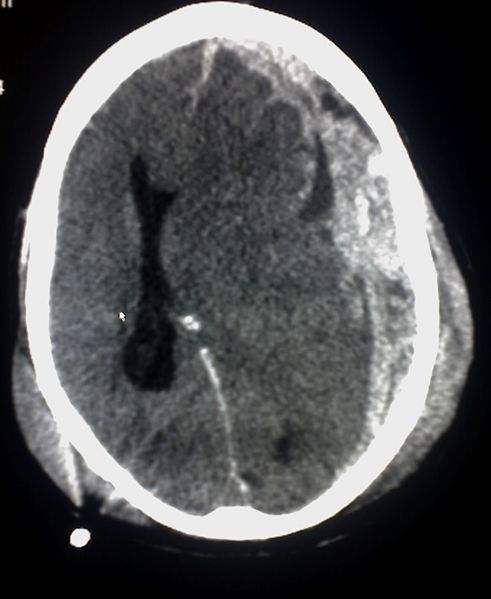
| Image = Trauma subdural.jpg | | | Image = Trauma subdural.jpg | |
| Caption = |
| |
| DiseasesDB = 12614 |
| |
| ICD10 = {{ICD10|I|61|0|i|60}}, {{ICD10|S|06|5|s|00}} |
| |
| ICD9 = {{ICD9|852.2}} - traumatic; {{ICD9|432.1}} - nontraumatic |
| |
| ICDO = |
| |
| OMIM = |
| |
| MedlinePlus = 000713 |
| |
| eMedicineSubj = neuro |
| |
| eMedicineTopic = 575 |
| |
| MeshID = D006408 |
| |
| }} | | }} |
| {{SI}} | | {{Subdural hematoma}} |
| {{CMG}} | | {{CMG}} {{AE}}, {{Fs}} |
| | |
| {{EH}} | |
| | |
| A '''subdural [[hematoma]]''' (Subdural haematoma) (SDH) is a form of [[traumatic brain injury]] in which [[blood]] gathers between the [[dura mater|dura]] (the outer protective covering of the [[brain]]) and the [[arachnoid (brain)|arachnoid]] (the middle layer of the [[meninges]]). Unlike in [[epidural hematomas]], which are usually caused by tears in [[artery|arteries]], subdural bleeding usually results from tears in veins that cross the [[subdural space]]. This bleeding often separates the dura and the arachnoid layers. Subdural hemorrhages may cause an increase in [[intracranial pressure]] (ICP), which can cause compression of and damage to delicate brain tissue. Acute subdural hematoma (ASDH) has a high mortality rate and is a severe [[medical emergency]]. ''
| |
| | |
| ==Causes==
| |
| '''Subdural hematomas''' are most often caused by [[head injury]], when fast changing [[velocity|velocities]] within the [[skull]] may stretch and tear small bridging [[vein]]s. Subdural hematomas due to head injury are described as [[Physical trauma|traumatic]]. Much more common than [[epidural hemorrhage]]s, subdural hemorrhages generally result from shearing injuries due to various rotational or linear forces.<ref name="UVT">University of Vermont College of Medicine. [http://web.archive.org/web/20030821142023/http://cats.med.uvm.edu/cats_teachingmod/pathology/path302/np/home/neuroindex.html "Neuropathology: Trauma to the CNS."] Accessed through web archive on [[August 8]], [[2007]]. </ref><ref name="wagner">Wagner AL. 2004. [http://www.emedicine.com/radio/topic664.htm "Subdural hematoma."] Emedicine.com. Retrieved on [[August 8]], [[2007]]. </ref> It is also commonly seen in the elderly and in alcoholics, who have evidence of brain atrophy. Cerebral atrophy increases the length the bridging veins have to traverse between the two meningeal layers, hence increasing the likelihood of shearing forces causing a tear. It is also more common in patients on anticoagulants, especially Aspirin and Warfarin. Patients on these medications can have a subdural hematoma with a minor injury.
| |
| | |
| ==Signs and symptoms==
| |
| Symptoms of subdural hemorrhage have a slower onset than those of [[epidural hemorrhage]]s because the lower pressure veins bleed more slowly than arteries. Thus, signs and symptoms may show up within 24 hours but can be delayed as much as 2 weeks.<ref name="Sanders and McKenna">Sanders MJ and McKenna K. 2001. ''Mosby’s Paramedic Textbook'', 2nd revised Ed. Chapter 22, "Head and facial trauma." Mosby.</ref> If the bleeds are large enough to put pressure on the brain, signs of increased [[intracranial pressure|ICP]] or damage to part of the brain will be present.<ref name="wagner"/> (Dr.Gill Mohinder MD)
| |
|
| |
| Other [[signs]] and [[symptom]]s of subdural hematoma include the following:
| |
| <div style="-moz-column-count:2; column-count:2;">
| |
| * A history of recent [[head injury]]
| |
| * Loss of [[consciousness]] or fluctuating levels of consciousness
| |
| * Irritability
| |
| * [[Seizures]]
| |
| * [[Numbness]]
| |
| * [[Headache]] (either constant or fluctuating)
| |
| * [[Dizziness]]
| |
| * [[Disorientation]]
| |
| * [[Amnesia]]
| |
| * Weakness or [[lethargy]]
| |
| * [[Nausea]] or [[vomit|vomiting]]
| |
| * Personality changes
| |
| * [[Dysphasia|Inability to speak]] or [[dysarthria|slurred speech]]
| |
| * [[Ataxia]], or difficulty walking
| |
| * Altered breathing patterns
| |
| * Blurred Vision
| |
| * [[Deviated gaze]], or abnormal movement of the eyes.<ref name="wagner"/>
| |
| </div>
| |
|
| |
|
| ==Features== | | {{SK}} Subdural haematoma |
| Most of the time, subdural hematomas occur around the tops and sides of the [[frontal lobe|frontal]] and [[parietal lobe]]s.<ref name="UVT"/><ref name="wagner"/> They also occur in the posterior [[fossa]], and near the [[falx cerebri]] and [[tentorium]].<ref name="wagner"/> Unlike [[epidural hematoma]]s, which cannot expand past the [[skull suture|sutures of the skull]], subdural hematomas can expand along the inside of the skull, creating a convex shape that follows the curve of the brain, stopping only at the [[dural reflection]]s like the tentorium and falx cerebri.
| | ==[[Subdural hematoma overview|Overview]]== |
| | ==[[Subdural hematoma historical perspective|Historical Perspective]]== |
|
| |
|
| On a [[CT scan]], subdural hematomas are crescent-shaped, with a concave surface away from the skull. Subdural blood can also be seen as a layering density along the [[tentorium cerebelli]]. This can be a chronic, stable process, since the feeding system is low-pressure. In such cases, subtle signs of bleeding such as effacement of [[sulcus (anatomy)|sulci]] or medial displacement of the junction between [[gray matter]] and [[white matter]] may be apparent. A chronic bleed can be the same density as brain tissue (called [[isodense]] to brain), meaning that it will show up on CT scan as the same shade as brain tissue, potentially obscuring the finding.
| | ==[[Subdural hematoma classification|Classification]]== |
|
| |
|
| ==Subtypes== | | ==[[Subdural hematoma pathophysiology|Pathophysiology]]== |
| Subdural hematomas are divided into [[Acute (medical)|acute]], subacute, and [[chronic (medicine)|chronic]], depending on their speed of onset. Acute subdural hematomas that are due to trauma are the most lethal of all head injuries and have a high [[mortality rate]] if they are not rapidly treated with surgical decompression.
| |
|
| |
|
| Acute bleeds develop after high speed acceleration or deceleration injuries and are increasingly severe with larger hematomas. They are most severe if associated with [[cerebral contusion]]s.<ref name="wagner"/> Though much faster than chronic subdural bleeds, acute subdural bleeding is usually venous and therefore slower than the usually arterial bleeding of an [[epidural hemorrhage]]. Acute subdural bleeds have a high mortality rate, higher even than epidural hematomas and [[diffuse brain injury|diffuse brain injuries]], because the velocities necessary to cause them cause other severe injuries as well.<ref>Vinas F.C. and Pilitsis J. 2006. [http://www.emedicine.com/med/topic2888.htm Penetrating Head Trauma]. Emedicine.com.</ref> The mortality rate associated with acute subdural hematoma is around 60 to 80% <ref>Dawodu S. 2004. [http://www.emedicine.com/pmr/topic212.htm "Traumatic brain injury: Definition, epidemiology, pathophysiology"] Emedicine.com. Retrieved on [[August 7]], [[2007]].</ref>
| | ==[[Subdural hematoma causes|Causes]]== |
|
| |
|
| Chronic subdural bleeds develop over the period of days to weeks, often after minor head trauma, though such a cause is not identifiable in 50% of patients.<ref name="Downie">Downie A. 2001. [http://www.radiology.co.uk/srs-x/tutors/cttrauma/tutor.htm "Tutorial: CT in head trauma"]. Retrieved on [[August 7]], [[2007]].</ref> They may not be discovered until they present clinically months or years after a head injury.<ref name="Kushner98">
| | ==[[Subdural hematoma differential diagnosis|Differentiating Subdural Hematoma from other Diseases]]== |
| {{
| |
| cite journal |author=Kushner D |title=Mild Traumatic Brain Injury: Toward Understanding Manifestations and Treatment |journal=Archives of Internal Medicine |volume=158 |issue=15 |pages=1617–1624 |year=1998 |pmid=9701095 |doi= |url=http://archinte.highwire.org/cgi/content/full/158/15/1617
| |
| }}
| |
| </ref> The bleeding from a chronic bleed is slow, probably from repeated minor bleeds, and usually stops by itself.<ref name="UVT"/><ref name="graham">Graham DI and Gennareli TA. Chapter 5, "Pathology of brain damage after head injury" Cooper P and Golfinos G. 2000. ''Head Injury'', 4th Ed. Morgan Hill, New York. </ref> Since these bleeds progress slowly, they present the chance to be stopped before they cause significant damage. Small subdural hematomas, those less than a centimeter wide, have much better outcomes than acute subdural bleeds: in one study, only 22% of patients with chronic subdural bleeds had outcomes worse than "good" or "complete recovery".<ref name="wagner"/> Chronic subdural hematomas are common in the elderly.<ref name="Kushner98"/>
| |
|
| |
|
| ==Pathophysiology== | | ==[[Subdural hematoma epidemiology and demographics|Epidemiology and Demographics]]== |
| Collected blood from the subdural bleed may draw in water due to [[osmosis]], causing it to expand, which may compress brain tissue and cause new bleeds by tearing other blood vessels.<ref name="Downie"/> The collected blood may even develop its own membrane.<ref>McCaffrey P. 2001. [http://www.csuchico.edu/~pmccaff/syllabi/SPPA336/336unit11.html "The neuroscience on the web series: CMSD 336 neuropathologies of language and cognition."] California State University, Chico. Retrieved on [[August 7]], [[2007]]. </ref>
| |
|
| |
|
| In some subdural bleeds, the [[arachnoid layer]] of the [[meninges]] is torn, and [[cerebrospinal fluid]] (CSF) and blood both expand in the [[intracranial space]], increasing pressure.<ref name="UVT"/>
| | ==[[Subdural hematoma risk factors|Risk Factors]]== |
|
| |
|
| Substances that cause vasoconstriction may be released from the collected material in a subdural hematoma, causing further [[ischemia]] under the site by restricting blood flow to the brain.<ref name="graham"/> When the brain is denied adequate blood flow, a [[biochemical cascade]] known as the [[ischemic cascade]] is unleashed, and may ultimately lead to brain [[cell (biology)|cell]] death.
| | ==[[Subdural hematoma natural history, complications and prognosis|Natural History, Complications and Prognosis]]== |
|
| |
|
| The body gradually reabsorbs the clot and replaces it with [[wound healing phases|granulation tissue]].
| | ==Diagnosis== |
| | [[Subdural hematoma history and symptoms|History and Symptoms]] | [[Subdural hematoma physical examination|Physical Examination]] | [[Subdural hematoma laboratory findings|Laboratory Findings]] | [[Subdural hematoma CT|CT]] | [[Subdural hematoma MRI|MRI]] | [[Subdural hematoma other imaging findings|Other Imaging Findings]] | [[Subdural hematoma other diagnostic studies|Other Diagnostic Studies]] |
|
| |
|
| ==Treatment== | | ==Treatment== |
| It is important that a patient receive medical assessment, including a complete [[neurology|neurological]] examination, after any head trauma. A [[CT scan]] or [[MRI scan]] will usually detect significant subdural hematomas.
| | [[Subdural hematoma medical therapy|Medical Therapy]] | [[Subdural hematoma surgery|Surgery]] | [[Subdural hematoma primary prevention|Primary Prevention]] | [[Subdural hematoma secondary prevention|Secondary Prevention]] | [[Subdural hematoma cost-effectiveness of therapy|Cost-Effectiveness of Therapy]] | [[Subdural hematoma future or investigational therapies|Future or Investigational Therapies]] |
|
| |
|
| Treatment of a subdural hematoma depends on its size and rate of growth. Small subdural hematomas can be managed by careful monitoring until the body heals itself. Large or symptomatic hematomas require a [[craniotomy]], the surgical opening of the [[skull]]. A surgeon then opens the [[dura]], removes the [[blood clot]] with suction or irrigation, and identifies and controls sites of [[bleeding]]. Postoperative complications include increased [[intracranial pressure]], brain [[edema]], new or recurrent [[bleeding]], [[infection]], and [[seizure]].
| | == Case Studies == |
| | [[Subdural hematoma case study one|Case #1]] |
|
| |
|
| ==Risk factors== | | ==Related Chapters== |
| Factors increasing the risk of a subdural hematoma include very young or very old [[senescence|age]]. As the brain shrinks with age, the [[subdural space]] enlarges and the [[vein]]s that traverse the space must travel over a wider distance, making them more vulnerable to tears. This and the fact that the elderly have more brittle veins make chronic subdural bleeds more common in older patients.<ref name="Downie"/> Infants, too, have larger subdural spaces and are more predisposed to subdural bleeds than are young adults.<ref name="wagner"/> For this reason, subdural hematoma is a common finding in [[shaken baby syndrome]]. In juveniles, an [[arachnoid cyst]] is a risk factor for a subdural hematoma.<ref>{{cite journal |author=Mori K, Yamamoto T, Horinaka N, Maeda M |title=Arachnoid cyst is a risk factor for chronic subdural hematoma in juveniles: twelve cases of chronic subdural hematoma associated with arachnoid cyst |journal=J. Neurotrauma |volume=19 |issue=9 |pages=1017–27 |year=2002 |pmid=12482115 |doi=10.1089/089771502760341938}}</ref>
| |
| | |
| Other risk factors for subdural bleeds include taking blood thinners ([[anticoagulant]]s), long-term [[alcoholism|alcohol abuse]], and [[dementia]].
| |
| | |
| ==See also==
| |
| * [[Head injury]] | | * [[Head injury]] |
| * [[Traumatic brain injury]] | | * [[Traumatic brain injury]] |
| Line 91: |
Line 45: |
| * [[Concussion]] | | * [[Concussion]] |
| * [[Diffuse axonal injury]] | | * [[Diffuse axonal injury]] |
|
| |
| ==References==
| |
| {{Reflist|2}}
| |
|
| |
|
| {{Cerebral hemorrhage}} | | {{Cerebral hemorrhage}} |
| {{Injuries, other than fractures, dislocations, sprains and strains}} | | {{Injuries, other than fractures, dislocations, sprains and strains}} |
| {{SIB}}
| |
|
| |
|
| [[Category:Neurotrauma]] | | |
| | [[Category:Disease]] |
| | [[Category:Neurosurgery]] |
| [[Category:Neurology]] | | [[Category:Neurology]] |
| [[Category:Emergency medicine]] | | [[Category:Emergency medicine]] |