|
|
| (3 intermediate revisions by the same user not shown) |
| Line 1: |
Line 1: |
| | |
| | |
|
| |
|
|
| |
|
| Line 5: |
Line 7: |
| ---- | | ---- |
|
| |
|
| '''Complication 1: Acute Kidney Injury in COVID-19'''<br><br>
| |
| '''For patient information, click [[Xyz (patient information)|here]]'''
| |
|
| |
|
| |
|
| |
| {{SK}} [[Acute Kidney Injury]], [[Acute Renal Failure]], [[AKI]], [[ARF]]
| |
|
| |
| ==[[AKI overview|Overview]]==
| |
|
| |
|
| |
|
| |
|
| |
| =[[AKI pathophysiology|Pathophysiology]]=
| |
|
| |
| *Angiotensin-converting enzyme 2 ([[ACE2]]), which is a primary receptor for [[SARS-CoV-2]] entry into cells, mostly presents in renal tubular epithelial cells as well as lungs and heart.<ref name="MalhaMueller2020">{{cite journal|last1=Malha|first1=Line|last2=Mueller|first2=Franco B.|last3=Pecker|first3=Mark S.|last4=Mann|first4=Samuel J.|last5=August|first5=Phyllis|last6=Feig|first6=Peter U.|title=COVID-19 and the Renin-Angiotensin System|journal=Kidney International Reports|volume=5|issue=5|year=2020|pages=563–565|issn=24680249|doi=10.1016/j.ekir.2020.03.024}}</ref>
| |
| *Despite kidney injury following [[COVID-19]] infection is less frequent than severe lung injury, [[ACE2]]: [[ACE]] ratio is higher in the kidneys compared to the respiratory system. (1:1 in the kidneys VS 1:20 in the respiratory system)<ref name="MalhaMueller2020">{{cite journal|last1=Malha|first1=Line|last2=Mueller|first2=Franco B.|last3=Pecker|first3=Mark S.|last4=Mann|first4=Samuel J.|last5=August|first5=Phyllis|last6=Feig|first6=Peter U.|title=COVID-19 and the Renin-Angiotensin System|journal=Kidney International Reports|volume=5|issue=5|year=2020|pages=563–565|issn=24680249|doi=10.1016/j.ekir.2020.03.024}}</ref>
| |
| * After [[SARS-CoV-2]] enters through the nasal cavity, it may travel to the kidneys and enters the bloodstream leading to severe inflammatory response activation and cytokine storm.
| |
| *It is thought that [[AKI]] following COVID-19 is the result of<ref name="MalhaMueller2020">{{cite journal|last1=Malha|first1=Line|last2=Mueller|first2=Franco B.|last3=Pecker|first3=Mark S.|last4=Mann|first4=Samuel J.|last5=August|first5=Phyllis|last6=Feig|first6=Peter U.|title=COVID-19 and the Renin-Angiotensin System|journal=Kidney International Reports|volume=5|issue=5|year=2020|pages=563–565|issn=24680249|doi=10.1016/j.ekir.2020.03.024}}</ref>
| |
| **[[Sepsis]]
| |
| **[[Hypovolemia]] and Hypotension
| |
| **Hypoxemia
| |
| **Blood clots formation, leading to impaired blood flow in the renal arterioles.
| |
| *[[AKI]] often occurs at later stages in critically ill patients with [[COVID-19]] following multiple organ failure.
| |
|
| |
|
| |
| [[File:AKI physiopathology COVID.PNG|600px|center]]
| |
|
| |
|
| |
|
| |
| =[[AKI epidemiology and demographics|Epidemiology and Demographics]]=
| |
| *Early reports from china revealed that COVID-19 rarely involves the kidneys, as [[Acute Renal Failure]] was not seen among COVID-19 hospitalized patients and mild [[BUN]] or creatinine rise [10.8%] and mild proteinuria [7.2%] occurred. <ref name="WangLi2020">{{cite journal|last1=Wang|first1=Luwen|last2=Li|first2=Xun|last3=Chen|first3=Hui|last4=Yan|first4=Shaonan|last5=Li|first5=Dong|last6=Li|first6=Yan|last7=Gong|first7=Zuojiong|title=Coronavirus Disease 19 Infection Does Not Result in Acute Kidney Injury: An Analysis of 116 Hospitalized Patients from Wuhan, China|journal=American Journal of Nephrology|volume=51|issue=5|year=2020|pages=343–348|issn=0250-8095|doi=10.1159/000507471}}</ref>
| |
| *However, recent study found 75.4% of hospitalized patients with COVID-19 pneumonia developed [[hematuria]], [[proteinuria]], and [[AKI]]. <ref name="PeiZhang2020">{{cite journal|last1=Pei|first1=Guangchang|last2=Zhang|first2=Zhiguo|last3=Peng|first3=Jing|last4=Liu|first4=Liu|last5=Zhang|first5=Chunxiu|last6=Yu|first6=Chong|last7=Ma|first7=Zufu|last8=Huang|first8=Yi|last9=Liu|first9=Wei|last10=Yao|first10=Ying|last11=Zeng|first11=Rui|last12=Xu|first12=Gang|title=Renal Involvement and Early Prognosis in Patients with COVID-19 Pneumonia|journal=Journal of the American Society of Nephrology|volume=31|issue=6|year=2020|pages=1157–1165|issn=1046-6673|doi=10.1681/ASN.2020030276}}</ref> But, these findings are not significantly different from other critical diseases.
| |
|
| |
|
| |
|
| |
|
| |
| =[[AKI Natural history|Natural history]]=
| |
| *Severe [[COVID-19]] pneumonia and [[severe acute respiratory distress syndrome]] are associated with developing [[AKI]].<ref name="PeiZhang2020">{{cite journal|last1=Pei|first1=Guangchang|last2=Zhang|first2=Zhiguo|last3=Peng|first3=Jing|last4=Liu|first4=Liu|last5=Zhang|first5=Chunxiu|last6=Yu|first6=Chong|last7=Ma|first7=Zufu|last8=Huang|first8=Yi|last9=Liu|first9=Wei|last10=Yao|first10=Ying|last11=Zeng|first11=Rui|last12=Xu|first12=Gang|title=Renal Involvement and Early Prognosis in Patients with COVID-19 Pneumonia|journal=Journal of the American Society of Nephrology|volume=31|issue=6|year=2020|pages=1157–1165|issn=1046-6673|doi=10.1681/ASN.2020030276}}</ref>
| |
| *Approximately half of the new AKI cases following COVID-19 is mild with good short-term prognosis.
| |
| *If no improvement occurs during follow-up, it is contributed to higher mortality.<ref name="PeiZhang2020">{{cite journal|last1=Pei|first1=Guangchang|last2=Zhang|first2=Zhiguo|last3=Peng|first3=Jing|last4=Liu|first4=Liu|last5=Zhang|first5=Chunxiu|last6=Yu|first6=Chong|last7=Ma|first7=Zufu|last8=Huang|first8=Yi|last9=Liu|first9=Wei|last10=Yao|first10=Ying|last11=Zeng|first11=Rui|last12=Xu|first12=Gang|title=Renal Involvement and Early Prognosis in Patients with COVID-19 Pneumonia|journal=Journal of the American Society of Nephrology|volume=31|issue=6|year=2020|pages=1157–1165|issn=1046-6673|doi=10.1681/ASN.2020030276}}</ref>
| |
|
| |
|
| =[[AKI History and Symptoms|History and Symptoms]]=
| |
|
| |
|
| *Patients in the early stages of kidney failure may be asymptomatic. If left untreated, patients may progress to develop [[Azotemia]] and [[Uremia]], which occur due to the buildup of waste materials in the blood.
| |
| '''History and Symptoms'''
| |
| *Symptoms of kidney injury include<ref name=Skorecki>{{cite book |vauthors=Skorecki K, Green J, Brenner BM |veditors=Kasper DL, Braunwald E, Fauci AS |title=Harrison's Principles of Internal Medicine|url=https://archive.org/details/harrisonsprincip00kasp |url-access=limited |edition=16th |year=2005 |publisher=McGraw-Hill |location=New York, NY |isbn=978-0-07-139140-5 |pages=[https://archive.org/details/harrisonsprincip00kasp/page/n1681 1653]–63 |chapter=Chronic renal failure|display-editors=etal}}</ref>:
| |
| **Nausea and Vomiting
| |
| **Weakness
| |
| **Fatigue
| |
| **Confusion
| |
| **Weight loss
| |
| **Loss of appetite
| |
| **[[Oliguria]] or [[Anuria]]
| |
| **Fluid retention, leading [[edema]] and swelling of face, extremities
| |
| **Electrolyte imbalance; High level of [[Potassium]] which leads to [[cardiac arrhythmia]]
| |
|
| |
|
| '''Physical Examination''' | | {{familytree/start}}{{familytree | | | | | | | | | A01 | | | | | |A01= [[COVID-19]] }} |
| | {{familytree | | |,|-|-|-|-|-|-|^|-|-|-|-|-|-|.| }} |
| | {{familytree | | C01 | | | | | | | | | | | | C02 |C01= '''30-40%''' <br> [[Asymptomatic]]|C02= '''60-70%''' <br> [[Symptomatic]]}} |
| | {{familytree | | |!| | | | | | | | | |,|-|-|-|+|-|-|-|-|.|}} |
| | {{familytree | | E01 | | | | | | | | E02 | | E03 | | | E04 |E01=[[Asymptomatic carrier]]|E02='''80%''' <br> Mild symtoms|E03='''14%''' <br> Severe symptoms|E04='''6%''' <br> Critically ill}} |
| | {{familytree | | | | | | | | | | | | |!| | | |!| | | | |!| | }} |
| | {{familytree | | | | | | | | | | | | F01 | | F02 | | | F03 |F01=[[Fever]]<br> [[Chills]]<br> [[Cough]]<br> [[Headache]]<br> [[Sore throat]]<br> [[Nasal congestion]] or secretion <br> [[Fatigue]]<br> [[Body aches]]<br> [[loss of taste]] or [[smell]] |
| | <br> [[Nausea]] or [[vomiting]] <br> [[Diarrhea]]<br> |F02=Severe [[Dyspnea]]<br> [[Chest pain]]<br> Severe [[weakness]] <br> new [[Confusion]]<br> Central [[Cyanosis]] |
| | |F03=Death}} |
| | {{familytree/end}} |
|
| |
|
| =[[AKI Diagnosis|Diagnosis]]=
| |
|
| |
|
| '''Laboratory Findings'''
| |
| *Laboratory findings consistent with the diagnosis of [[AKI]] include:
| |
| **Elevated [[BUN]] level
| |
| **Based on KDIGO definition for the diagnosis of AKI<ref name="pmid22890468">{{cite journal| author=Khwaja A| title=KDIGO clinical practice guidelines for acute kidney injury. | journal=Nephron Clin Pract | year= 2012 | volume= 120 | issue= 4 | pages= c179-84 | pmid=22890468 | doi=10.1159/000339789 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22890468 }} </ref>:
| |
| ***Elevated serum Creatinine by ≥0.3 mg/dl (≥26.5 μmol/l) within 48 hours; or
| |
| ***Elevated serum Creatinine to ≥1.5 times baseline within the previous 7 days; or
| |
| ***Urine volume < 0.5 ml/kg/h for >6 hours
| |
|
| |
|
| '''Electrocardiogram''' | | {| class="wikitable" |
| *There are no specific ECG findings associated with AKI. However, electrolyte disturbances such as hyperkalemia might lead to various ECG findings. | | ! colspan=4 style="background: #4479BA; color: #FFFFFF; " align="center"|CT manifestations of COVID-19 |
| | |- |
| | !style="background: #4479BA; color: #FFFFFF; " align="center" |CT findings |
| | !style="background: #4479BA; color: #FFFFFF; " align="center" |Definition |
| | !style="background: #4479BA; color: #FFFFFF; " align="center" |CT picture |
| | |- |
| | |style="background: #DCDCDC; |'''[[Ground glass opacity]]''' |
| | | |
| | *Hazy opacity in the lungs with well defined bronchial and vascular margins |
| | *the most common imaging finding |
| | *due to infection, chronic interstitial lung disease, and acute lung injury |
|
| |
|
| '''Ultrasound Finding''' | | |[[File:Covid-19-pneumonia-26.jpg|200px|thumb|center]] |
| | |- |
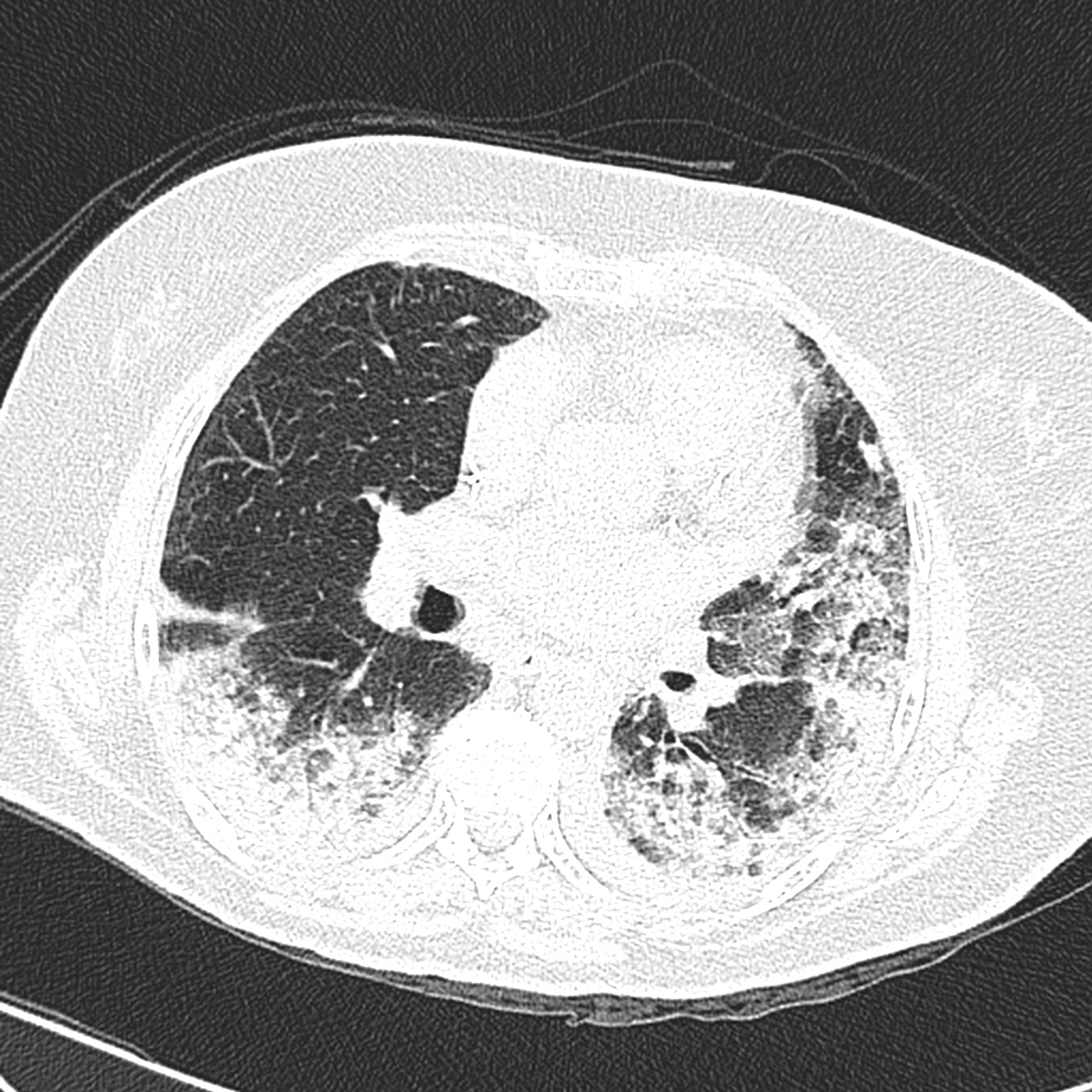
| | |style="background: #DCDCDC; |'''[[Consolidation]]''' |
| | | |
| | *a parenchymal density with ill-defined bronchial and vascular margins |
| | *filling with infectious material [fluid, cells, tissue] |
| | * due to cellular exudates in alveoli |
| | |[[file |
| | |- |
| | |style="background: #DCDCDC; |''' [[Crazy paving pattern]] ''' |
| | | |
| | * Septal thickening of inter and intra-lobar regions |
| | * with the background of the Ground glass opacity |
| | * Similar to paving stones |
| | * Due to alveolar edema and acute inflammation of the lung |
| | * Sign of progression |
| | |[[File:Covid-19-pneumonia-122.jpg|200px|thumb|center]] |
|
| |
|
| '''Other Diagnostic Studies'''
| |
|
| |
|
| =Treatment= | | |- |
| | |style="background: #DCDCDC; |''' [[Reticuldar]] pattern ''' |
| | | |
| | *Linear opacities in the lungs |
| | *Due to Interstitial thickening of inter and intralobular septa |
|
| |
|
| *Management of [[AKI]] following [[COVID-19]] includes treatment of infection, identifying electrolyte disorders, and [[intravenous fluid]] administration.
| | |[[file |
|
| |
|
| '''AKI Medical Therapy'''
| | |- |
| *Treatment of [[AKI]] following [[COVID-19]] includes<ref name="pmid32416769">{{cite journal| author=Ronco C, Reis T, Husain-Syed F| title=Management of acute kidney injury in patients with COVID-19. | journal=Lancet Respir Med | year= 2020 | volume= | issue= | pages= | pmid=32416769 | doi=10.1016/S2213-2600(20)30229-0 | pmc=7255232 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32416769 }} </ref>:
| | |style="background: #DCDCDC; |'''[[Air bronchogram]] ''' |
| **Correction of hypovolemia and hypotension by the administration of adequate [[intravenous fluid]]
| | | |
| **Correction of electrolyte disturbances
| | * Air-filled bronchi |
| **[[Renal Replacement Therapy]] | | *Low attenuated areas in the lung |
| ***If AKI is unresponsive to conservative therapy
| | |[[file |
| ***In volume overload conditions
| |
| ***Modality of choice in unstable hemodynamic status | |
| **Anticoagulants in hypercoagulable conditions
| |
| **Sequential extracorporeal therapy
| |
| ==References==
| |
| {{Reflist|2}}
| |
|
| |
|
| [[Category:Disease]] | | |- |
| [[Category:Emergency medicine]]
| | |style="background: #DCDCDC; |''' [[Bronchiectasis]] ''' |
| [[Category:Kidney diseases]] | | | |
| [[Category:Nephrology]]
| | *irreversible dilatation of the lung airways |
| | * Bronchus diameter more than 1.5 cm |
| | *due to inflammation, obstruction and impaired clearance |
| | |[[file |
| | |} |