ST elevation myocardial infarction aspirin therapy
| Cardiology Network |
 Discuss ST elevation myocardial infarction aspirin therapy further in the WikiDoc Cardiology Network |
| Adult Congenital |
|---|
| Biomarkers |
| Cardiac Rehabilitation |
| Congestive Heart Failure |
| CT Angiography |
| Echocardiography |
| Electrophysiology |
| Cardiology General |
| Genetics |
| Health Economics |
| Hypertension |
| Interventional Cardiology |
| MRI |
| Nuclear Cardiology |
| Peripheral Arterial Disease |
| Prevention |
| Public Policy |
| Pulmonary Embolism |
| Stable Angina |
| Valvular Heart Disease |
| Vascular Medicine |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [3] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Antiplatelet therapy with aspirin is a mainstay of pharmacotherapy in STEMI. In the International Study of Infarct Survival 2 (ISIS 2), aspirin reduced mortality in STEMI as much as streptokinase (by approximately 25%) when compared to the administration of neither agent. [1] Full doses of non-enteric coated aspirin should be administered as soon as possible to patients with STEMI if there are no contraindications (history of aspirin allergy or anaphylaxis to aspirin). Aspirin should be administered irrespective of the reperfusion strategy selected (either primary PCI or fibrinolytic administration).
Clinical trials supporting the administration of aspirin in STEMI
ISIS 2 was a landmark trial which randomized a total of 17,187 patients from 417 hospitals who presented within 24 hours (median 5 h) of STEMI symptom onset to one of 4 strategies:
- Streptokinase (1.5 million units) administered via the intravenous route over 1 hour or
- Aspirin (enteric coated at a dose of 160 mg/day) for one month or
- Both streptokinase and aspirin treatments or
- Neither treatemnt
Both streptokinase alone and aspirin alone were associated with a similar significant reduction in 5 week cardiovascular mortality:
- 9.2% (791/8592) incidence of cardiovascular deaths among streptokinase versus 12.0% (1029/8595) among placebo infusion patients (odds reduction: 25% +/- 4; p < 0.00001)
- 9.4% (804/8587) incidence of cardiovascular deaths among aspirin versus 11.8% (1016/8600) among placebo tablet patients (odds reduction: 23% +/- 4; p < 0.00001)
The combination of streptokinase and aspirin was associated with a significant reduction in cardiovascular mortality when compared to the administration of either agent alone (p < 0.0001). Furthermore, the effect of SK and ASA appeared to be additive as the mortality was only 8.0% (343/4292) among patients treated with both SK and ASA vs 13.2% (568/4300) among those treated with neither agent (42% +/- 5 relative risk reduction; 95% confidence limits 34% to 50%).
Streptokinase was associated with an increased risk of bleeding requiring transfusion (0.5% versus 0.2%) and intracranial hemmorhage (ICH) (0.1% versus 0.0%). Streptokinase was, however, assocaited with fewer non-ICH strokes (0.6% versus 0.8%).
Aspirin was associated with a significant reduction in nonfatal reinfarction (1.0% versus 2.0%) as well as nonfatal stroke (0.3% versus 0.6%). In contrast to streptokinase, aspirin was not associated with a significant increase in intracranial hemorrhage or bleeding requiring transfusion. Furthermore, while streptokinase alone was associated with an increased risk of reinfarction. The addition of aspirin to streptokinase eliminated of this increased risk of reinfarction associated with streptokinase administration.
History
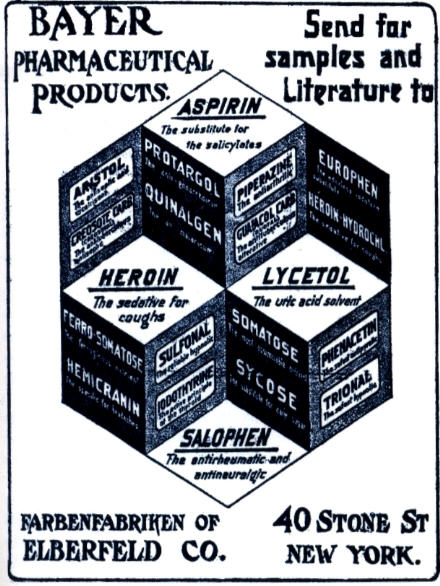
Medicines containing derivatives of salicylic acid, structurally similar to aspirin, have been in medical use since ancient times. Salicylate-rich willow bark extract became recognized for its specific effects on fever, pain and inflammation in the mid-eighteenth century. By the nineteenth century pharmacists were experimenting with and prescribing a variety of chemicals related to salicylic acid, the active component of willow extract.
A French chemist, Charles Frederic Gerhardt, was the first to prepare acetylsalicylic acid in 1853 (patented under the name aspirin on March 6, 1899 [2]). In the course of his work on the synthesis and properties of various acid anhydrides, he mixed acetyl chloride with a sodium salt of salicylic acid (sodium salicylate). A vigorous reaction ensued, and the resulting melt soon solidified.[3] Since no structural theory existed at that time, Gerhardt called the compound he obtained "salicylic-acetic anhydride" (wasserfreie Salicylsäure-Essigsäure). This preparation of aspirin ("salicylic-acetic anhydride") was one of the many reactions Gerhardt conducted for his paper on anhydrides, but he did not pursue it further.
Six years later, in 1859, von Gilm obtained analytically pure acetylsalicylic acid (which he called "acetylierte Salicylsäure", acetylated salicylic acid) by a reaction of salicylic acid and acetyl chloride.[4] In 1869 Schröder, Prinzhorn and Kraut repeated both Gerhardt's (from sodium salicylate) and von Gilm's (from salicylic acid) syntheses and concluded that both reactions gave the same compound—acetylsalicylic acid. They were first to assign to it the correct structure with the acetyl group connected to the phenolic oxygen.[5]
In 1897, scientists at the drug and dye firm Bayer began investigating acetylsalicylic acid as a less-irritating replacement for standard common salicylate medicines. By 1899, Bayer had dubbed this drug Aspirin and was selling it around the world.[6]The name Aspirin is derived from A = Acetyl and "Spirsäure" = an old (German) name for salicylic acid.[7] Aspirin's popularity grew over the first half of the twentieth century, spurred by its effectiveness in the wake of the Spanish flu pandemic of 1918, and aspirin's profitability led to fierce competition and the proliferation of aspirin brands and products, especially after the American patent held by Bayer expired in 1917.[8][9]
Aspirin's popularity declined after the market releases of paracetamol (acetaminophen) in 1956 and ibuprofen in 1969.[10] In the 1960s and 1970s, John Vane and others discovered the basic mechanism of aspirin's effects, while clinical trials and other studies from the 1960s to the 1980s established aspirin's efficacy as an anti-clotting agent that reduces the risk of clotting diseases.[11] Aspirin sales revived considerably in the last decades of the twentieth century, and remain strong in the twenty-first, thanks to widespread use as a preventive treatment for heart attacks and strokes.[12]
Trademark in most countries
As part of war reparations specified in the 1919 Treaty of Versailles following Germany's surrender after World War I, Aspirin (along with Heroin) lost its status as a registered trademark in France, Russia, the United Kingdom, and the United States, where it became a generic name and can be spelled in lower case.[13][14][15] Today, "aspirin" is a generic word in Australia, Argentina, Britain, France, India, Ireland, New Zealand, Pakistan, the Philippines, South Africa and the United States.[16] Aspirin remains a registered trademark of Bayer in Germany, Canada, Mexico, and in over 80 other countries, where the first letter of its name should be capitalized and used only in reference to and on ASA products manufactured and marketed by Bayer.[17][18]
Mechanism(s) of Benefit
Acetylation of platelet cyclooxygenase-1 (COX-1) begins to occur in the portal circulation prior to any measurable systemic level; thus, the measurement of plasma levels of the inactive form of acetylsalicylic acid may be an incomplete measure of efficacy. Nonetheless, peak plasma levels are achieved rapidly, within approximately 30 minutes, followed by rapid clearance with a half-life of 15-20 minutes. The systemic bioavailability of aspirin is about 50% for single oral doses ranging from 20-1300 mg.[19]
Both the beneficial and detrimental effects of aspirin are believed to be primarily due to inhibition of prostanoid biosynthesis, in particular the inhibition of of thromboxane A2 (TXA2) and prostaglandins (e.g., PGE2 and PGI2).
Aspirin irreversibly inhibits platelet cyclooxygenase 1 (COX-1) through acetylation of the amino acid serine at position 529, thereby preventing arachidonic acid's access to the COX-1 catalytic site through steric hindrance. By inhibiting COX-1, the platelet is unable to synthesize prostaglandin H2, which, under normal circumstances, is then converted to thromboxane A2 (TXA2) via the enzyme Thromboxane synthase. Although anucleate platelets possess some capacity for protein synthesis, they are incapable of overcoming COX-1 inhibition with new protein synthesis, and the aspirin-induced defect spans the 8 to 10 day life span of the platelet. Because of platelet turnover, approximately 10% of platelets with normal COX activity will be recovered daily following cessation of aspirin therapy. Therefore, up to 10 days can be required for complete recovery of platelet COX activity; however, it may require only 20% of normal COX activity to exhibit normal hemostasis.[20][21][22][23]
COX-1 is constitutively expressed in most cells and plays important roles beyond TXA2 production in platelets. Of particular importance is the production of the cytoprotective prostaglandins by gastric mucosa. Unlike platelets, gastric mucosal cells possess the biosynthetic machinery necessary to overcome COX-1 inhibition and, therefore, recover the ability to synthesize prostaglandins within a few hours after exposure to aspirin. COX-2, a second cyclo oxygenase isoenzyme primarily responsible for synthesis of the platelet inhibitor PGI2 by endothelial cells and induced in response to inflammatory stimuli, is less sensitive to the effects of aspirin. Aspirin is 170 fold less effective at inhibiting COX-2 than COX-1.
At higher doses, aspirin suppresses vascular endothelial cell production of prostacyclin, which, if unopposed, results in inhibition of platelet aggregation and induces vasodilatation.
It has been postulated that aspirin’s anti-inflammatory properties may explain at least part of its mechanism of benefit in CVD. However, with aspirin’s much greater selectivity for COX-1 and the central role of COX-2 in inflammation, dosages that achieve measurable anti-inflammatory activity (up to several grams daily) are much higher than those proven clinically effective in the prevention of atherothrombotic events. Consistent with this is the lack of an effect on high sensitivity C-reactive protein levels in most studies.
Currently, there is no gold standard measure of aspirin’s pharmacodynamics.
There has been only 1 randomized study that directly compared aspirin dose in STEMI. The Duke University Clinical Cardiology Group Study-II (DUCCS-II) compared the efficacy of 81 and 325 mg aspirin doses in 162 patients with STEMI treated with front loaded tissue plasminogen activator or an isolated plasminogen streptokinase activator complex. No effect of aspirin dose on clinical outcomes was noted; however, because of its early termination, the study was severely underpowered. The majority of data supporting the use of aspirin in the setting of acute myocardial infarction are from ISIS-2. In this study, 162.5 mg aspirin reduced vascular mortality, re-infarction, and stroke without substantially increasing the risk of major bleeding. Other studies of aspirin in the acute setting of myocardial infarction have been severely underpowered to address the clinical efficacy and safety profile of aspirin in this setting.
A wide range of aspirin doses, preparations, and methods of ingestion have been evaluated to determine the best way to achieve maximal antiplatelet activity in the acute setting. In a study that evaluated the acute antiplatelet effects of 40 mg, 100 mg, 300 mg, and 500 mg doses of aspirin, the 300 mg and 500 mg doses were found to achieve equal levels of platelet inhibition 2 hours following ingestion, suggesting that there is no added benefit for doses of more than 300 mg. However, at very low doses (0.45 mg/kg, corresponding to about 30 mg in an adult), it may take 10 days to effectively suppress TXA2 production. [24]
Aspirin absorption and the onset of antiplatelet activity are significantly shortened by chewing or drinking soluble aspirin, with maximal inhibition of serum Thromboxane B2 (TXB2) production achieved within 20 to 30 minutes compared with swallowing a whole pill that required approximately 60 minutes.
In another study of 18 volunteers, chewing an 81 mg, 162 mg, or 324 mg aspirin pill led to equivalent reduction in TXB2 production, but maximal inhibition by 15 minutes after ingestion was achieved only with the 162 mg and 324 mg doses. The results of these and other studies suggest that to rapidly (within 15 minutes) achieve the maximal effects of aspirin, at least 162 mg should be chewed or dissolved, then swallowed.[25][26]
The major risk of aspirin, as with other non steroidal anti inflammatory drugs (NSAIDs), is the risk of bleeding. Although the antiplatelet effects of aspirin likely contribute to an increase in the risk of bleeding, as highlighted by an increased risk of hemorrhagic stroke of 0.2 events per 1000 patient years, the majority of the increased bleeding has a gastrointestinal tract etiology.
Although this increased risk of gastrointestinal bleeding is more commonly attributed to non aspirin NSAIDs, a recent evaluation of patients hospitalized for ulcer bleeding found that low-dose aspirin therapy was responsible for as much ulcer bleeding as all other NSAIDs combined. In another prospective evaluation of 18 820 hospitalized patients, 1225 were admitted as a result of adverse drug reactions, and low-dose aspirin was identified as one of the most common causal agents, with 18% of the hospitalizations and 61% of the fatal cases associated with aspirin.[27][28][29][30]
An analysis of aspirin-treated patients from the UKTIA trial found almost double the risk of gastrointestinal bleeding among patients randomized to 1200 mg/day of aspirin compared with 300 mg/day. In the Dutch-TIA trial, where the higher aspirin dose was more reflective of contemporary dosing, a trend toward less bleeding was noted in the 30 mg group (2.6%) than the 283 mg group (3.2%).
Observational data from the BRAVO (Blockade of the Glycoprotein IIb/IIIa Receptor to Avoid Vascular Occlusion) and CURE (Clopidogrel in Unstable Angina to Prevent Recurrent Events) trials also demonstrated an increased risk of bleeding with higher doses of aspirin, even when doses no greater than 325 mg were used.[31][32]
Dosing
If not given prior to hospital admission, Aspirin should be administered to all patients at a dose of 162 to 325 mg to chew and swallow, unless there is a compelling contraindication (e.g., history of anaphylactic reaction). Aspirin is generally administered orally and is rapidly absorbed in the stomach and upper intestine. Enteric coating may delay the absorption, and it is for this reason that not enteric coated aspirin is often administered in the setting of ST elevation MI. It should also be noted that aspirin can also be administered via the intravenous route.[33]
Efficacy and safety of low dose (162 mg) aspirin versus high dose (325 mg) aspirin in STEMI patients
Large, prospective, randomized trials randomizing STEMI patients to either low vs high doses of aspirin in STEMI are lacking. The 30 day mortality and bleeding risks associated with the administration of 162 mg versus 325 mg aspirin among patients with STEMI treated with thrombolytic therapy has been compared in a non-randomized retrospective analysis. [34][35] Data for the analysis was drawn from a total of 48,422 patients with acute ST segment elevation myocardial infarction in the GUSTO I and GUSTO III trials (Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries). 24.4% of patients (n=11 828) were treated in a non-randomized fashio with an initial aspirin dose of 325 mg, and 75.6% (n=36 594) were treated with 162 mg. 24-hour mortality did not differ between the two doses: 2.9% for those receiving an initial aspirin dose of 325 mg versus 2.8% (P=0.894) for those receiving an initial aspirin dose 162 mg. 7 and 30 day mortality rates were 5.2% versus 4.9% (P=0.118) and 7.1% versus 6.5% (P=0.017) among patients receiving the 325 versus 162 mg aspirin respectively. After multivariate adjustment for imbalances in baseline characteristics, the initial aspirin dose was not associated with 24-hour (odds ratio [OR], 1.01; 95% CI, 0.82 to 1.25), 7-day (OR, 1.00; 95% CI, 0.87 to 1.17), or 30-day (OR, 0.99; 95% CI, 0.87 to 1.12) mortality rates. No significant difference was noted for reinfarction or the composite of death or reinfarction between the two aspirin dose groups. In-hospital moderate/severe bleeding occurred in 9.3% of those treated with 325 mg versus 12.2% among those receiving 162 mg (P<0.001). However, after adjustment for imbalances in baseline characteristics, an initial dose of 325 mg was associated with a significant increase in moderate/severe bleeding (OR, 1.14; 95% CI, 1.05 to 1.24; P=0.003) compared to an initial does of 162 mg.
This non-randomized data from trials conducted many years ago with a substantial use of streptokinase demonstrates that the initial dose of 162 mg aspirin may be as effective as and perhaps safer than 325 mg for the acute treatment of ST elevation myocardial infarction. These findings require confirmation in large randomized trials before a firm recommendation can be made regarding the optimal initial dose of aspirin in STEMI patients.
Side Effects and Contraindications
The use of aspirin is contraindicated in those with a hypersensitivity to salicylate.
Aspirin suppositories (300 mg) can be used safely and are the recommended route of administration for patients with severe nausea and vomiting or known upper-gastrointestinal disorders.
In patients with true aspirin allergy (hives, nasal polyps, bronchospasm, or anaphylaxis), clopidogrel or ticlopidine may be substituted.[36]
Guidelines (DO NOT EDIT)
Class I
- For all post Percutaneous Coronary Interventions (PCI) stented STEMI patients without aspirin resistance, allergy, or increased risk of bleeding, aspirin 162 mg to 325 mg daily should be given for at least 1 month after bare metal stent (BMS) implantation, 3 months after Sirolimus eluting stent implantation (SES), and 6 months after Paclitaxel eluting stent implantation (PES), after which long term aspirin use should be continued indefinitely at a dose of 75 mg to 162 mg daily. Class I (Level of Evidence: B)[37]
Class IIa
- In patients for whom the physician is concerned about risk of bleeding lower-dose 75 mg to 162 mg of aspirin is reasonable during the initial period after stent implantation. Class IIa (Level of Evidence: C)[37]
References
- ↑ "Randomized trial of intravenous streptokinase, oral aspirin, both, or neither among 17,187 cases of suspected acute myocardial infarction: ISIS-2.ISIS-2 (Second International Study of Infarct Survival) Collaborative Group". J. Am. Coll. Cardiol. 12 (6 Suppl A): 3A–13A. 1988. PMID 2903874. Unknown parameter
|month=ignored (help) - ↑ "1899". Wonders of Aspirin. BAYER. Retrieved March 3, 2009.
- ↑ Template:De icon Gerhardt C (1853). "Untersuchungen über die wasserfreien organischen Säuren". Annalen der Chemie und Pharmacie. 87: 149–179. doi:10.1002/jlac.18530870107.
- ↑ Template:De icon von Gilm H (1859). "Acetylderivate der Phloretin- und Salicylsäure". Annalen der Chemie und Pharmacie. 112 (2): 180–185. doi:10.1002/jlac.18591120207.
- ↑ Template:De icon Schröder, Prinzhorn, Kraut K (1869). "Uber Salicylverbindungen". Annalen der Chemie und Pharmacie. 150 (1): 1–20. doi:10.1002/jlac.18691500102.
- ↑ Jeffreys, Diarmuid (August 11, 2005). Aspirin: The Remarkable Story of a Wonder Drug. Bloomsbury USA. p. 73. ISBN 1582346003.
- ↑ Ueber Aspirin. Pflügers Archiv : European journal of physiology, Volume: 84, Issue: 11-12 (March 1, 1901), pp: 527-546.
- ↑ Jeffreys, Aspirin, pp. 136–142 and 151-152
- ↑ http://www.history.com/this-day-in-history.do?action=VideoArticle&id=52415
- ↑ Jeffreys, Aspirin, pp. 212–217
- ↑ Jeffreys, Aspirin, pp. 226–231
- ↑ Jeffreys, Aspirin, pp. 267–269
- ↑ "Treaty of Versailles, Part X, Section IV, Article 298". 1919-06-28. pp. Annex, Paragraph 5. Retrieved 2008-10-25.
- ↑ Mehta, Aalok (2005-06-20). "Aspirin". Chemical & Engineering News. 83 (25). Retrieved 2008-10-23.
- ↑ http://www.ul.ie/~childsp/CinA/Issue59/TOC43_Aspirin.htm
- ↑ CBE Style Manual Committee; Huth, Edward J. (1994). Scientific Style and Format: The CBE Manual for Authors, Editors, and Publishers. Cambridge University Press. p. 164.
- ↑ http://www.aspirin.com/faq_en.html
- ↑
Cheng, Tsung O. (2007). "The History of Aspirin". Texas Heart Institute Journal. 34 (3): 392–393. PMID 17948100. Retrieved 2008-10-23. Unknown parameter
|day=ignored (help); Unknown parameter|month=ignored (help) - ↑ Campbell CL, Smyth S, Montalescot G, Steinhubl SR (2007). "Aspirin dose for the prevention of cardiovascular disease: a systematic review". JAMA. 297 (18): 2018–24. doi:10.1001/jama.297.18.2018. PMID 17488967. Unknown parameter
|month=ignored (help) - ↑ Roux S, Christeller S, Lüdin E (1992). "Effects of aspirin on coronary reocclusion and recurrent ischemia after thrombolysis: a meta-analysis". J. Am. Coll. Cardiol. 19 (3): 671–7. PMID 1531663. Unknown parameter
|month=ignored (help) - ↑ "Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients". BMJ. 324 (7329): 71–86. 2002. PMC 64503. PMID 11786451. Unknown parameter
|month=ignored (help) - ↑ Sagar KA, Smyth MR (1999). "A comparative bioavailability study of different aspirin formulations using on-line multidimensional chromatography". J Pharm Biomed Anal. 21 (2): 383–92. PMID 10703994. Unknown parameter
|month=ignored (help) - ↑ Sabatine MS, Cannon CP, Gibson CM; et al. (2005). "Addition of clopidogrel to aspirin and fibrinolytic therapy for myocardial infarction with ST-segment elevation". N. Engl. J. Med. 352 (12): 1179–89. doi:10.1056/NEJMoa050522. PMID 15758000. Unknown parameter
|month=ignored (help) - ↑ Patrignani P, Filabozzi P, Patrono C (1982). "Selective cumulative inhibition of platelet thromboxane production by low-dose aspirin in healthy subjects". J. Clin. Invest. 69 (6): 1366–72. PMC 370209. PMID 7045161. Unknown parameter
|month=ignored (help) - ↑ Dabaghi SF, Kamat SG, Payne J; et al. (1994). "Effects of low-dose aspirin on in vitro platelet aggregation in the early minutes after ingestion in normal subjects". Am. J. Cardiol. 74 (7): 720–3. PMID 7942533. Unknown parameter
|month=ignored (help) - ↑ Feldman M, Cryer B (1999). "Aspirin absorption rates and platelet inhibition times with 325-mg buffered aspirin tablets (chewed or swallowed intact) and with buffered aspirin solution". Am. J. Cardiol. 84 (4): 404–9. PMID 10468077. Unknown parameter
|month=ignored (help) - ↑ Hovens MM, Snoep JD, Eikenboom JC, van der Bom JG, Mertens BJ, Huisman MV (2007). "Prevalence of persistent platelet reactivity despite use of aspirin: a systematic review". Am. Heart J. 153 (2): 175–81. doi:10.1016/j.ahj.2006.10.040. PMID 17239674. Unknown parameter
|month=ignored (help) - ↑ Jochmann N, Stangl K, Garbe E, Baumann G, Stangl V (2005). "Female-specific aspects in the pharmacotherapy of chronic cardiovascular diseases". Eur. Heart J. 26 (16): 1585–95. doi:10.1093/eurheartj/ehi397. PMID 15996977. Unknown parameter
|month=ignored (help) - ↑ Becker DM, Segal J, Vaidya D; et al. (2006). "Sex differences in platelet reactivity and response to low-dose aspirin therapy". JAMA. 295 (12): 1420–7. doi:10.1001/jama.295.12.1420. PMID 16551714. Unknown parameter
|month=ignored (help) - ↑ Berger JS, Roncaglioni MC, Avanzini F, Pangrazzi I, Tognoni G, Brown DL (2006). "Aspirin for the primary prevention of cardiovascular events in women and men: a sex-specific meta-analysis of randomized controlled trials". JAMA. 295 (3): 306–13. doi:10.1001/jama.295.3.306. PMID 16418466. Unknown parameter
|month=ignored (help) - ↑ Topol EJ, Easton D, Harrington RA; et al. (2003). "Randomized, double-blind, placebo-controlled, international trial of the oral IIb/IIIa antagonist lotrafiban in coronary and cerebrovascular disease". Circulation. 108 (4): 399–406. doi:10.1161/01.CIR.0000084501.48570.F6. PMID 12874182. Unknown parameter
|month=ignored (help) - ↑ Quinn MJ, Aronow HD, Califf RM; et al. (2004). "Aspirin dose and six-month outcome after an acute coronary syndrome". J. Am. Coll. Cardiol. 43 (6): 972–8. doi:10.1016/j.jacc.2003.09.059. PMID 15028352. Unknown parameter
|month=ignored (help) - ↑ Berger JS, Stebbins A, Granger CB; et al. (2008). "Initial aspirin dose and outcome among ST-elevation myocardial infarction patients treated with fibrinolytic therapy". Circulation. 117 (2): 192–9. doi:10.1161/CIRCULATIONAHA.107.729558. PMID 18086929. Unknown parameter
|month=ignored (help) - ↑ Alberts MJ, Bergman DL, Molner E, Jovanovic BD, Ushiwata I, Teruya J (2004). "Antiplatelet effect of aspirin in patients with cerebrovascular disease". Stroke. 35 (1): 175–8. doi:10.1161/01.STR.0000106763.46123.F6. PMID 14671242. Unknown parameter
|month=ignored (help) - ↑ Serebruany VL, Steinhubl SR, Berger PB; et al. (2005). "Analysis of risk of bleeding complications after different doses of aspirin in 192,036 patients enrolled in 31 randomized controlled trials". Am. J. Cardiol. 95 (10): 1218–22. doi:10.1016/j.amjcard.2005.01.049. PMID 15877994. Unknown parameter
|month=ignored (help) - ↑ Pirmohamed M, James S, Meakin S; et al. (2004). "Adverse drug reactions as cause of admission to hospital: prospective analysis of 18 820 patients". BMJ. 329 (7456): 15–9. doi:10.1136/bmj.329.7456.15. PMC 443443. PMID 15231615. Unknown parameter
|month=ignored (help) - ↑ 37.0 37.1 Antman EM, Hand M, Armstrong PW; et al. (2008). "2007 Focused Update of the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: developed in collaboration With the Canadian Cardiovascular Society endorsed by the American Academy of Family Physicians: 2007 Writing Group to Review New Evidence and Update the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction, Writing on Behalf of the 2004 Writing Committee". Circulation. 117 (2): 296–329. doi:10.1161/CIRCULATIONAHA.107.188209. PMID 18071078. Unknown parameter
|month=ignored (help)