Riedel's thyroiditis pathophysiology
|
Riedel's thyroiditis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Riedel's thyroiditis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Riedel's thyroiditis pathophysiology |
|
Risk calculators and risk factors for Riedel's thyroiditis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Furqan M M. M.B.B.S[2]
Overview
The exact pathogenesis of Riedel's thyroiditis is not fully understood. The presence of thyroid autoantibodies and lymphoid infiltration of the thyroid gland resembling that of Hashimoto's thyroiditis might indicate an autoimmune etiology. It is considered that the infiltrating lymphocytes release cytokines which are responsible for the activation of fibroblasts responsible for the fibrosis. Riedel's thyroiditis is characterized by a replacement of the normal thyroid parenchyma by a dense fibrosis that invades adjacent structures of the neck and extends beyond the thyroid capsule. This makes the thyroid gland stone-hard and fixed to adjacent structures. A shared mechanism with retroperitoneal fibrosis and sclerosing cholangitis has been suggested.
Pathophysiology
Pathophysiology
The exact pathophysiology of Riedel's thyroiditis is not fully understood. The presence of thyroid autoantibodies and lymphoid infiltration of the thyroid gland resembling that of Hashimoto's thyroiditis might indicate an autoimmune etiology.[1]
- It is considered that the infiltrating lymphocytes (CD4+ and CD8+) release cytokines which are responsible for the activation of fibroblasts responsible for the fibrosis.[2]
- Riedel's thyroiditis is characterized by a replacement of the normal thyroid parenchyma by a dense fibrosis that invades adjacent structures of the neck and extends beyond the thyroid capsule.This makes the thyroid gland stone-hard and fixed to adjacent structures.[3]
- Tissue eosinophilia and Major basic protein (MBP) identified in the thyroid gland on the histopathological analysis are also thought to play a role in the proliferation of fibroblasts.[4]
- A shared mechanism with retroperitoneal fibrosis and sclerosing cholangitis is also suggested.[5]
Pathogenesis
The following hypotheses regarding the pathogenesis of Riedel's thyroiditis have been proposed:[6]
The Systemic Autoimmune Hypothesis
Based on this theory, it is accepted that RT might be a primary disease of fibroblasts and, therefore, might represent just one manifestation of a systemic fibrosclerotic process triggered by autoimmune stimuli. The cascade of events leading to fibrosis remains unknown.The “trigger” event could be an allergic hypersensitivity reaction caused by the leakage of oxidized low-density lipoprotein from atheromatous plaques, following an injury of endothelial cells. The natural consequence of this hypothesis is that the antigen initiating fibrosis is not localized within the thyroid, and the disease process does not originate within the thyroid. On the contrary, the thyroid gland is affected secondarily by a systemic fibroinflammatory process, probably because follicular cells, perithyroid muscular cells, or intrathyroidal endothelial cells express antigens, cytokines, or adhesion molecules that contribute to local activation of the disease. The evidence of a perivascular concentration of inflammatory cells in RT (occlusive phlebitis) might support the theory that the allergic process first involves blood vessels.
The Genetic Hypothesis
This hypothesis was also proposed for the multifocal fibrosclerosis. The basis of this hypothesis was a report of multifocal fibrosclerotic disease in two brothers, whose parents were first cousins. They developed different combinations of the multifocal fibrosclerotic disease and a familial multifocal fibrosclerosis was hypothesized. It was thought that genetic factors might have played a partial role in an enzymatic defect in the tryptophan → serotonin → 5-hydroxyindolacetic acid pathway. However, such a relationship has never been proven, and the siblings described remain the only case of familial multifocal fibrosclerosis reported in the literature.[7]
The Intrathyroidal hypothesis
Riedel's thyroiditis is associated with Hashimoto's thyroiditis, subacute thyroiditis, and de Quervain's thyroiditis. It is proposed that Riedel's thyroiditis might represent a late fibrotic stage of subacute or chronic thyroiditis. The fundamental concept of this theory is that the fibrosing process of RT is specific to the thyroid gland.[8]
The Pharmacologic Hypothesis
The production of fibrosis by the drugs might be determined by an increased serum serotonin concentration through competitive inhibition at the serotonin receptor level and a reaction of hypersensitivity causing vasculitis, plasmatic exudation resulting in fibrosis. Although drugs have been found to cause multi organ fibrosis, there are no reports of the association of Riedel's thyroiditis caused by drugs. As Riedel's thyroiditis is associated with multi organ fibrosis this theory might explain the indirect association of Riedel's thyroiditis with drugs.[6][9]
Associated Conditions
Riedel's thyroiditis is associated various other autoimmune conditions including:[2][10][11][12][13][9]
- Graves’ disease
- Hashimoto’s thyroiditis
- Multifocal idiopathic fibrosclerosis
- Addison’s disease
- Pernicious anemia
- Type 1 diabetes
Gross Pathology
- On gross pathology, dense, avascular white fibrous tissue, the absence of a capsule, and no normal thyroid tissue are characteristic findings of Riedel's thyroiditis.[14]
Microscopic Pathology
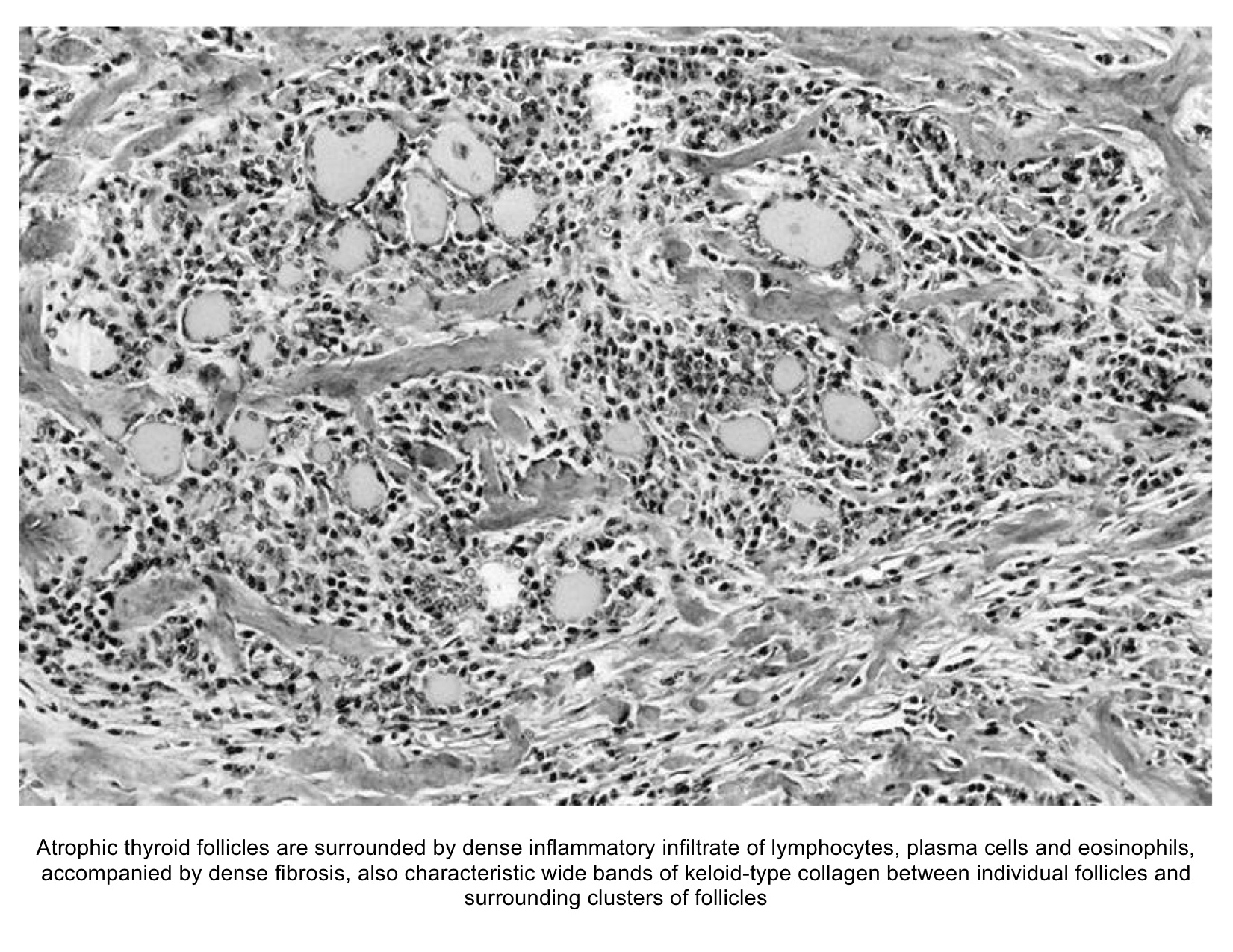
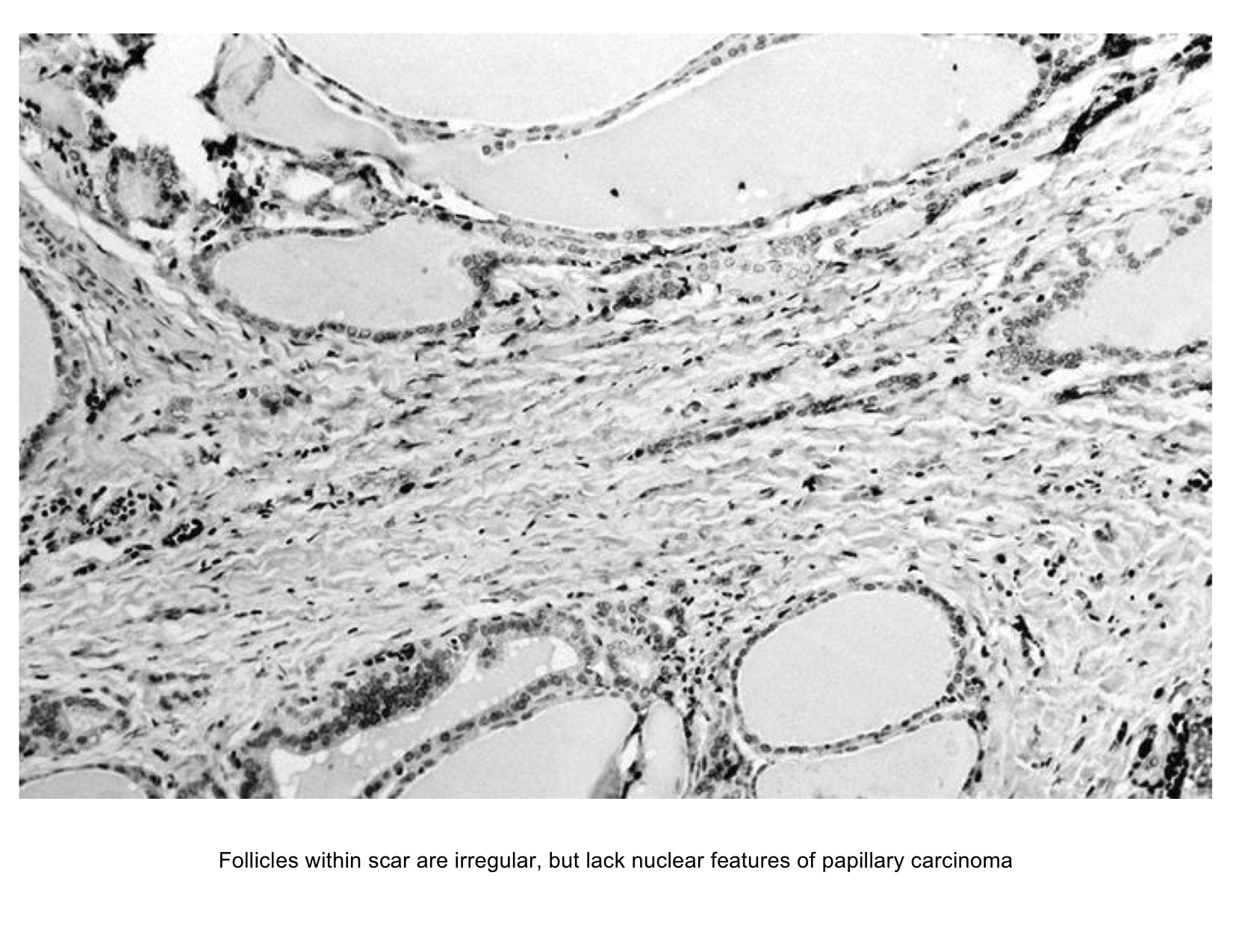
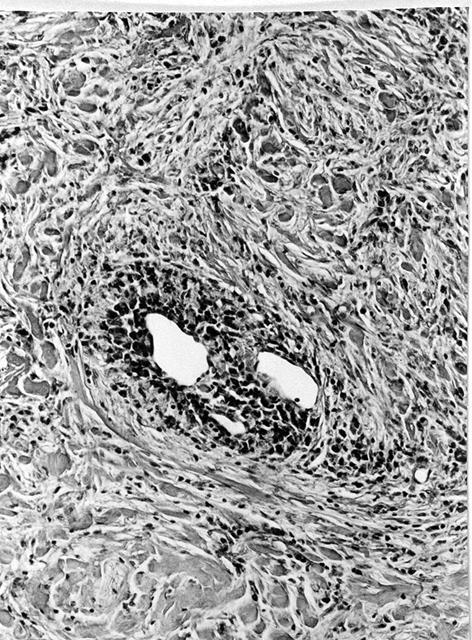
- On microscopic histopathological analysis, destruction of thyroid follicle by inflammatory cells and fibrous tissues and invasion of surrounding structures are characteristic findings of Riedel's thyroiditis.The inflammatory cells including lymphocytes, plasma cells, and eosinophils are present in a dense matrix of hyalinized connective tissue.[15][6]
Gallery
-
Histology of Riedel's thyroiditis (Image courtesy of AFIP and PathologyOutlines.com; http://www.pathologyoutlines.com/topic/thyroidriedel.html )
-
Histology of Riedel's thyroiditis (Image courtesy of AFIP and PathologyOutlines.com; http://www.pathologyoutlines.com/topic/thyroidriedel.html )
-
Histology of Riedel's thyroiditis (Image courtesy of AFIP and PathologyOutlines.com; http://www.pathologyoutlines.com/topic/thyroidriedel.html )
References
- ↑ Schwaegerle SM, Bauer TW, Esselstyn CB (1988). "Riedel's thyroiditis". Am. J. Clin. Pathol. 90 (6): 715–22. PMID 3057862.
- ↑ 2.0 2.1 Zimmermann-Belsing T, Feldt-Rasmussen U (1994). "Riedel's thyroiditis: an autoimmune or primary fibrotic disease?". J. Intern. Med. 235 (3): 271–4. PMID 8120524.
- ↑ Cho MH, Kim CS, Park JS; et al. (2007). "Riedel's thyroiditis in a patient with recurrent subacute thyroiditis: a case report and review of the literature". Endocr. J. 54 (4): 559–62. PMID 17603227.
- ↑ "Tissue eosinophilia and eosinophil degranulation in Riedel's invasive fibrous thyroiditis | The Journal of Clinical Endocrinology & Metabolism | Oxford Academic".
- ↑ De Boer WA (1993). "Riedel's thyroiditis, retroperitoneal fibrosis, and sclerosing cholangitis: diseases with one pathogenesis?". Gut. 34 (5): 714. PMC 1374200. PMID 8504980.
- ↑ 6.0 6.1 6.2 Papi G, LiVolsi VA (2004). "Current concepts on Riedel thyroiditis". Am. J. Clin. Pathol. 121 Suppl: S50–63. PMID 15298150.
- ↑ Comings DE, Skubi KB, Van Eyes J, Motulsky AG (1967). "Familial multifocal fibrosclerosis. Findings suggesting that retroperitoneal fibrosis, mediastinal fibrosis, sclerosing cholangitis, Riedel's thyroiditis, and pseudotumor of the orbit may be different manifestations of a single disease". Ann. Intern. Med. 66 (5): 884–92. PMID 6025229.
- ↑ Ewing J (1919). Neoplastic Diseases 2nd edition. Saunders; 1922:908.
- ↑ 9.0 9.1 Drieskens O, Blockmans D, Van den Bruel A, Mortelmans L (2002). "Riedel's thyroiditis and retroperitoneal fibrosis in multifocal fibrosclerosis: positron emission tomographic findings". Clin Nucl Med. 27 (6): 413–5. PMID 12045432.
- ↑ Drury MI, Sweeney EC, Heffernan SJ (1974). "Invasive fibrous (Riedel's) thyroiditis". Ir Med J. 67 (14): 388–90. PMID 4413980.
- ↑ "Chronic thyroiditis: A case showing features of both riedel's and hashimoto's thyroiditis - Merrington - 1948 - British Journal of Surgery - Wiley Online Library".
- ↑ Hines RC, Scheuermann HA, Royster HP (1970). "Invasive Fibrous (Riedel's) Thyroiditis With Bilateral Fibrous Parotitis". JAMA: 869–871. doi:10.1001/jama.1970.03170310147054.
- ↑ "Riedel's Thyroiditis: A Clinical Review | The Journal of Clinical Endocrinology & Metabolism | Oxford Academic".
- ↑ "Riedel's Thyroiditis | American Journal of Clinical Pathology | Oxford Academic".
- ↑ "Redirecting".