Prolactinoma surgery: Difference between revisions
Jump to navigation
Jump to search
No edit summary |
m (Bot: Removing from Primary care) |
||
| (47 intermediate revisions by 8 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Prolactinoma}} | {{Prolactinoma}} | ||
{{CMG}} | {{CMG}}; {{AE}} {{Faizan}}, {{Anmol}} | ||
==Overview== | |||
Surgery is not the first-line treatment option for patients with [[prolactinoma]]. [[Surgery]] is usually reserved for patients in whom medical therapy fails to reduce the size of the [[tumor]]. | |||
==Surgery== | |||
== | === Indications === | ||
Medical therapy should be continued even if it is partially successful, possibly combined with surgery or [[radiation]]. Surgery is indicated in patients if medical therapy:<ref name="urlProlactinoma | NIDDK">{{cite web |url=https://www.niddk.nih.gov/health-information/endocrine-diseases/prolactinoma |title=Prolactinoma | NIDDK |format= |work= |accessdate=}}</ref><ref name="pmid21423245">{{cite journal| author=Colao A, Savastano S| title=Medical treatment of prolactinomas. | journal=Nat Rev Endocrinol | year= 2011 | volume= 7 | issue= 5 | pages= 267-78 | pmid=21423245 | doi=10.1038/nrendo.2011.37 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21423245 }} </ref><ref name="pmid11761431">{{cite journal| author=Nomikos P, Buchfelder M, Fahlbusch R| title=Current management of prolactinomas. | journal=J Neurooncol | year= 2001 | volume= 54 | issue= 2 | pages= 139-50 | pmid=11761431 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11761431 }} </ref> | |||
*Cannot be tolerated | |||
*Fails to reduce [[ prolactin]] concentration | |||
*Fails to restore normal [[reproductive]] and [[pituitary]] function | |||
*Fails to reduce [[tumor]] size | |||
== | ===Transsphenoidal resection=== | ||
{| align="right" | |||
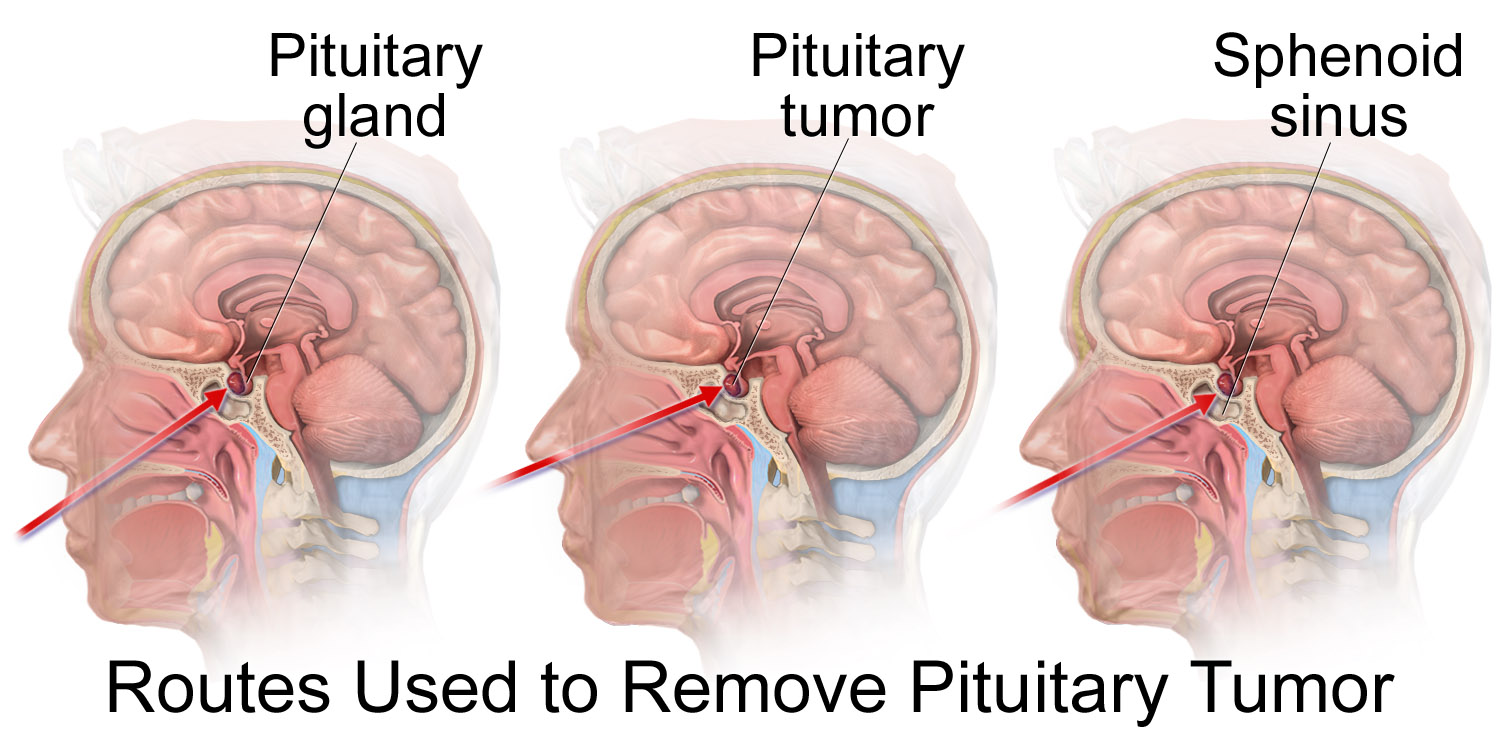
| [[image:Pituitary Tumor Removal.png|thumb|500px|Transsphenoidal approach to pituitary tumor - Source: Wikimedia.org<ref name=Delayed puberty "{{commons.wikimedia.org/wiki/User:BruceBlaus" title="User:BruceBlaus">BruceBlaus-Own work, <"https://commons.wikimedia.org/w/index.php?curid=61131794"></ref>]] | |||
|-| | |||
| {{#ev:youtube|_fioC34LZeg|500}} | |||
|} | |||
==== Endoscopic transsphenoidal surgery<ref name="pmid24533411">{{cite journal| author=Fan YP, Lv MH, Feng SY, Fan X, Hong HY, Wen WP et al.| title=Full Endoscopic Transsphenoidal Surgery for Pituitary Adenoma-emphasized on Surgical Skill of Otolaryngologist. | journal=Indian J Otolaryngol Head Neck Surg | year= 2014 | volume= 66 | issue= Suppl 1 | pages= 334-40 | pmid=24533411 | doi=10.1007/s12070-011-0317-4 | pmc=3918297 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24533411 }}</ref> ==== | |||
* In this method, the [[pituitary tumor]] is excised through [[nostrils]] by means of a tiny fiber-optic [[endoscopic]] tube. | |||
* First, bilateral [[nasal]] septal [[mucosa]] is incised in a C-shaped manner. The septal [[bone]] is approached through this incision. | |||
* Then, [[sphenoidal]] rostrum and anterior wall of [[sphenoid sinus]] are gradually removed, a [[bone]] window is opened through the [[skull]] space. | |||
* After that, the [[dura mater]] is passed and the lesion becomes visible. | |||
* Finally, the [[tumor]] is removed using [[curette]] and basket with suction. | |||
* '''Advantages:''' | |||
** No harm to other parts of the [[brain]] | |||
** High cure rate | |||
** No visible [[scar]] | |||
* '''Disadvantages''': | |||
** Not for large [[tumors]] | |||
** Recurrent [[sinusitis]] in the future | |||
** Low cure rate in case of [[suprasellar]] adhesion to adjunct tissues | |||
==== Craniotomy<ref name="pmid15987585">{{cite journal |vauthors=Youssef AS, Agazzi S, van Loveren HR |title=Transcranial surgery for pituitary adenomas |journal=Neurosurgery |volume=57 |issue=1 Suppl |pages=168–75; discussion 168–75 |year=2005 |pmid=15987585 |doi= |url=}}</ref> ==== | |||
* Although the preferred procedure to excise the [[pituitary tumors]] is a trans-sphenoidal approach, but in some cases (1-4%) the size of the tumor or any [[suprasellar]] adhesion may require trans-cranial method. | |||
* Situations requiring transcranial method include: | |||
** Isolation by a narrow waist at the [[diaphragma sellae]] | |||
** Containment within the [[cavernous sinus]] lateral to the [[carotid artery]] | |||
** Projection anteriorly onto the planum sphenoidal | |||
** Projection laterally into the middle fossa | |||
* [[Skull]] base surgical procedure is also the option for [[pituitary tumor]] treatment but may encounter the problems that transsphenoidal method is faced with. | |||
* '''Advantages:''' | |||
** Resection of large [[tumors]] | |||
** Ability to excise the tumors with [[suprasellar]] specific conditions | |||
* '''Disadvantages:''' | |||
** Long duration of post-operation recovery | |||
** Damage to other parts of the [[brain]] | |||
== References == | == References == | ||
| Line 19: | Line 56: | ||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
| |||
[[Category:Disease]] | [[Category:Disease]] | ||
[[Category:Neuroendocrinology]] | [[Category:Neuroendocrinology]] | ||
[[Category: | [[Category:Oncology]] | ||
[[Category: | [[Category:Medicine]] | ||
[[Category:Endocrinology]] | |||
[[Category:Up-To-Date]] | |||
[[Category:Neurology]] | |||
[[Category:Neurosurgery]] | |||
Latest revision as of 23:50, 29 July 2020
|
Prolactinoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Prolactinoma surgery On the Web |
|
American Roentgen Ray Society Images of Prolactinoma surgery |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Faizan Sheraz, M.D. [2], Anmol Pitliya, M.B.B.S. M.D.[3]
Overview
Surgery is not the first-line treatment option for patients with prolactinoma. Surgery is usually reserved for patients in whom medical therapy fails to reduce the size of the tumor.
Surgery
Indications
Medical therapy should be continued even if it is partially successful, possibly combined with surgery or radiation. Surgery is indicated in patients if medical therapy:[1][2][3]
- Cannot be tolerated
- Fails to reduce prolactin concentration
- Fails to restore normal reproductive and pituitary function
- Fails to reduce tumor size
Transsphenoidal resection
 |
| _fioC34LZeg|500}} |
Endoscopic transsphenoidal surgery[4]
- In this method, the pituitary tumor is excised through nostrils by means of a tiny fiber-optic endoscopic tube.
- First, bilateral nasal septal mucosa is incised in a C-shaped manner. The septal bone is approached through this incision.
- Then, sphenoidal rostrum and anterior wall of sphenoid sinus are gradually removed, a bone window is opened through the skull space.
- After that, the dura mater is passed and the lesion becomes visible.
- Finally, the tumor is removed using curette and basket with suction.
- Advantages:
- Disadvantages:
- Not for large tumors
- Recurrent sinusitis in the future
- Low cure rate in case of suprasellar adhesion to adjunct tissues
Craniotomy[5]
- Although the preferred procedure to excise the pituitary tumors is a trans-sphenoidal approach, but in some cases (1-4%) the size of the tumor or any suprasellar adhesion may require trans-cranial method.
- Situations requiring transcranial method include:
- Isolation by a narrow waist at the diaphragma sellae
- Containment within the cavernous sinus lateral to the carotid artery
- Projection anteriorly onto the planum sphenoidal
- Projection laterally into the middle fossa
- Skull base surgical procedure is also the option for pituitary tumor treatment but may encounter the problems that transsphenoidal method is faced with.
- Advantages:
- Resection of large tumors
- Ability to excise the tumors with suprasellar specific conditions
- Disadvantages:
- Long duration of post-operation recovery
- Damage to other parts of the brain
References
- ↑ "Prolactinoma | NIDDK".
- ↑ Colao A, Savastano S (2011). "Medical treatment of prolactinomas". Nat Rev Endocrinol. 7 (5): 267–78. doi:10.1038/nrendo.2011.37. PMID 21423245.
- ↑ Nomikos P, Buchfelder M, Fahlbusch R (2001). "Current management of prolactinomas". J Neurooncol. 54 (2): 139–50. PMID 11761431.
- ↑ Fan YP, Lv MH, Feng SY, Fan X, Hong HY, Wen WP; et al. (2014). "Full Endoscopic Transsphenoidal Surgery for Pituitary Adenoma-emphasized on Surgical Skill of Otolaryngologist". Indian J Otolaryngol Head Neck Surg. 66 (Suppl 1): 334–40. doi:10.1007/s12070-011-0317-4. PMC 3918297. PMID 24533411.
- ↑ Youssef AS, Agazzi S, van Loveren HR (2005). "Transcranial surgery for pituitary adenomas". Neurosurgery. 57 (1 Suppl): 168–75, discussion 168–75. PMID 15987585.