Non-Hodgkin lymphoma natural history, complications and prognosis: Difference between revisions
No edit summary |
No edit summary |
||
| Line 2: | Line 2: | ||
{{CMG}} | {{CMG}} | ||
==Overview== | ==Overview== | ||
Common complications of | Common complications of non-Hodgkin lymphoma include [[autoimmune hemolytic anemia]] and [[infection]]. The indolent non-Hodgkin lymphoma types are associated with relatively good prognosis. | ||
==Complications== | ==Complications== | ||
Common complications of | Common complications of non-Hodgkin lymphoma include:<ref> Non-Hodgkin lymphoma. medline plus. https://www.nlm.nih.gov/medlineplus/ency/article/000581.htm Accessed on September 22, 2015</ref> | ||
* [[Autoimmune hemolytic anemia]] | * [[Autoimmune hemolytic anemia]] | ||
* [[Infection]] | * [[Infection]] | ||
==Prognosis== | ==Prognosis== | ||
* The | * The non-Hodgkin lymphoma can be divided into two prognostic groups: indolent lymphomas and aggressive lymphomas.<ref name=”cancergov”>National Cancer Institute. Physician Data Query Database 2015. http://www.cancer.gov/publications/pdq</ref> | ||
* Indolent | * Indolent non-Hodgkin lymphoma types have a relatively good prognosis with a median survival as long as 20 years, but they usually are not curable in advanced clinical stages. Early-stage (stage I and stage II) indolent non-Hodgkin lymphoma can be effectively treated with radiation therapy alone. Most of the indolent types are nodular (or follicular) in morphology. | ||
* The aggressive type of | * The aggressive type of non-Hodgkin lymphoma has a shorter natural history, but a significant number of these patients can be cured with intensive combination chemotherapy regimens. | ||
* In general, with modern treatment of patients with | * In general, with modern treatment of patients with non-Hodgkin lymphoma, overall survival at 5 years is over 60%. Of patients with aggressive non-Hodgkin lymphoma, more than 50% can be cured. The vast majority of relapses occur in the first 2 years after therapy. The risk of late relapse is higher in patients who manifest both indolent and aggressive histologies. | ||
* While indolent | * While indolent non-Hodgkin lymphoma is responsive to [[immunotherapy]], [[radiation therapy]], and [[chemotherapy]], a continuous rate of relapse is usually seen in advanced stages. Patients can often be re-treated with considerable success as long as the disease histology remains low grade. Patients who present with or convert to aggressive forms of non-Hodgkin lymphoma may have sustained complete remissions with combination chemotherapy regimens or aggressive consolidation with marrow or stem cell support. | ||
===Prognostic Indexes=== | ===Prognostic Indexes=== | ||
====International Prognostic Index (IPI)==== | ====International Prognostic Index (IPI)==== | ||
| Line 21: | Line 21: | ||
:*Clinical stage | :*Clinical stage | ||
:*Sites of extranodal disease | :*Sites of extranodal disease | ||
However, it should be noted that the IPI was developed prior to the introduction of [[rituximab]]. [[Rituximab]] has become a standard part of therapy for [[B-cell]] non-Hodgkin lymphoma snd the impact on the prognostic value of the IPI is unclear. | |||
However, it should be noted that the IPI was developed prior to the introduction of [[rituximab]]. | |||
====Follicular Lymphoma International Prognostic Index (FLIPI)==== | ====Follicular Lymphoma International Prognostic Index (FLIPI)==== | ||
For the subtype of | For the subtype of non-Hodgkin lymphoma known as [[follicular lymphoma]], a modified version of the IPI called the FLIPI ([[International Prognostic Index|follicular lymphoma international prognostic index]]) has been developed. The factors which figure into the FLIPI are age, clinical stage, [[lactate dehydrogenase]] level, [[hemoglobin]] level, and number of nodal sites involved. As with the IPI, the FLIPI was developed and validated prior to the widespread use of [[rituximab]]. | ||
===5-Year Survival=== | ===5-Year Survival=== | ||
* Between 2004 and 2010, the 5-year relative survival of patients with non-Hodgkin lymphoma was 71.4%.<ref name="SEER">Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.</ref> | |||
* When stratified by age, the 5-year relative survival of patients with non-Hodgkin lymphoma was 77.2% and 60.9% for patients <65 and ≥ 65 years of age respectively.<ref name="SEER">Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.</ref> | |||
* When stratified by age, the 5-year relative survival of patients with | |||
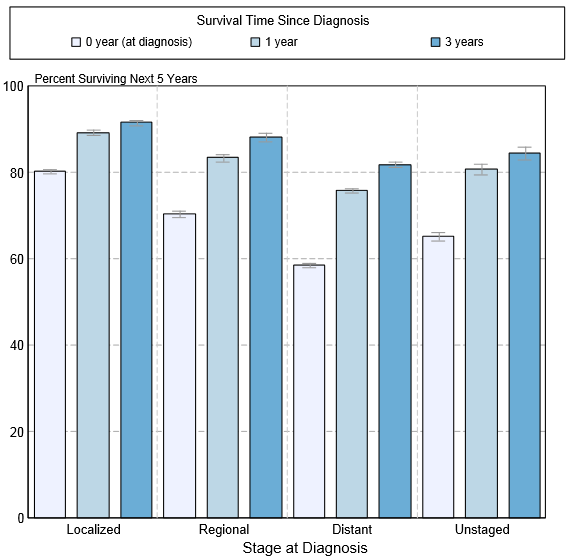
* The survival of patients with | * The survival of patients with non-Hodgkin lymphoma varies with the stage of the disease. Shown below is a table depicting the 5-year relative survival by the stage of non-Hodgkin lymphoma:<ref name="SEER">Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.</ref> | ||
{| style="cellpadding=0; cellspacing= 0; width: 600px;" | {| style="cellpadding=0; cellspacing= 0; width: 600px;" | ||
| Line 50: | Line 46: | ||
|} | |} | ||
* Shown below is an image depicting the 5-year conditional relative survival (probability of surviving in the next 5-years given the cohort has already survived 0, 1, 3 years) between 1998 and 2010 of | * Shown below is an image depicting the 5-year conditional relative survival (probability of surviving in the next 5-years given the cohort has already survived 0, 1, 3 years) between 1998 and 2010 of non-Hodgkin lymphoma by stage at diagnosis according to [[SEER]]. These graphs are adapted from [[SEER]]: The Surveillance, Epidemiology, and End Results Program of the National Cancer Institute.<ref name="SEER">Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.</ref> | ||
[[Image:5-year survival in non Hodgkin lymphoma in USA.PNG|5-year conditional relative survival (probability of surviving in the next 5-years given the cohort has already survived 0, 1, 3 years) between 1998 and 2010 of non Hodgkin lymphoma by stage at diagnosis according to SEER]] | [[Image:5-year survival in non Hodgkin lymphoma in USA.PNG|5-year conditional relative survival (probability of surviving in the next 5-years given the cohort has already survived 0, 1, 3 years) between 1998 and 2010 of non Hodgkin lymphoma by stage at diagnosis according to SEER]] | ||
Revision as of 18:24, 2 October 2015
|
Non-Hodgkin lymphoma Microchapters |
|
Differentiating Non-Hodgkin's Lymphoma |
|---|
|
Treatment |
|
Case Studies |
|
Non-Hodgkin lymphoma natural history, complications and prognosis On the Web |
|
American Roentgen Ray Society Images of Non-Hodgkin lymphoma natural history, complications and prognosis |
|
FDA on Non-Hodgkin lymphoma natural history, complications and prognosis |
|
CDC on Non-Hodgkin lymphoma natural history, complications and prognosis |
|
Non-Hodgkin lymphoma natural history, complications and prognosis in the news |
|
Blogs on Non-Hodgkin lymphoma natural history, complications and prognosis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Common complications of non-Hodgkin lymphoma include autoimmune hemolytic anemia and infection. The indolent non-Hodgkin lymphoma types are associated with relatively good prognosis.
Complications
Common complications of non-Hodgkin lymphoma include:[1]
Prognosis
- The non-Hodgkin lymphoma can be divided into two prognostic groups: indolent lymphomas and aggressive lymphomas.[2]
- Indolent non-Hodgkin lymphoma types have a relatively good prognosis with a median survival as long as 20 years, but they usually are not curable in advanced clinical stages. Early-stage (stage I and stage II) indolent non-Hodgkin lymphoma can be effectively treated with radiation therapy alone. Most of the indolent types are nodular (or follicular) in morphology.
- The aggressive type of non-Hodgkin lymphoma has a shorter natural history, but a significant number of these patients can be cured with intensive combination chemotherapy regimens.
- In general, with modern treatment of patients with non-Hodgkin lymphoma, overall survival at 5 years is over 60%. Of patients with aggressive non-Hodgkin lymphoma, more than 50% can be cured. The vast majority of relapses occur in the first 2 years after therapy. The risk of late relapse is higher in patients who manifest both indolent and aggressive histologies.
- While indolent non-Hodgkin lymphoma is responsive to immunotherapy, radiation therapy, and chemotherapy, a continuous rate of relapse is usually seen in advanced stages. Patients can often be re-treated with considerable success as long as the disease histology remains low grade. Patients who present with or convert to aggressive forms of non-Hodgkin lymphoma may have sustained complete remissions with combination chemotherapy regimens or aggressive consolidation with marrow or stem cell support.
Prognostic Indexes
International Prognostic Index (IPI)
The International Prognostic Index, or IPI, is the most widely used prognostic system for Non-Hodgkin's lymphoma. This system uses 5 factors:
- Age
- Lactate dehydrogenase level (a blood test)
- Performance status
- Clinical stage
- Sites of extranodal disease
However, it should be noted that the IPI was developed prior to the introduction of rituximab. Rituximab has become a standard part of therapy for B-cell non-Hodgkin lymphoma snd the impact on the prognostic value of the IPI is unclear.
Follicular Lymphoma International Prognostic Index (FLIPI)
For the subtype of non-Hodgkin lymphoma known as follicular lymphoma, a modified version of the IPI called the FLIPI (follicular lymphoma international prognostic index) has been developed. The factors which figure into the FLIPI are age, clinical stage, lactate dehydrogenase level, hemoglobin level, and number of nodal sites involved. As with the IPI, the FLIPI was developed and validated prior to the widespread use of rituximab.
5-Year Survival
- Between 2004 and 2010, the 5-year relative survival of patients with non-Hodgkin lymphoma was 71.4%.[3]
- When stratified by age, the 5-year relative survival of patients with non-Hodgkin lymphoma was 77.2% and 60.9% for patients <65 and ≥ 65 years of age respectively.[3]
- The survival of patients with non-Hodgkin lymphoma varies with the stage of the disease. Shown below is a table depicting the 5-year relative survival by the stage of non-Hodgkin lymphoma:[3]
| Stage | 5-year relative survival (%), (2004-2010) |
| All stages | 69.3% |
| Localized | 81.6% |
| Regional | 72.9% |
| Distant | 61.6% |
| Unstaged | 67% |
- Shown below is an image depicting the 5-year conditional relative survival (probability of surviving in the next 5-years given the cohort has already survived 0, 1, 3 years) between 1998 and 2010 of non-Hodgkin lymphoma by stage at diagnosis according to SEER. These graphs are adapted from SEER: The Surveillance, Epidemiology, and End Results Program of the National Cancer Institute.[3]
References
- ↑ Non-Hodgkin lymphoma. medline plus. https://www.nlm.nih.gov/medlineplus/ency/article/000581.htm Accessed on September 22, 2015
- ↑ National Cancer Institute. Physician Data Query Database 2015. http://www.cancer.gov/publications/pdq
- ↑ 3.0 3.1 3.2 3.3 Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.