Multiple myeloma pathophysiology
|
Multiple myeloma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Multiple myeloma pathophysiology On the Web |
|
American Roentgen Ray Society Images of Multiple myeloma pathophysiology |
|
Risk calculators and risk factors for Multiple myeloma pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overveiw
Pathophysiology
- Multiple myeloma develops in post-germinal center B lymphocytes.
- A chromosomal translocation between the immunoglobulin heavy chain gene (on the fourteenth chromosome, locus 14q32) and an oncogene (often 11q13, 4p16.3, 6p21, 16q23 and 20q11[1]) is frequently observed in patients with multiple myeloma.
- This mutation results in dysregulation of the oncogene which is thought to be an important initiating event in the pathogenesis of myeloma.
- The result is proliferation of a plasma cell clone and genomic instability that leads to further mutations and translocations.
- The chromosome 14 abnormality is observed in about 50% of all cases of myeloma. Deletion of (parts of) the thirteenth chromosome is also observed in about 50% of cases.
- Production of cytokines (especially IL-6) by the plasma cells causes much of their localised damage, such as osteoporosis, and creates a microenvironment in which the malignant cells thrive. Angiogenesis (the attraction of new blood vessels) is increased.
- The produced antibodies are deposited in various organs, leading to renal failure, polyneuropathy and various other myeloma-associated symptoms.
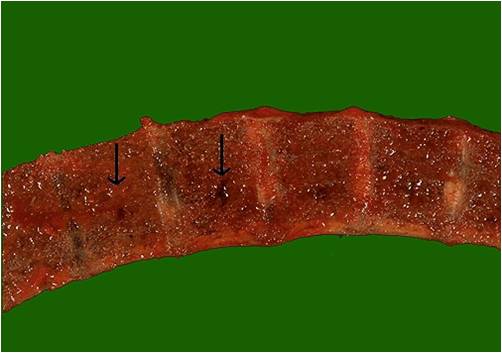
Gross Pathology
|

|
Microscopic Pathology
-
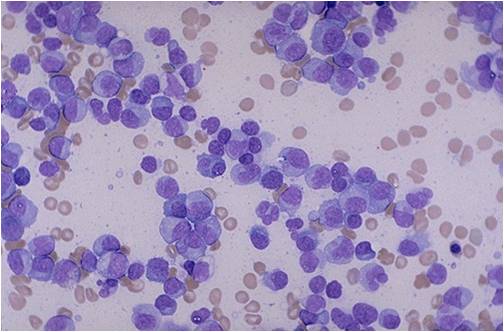
Multiple Myeloma [2]
-
Bone marrow aspiration in multiple myeloma.
(Image courtesy of Melih Aktan M.D.) -
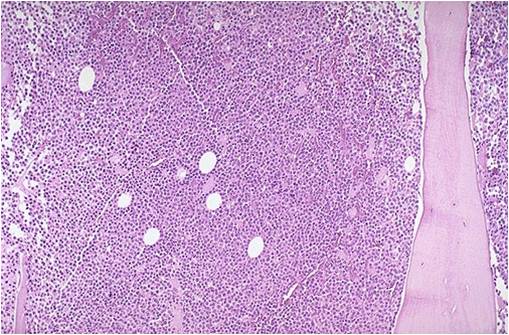
Bone marrow biopsy in multiple myeloma.
(Image courtesy of Melih Aktan M.D.) -
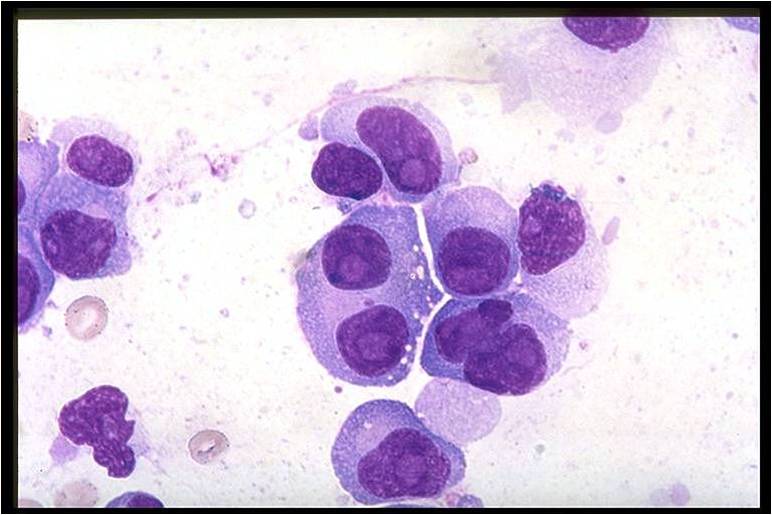
Bone marrow in multiple myeloma.
(Image courtesy of Melih Aktan M.D.) -
Bone marrow in multiple myeloma.
(Image courtesy of Melih Aktan M.D.)
References
- ↑ Kyle RA, Rajkumar SV. Multiple myeloma. N Engl J Med 2004;351:1860-73. PMID 15509819.
- ↑ http://picasaweb.google.com/mcmumbi/USMLEIIImages
![Multiple Myeloma [2]](/images/a/a5/Multiple_Myeloma.jpg)