Membranous glomerulonephritis pathophysiology: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Membranous glomerulonephritis}} | {{Membranous glomerulonephritis}} | ||
* {{CMG}}; {{AE}} | * {{CMG}}; {{AE}} {{SAH}} | ||
==Overview== | ==Overview== | ||
* Hall mark of Membranous glomerulonephritis is subepithelial deposits of IgG. | * Hall mark of Membranous glomerulonephritis is subepithelial deposits of IgG. | ||
== | == | ||
* The complement system ( C3 and C5-C9) constitutes for the 75% of the cases. | * The complement system ( C3 and C5-C9) constitutes for the 75% of the cases. | ||
* IgM and IgA are the features of SLE, which constitutes the 30% of idiopathic cases. | * IgM and IgA are the features of SLE, which constitutes the 30% of idiopathic cases. | ||
| Line 47: | Line 41: | ||
* The two loci are within the genes for the PLA2R on chromosome 2q24, and the human leukocyte antigen (HLA) complex class II alpha chain 1A (''HLA-DQA1'') on chromosome 6p21. | * The two loci are within the genes for the PLA2R on chromosome 2q24, and the human leukocyte antigen (HLA) complex class II alpha chain 1A (''HLA-DQA1'') on chromosome 6p21. | ||
* PLA2R variants have also been found in other cohorts with idiopathic MN, although no single variant was consistently found that could explain the association with disease [59]. The PLA2R has been identified as a major antigen in idiopathic MN. | * PLA2R variants have also been found in other cohorts with idiopathic MN, although no single variant was consistently found that could explain the association with disease [59]. The PLA2R has been identified as a major antigen in idiopathic MN. | ||
* Stages of Glomerulonephritis: | |||
* There are 4 stages of Membranous glomerulonephritis depending upon the sunepithelial deposits. | |||
* Stage 1: Include less number od deposits. The deposits are scattered. on light microscopy the GBM is not thick. | |||
* Stage 2: The immunoglobin deposits are uniform but they are numerous in number. On light microscopy the basement membrane is even with normal spikes. | |||
* Stage 3: The immunoglobin are entirely incorporated within GBM. The basement membrane is still normal. | |||
* The silver staining of stage 2 and 3 shows GBM but not the immune deposits. | |||
* Stage 4 : On Electron microscopy there is rarefaction of deposits. | |||
==Associated Conditions== | ==Associated Conditions== | ||
Revision as of 16:26, 3 July 2018
|
Membranous glomerulonephritis Microchapters |
|
Differentiating Membranous glomerulonephritis from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Membranous glomerulonephritis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Membranous glomerulonephritis pathophysiology |
|
Directions to Hospitals Treating Membranous glomerulonephritis |
|
Risk calculators and risk factors for Membranous glomerulonephritis pathophysiology |
- Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Syed Ahsan Hussain, M.D.[2]
Overview
- Hall mark of Membranous glomerulonephritis is subepithelial deposits of IgG.
==
- The complement system ( C3 and C5-C9) constitutes for the 75% of the cases.
- IgM and IgA are the features of SLE, which constitutes the 30% of idiopathic cases.
Phospholipase A2 receptor
- The M-type PLA2R is the major antigen in human idiopathic MN. It is expressed in glomerular podocytes.
- There was no colocalization of PLA2R in secondary MN biopsies.
- PLA2R antigen detected within immune deposits by immunofluorescence of the biopsy specimen. [26]
- Detection of the immune complex specificity is 100 percent.
Thrombospondin type-1
- THSD7A has been found in patients with idiopathic MN who are negative for anti-PLA2R antibodies.
Neutral endopeptidase
- Anti-neutral endopeptidase antibodies caused MN in the neonates.
- It resolves months after birth.
- The T helper-2 predominates in MN and minimal change disease.
| HLA susceptibility 1 | Environmental factors | ||||||||||||||||||||||||||||
| Variant of PLA2R1 on podocyte surface | |||||||||||||||||||||||||||||
| Innate immunity activation and inflammation dendritic cell sense epitope of PLA2R1 and present them for adaptive immunity | |||||||||||||||||||||||||||||
| Production of auto-immune antibody IgG4/IgG1 which attach them self to epitope on podocyte surface | |||||||||||||||||||||||||||||
| In Situ formation and shedding of subepithelial immune complex | |||||||||||||||||||||||||||||
| Complement activationMANNAN PATHWAY and T cell activation | |||||||||||||||||||||||||||||
| Which lead to cytokine release oxygen derivative release membrane attack complex C5-C9 | |||||||||||||||||||||||||||||
| Podocyte injury by apoptosis altered lectin cytoskeleton loss of silt pore integrity loss of glomerular permeability proteinuria | |||||||||||||||||||||||||||||
Genetics
- Single-nucleotide polymorphisms (SNPs) at two loci that are highly associated with idiopathic MN. [58]
- The two loci are within the genes for the PLA2R on chromosome 2q24, and the human leukocyte antigen (HLA) complex class II alpha chain 1A (HLA-DQA1) on chromosome 6p21.
- PLA2R variants have also been found in other cohorts with idiopathic MN, although no single variant was consistently found that could explain the association with disease [59]. The PLA2R has been identified as a major antigen in idiopathic MN.
- Stages of Glomerulonephritis:
- There are 4 stages of Membranous glomerulonephritis depending upon the sunepithelial deposits.
- Stage 1: Include less number od deposits. The deposits are scattered. on light microscopy the GBM is not thick.
- Stage 2: The immunoglobin deposits are uniform but they are numerous in number. On light microscopy the basement membrane is even with normal spikes.
- Stage 3: The immunoglobin are entirely incorporated within GBM. The basement membrane is still normal.
- The silver staining of stage 2 and 3 shows GBM but not the immune deposits.
- Stage 4 : On Electron microscopy there is rarefaction of deposits.
Associated Conditions
Hepatitis B
The most frequent glomerulopathy in patients infected with hepatitis B virus is MGN followed by membranoproliferative GN. The antigens Core (HBcAg) and e (HBeAg) seem the most important in the pathogenesis of hepatitis B-associated MGN. In these cases the antigens, or their antibodies, are identified in the glomerular immune deposits. It is not clear what is first deposited: the Ag., the Ac. or the Ag-Ac complex previously formed (circulating). Prevalence of MGN in the infection is not known, but in children with MGN the carrier stage is detected in around 20% of cases, with higher rates in endemic countries. In adults the percentage of patients with MGN carrying hepatitis B virus is lower than in children. In GNM cases associated with this infection there are more frequently mesangial hypercellularity, endocapillary proliferation, subendothelial immune deposits, and tubuloreticular endothelial structures (electron microscopy). It is frequent that appears with hypocomplementemia. The prognosis of MGN in hepatitis B patients seem more favorable, with most frequency of remission and less probability of evolution to terminal renal damage.
Hepatitis C
In this infection disease also secondary MGN can appear, although membranoproliferative GN is more frequent. In many studies have not been identified antigens of the virus, or Acs against these, in the glomerular deposits. Clinic expression can be similar to idiopathic MGN or it may appear with asymptomatic proteinuria.
Congenital Syphilis
MGN is a rare complication in congenital syphilis, but it is a well-recognized cause of NS in children with this infection. Other glomerular disease in congenital syphilis include nephritic syndrome and crescentic GN with rapidly progressive disease. We have seen cases with these types of glomerular disease and there is a dramatic improvement with the antibiotic treatment. Several studies have demonstrated the presence of antigens of Treponema pallidum in the immune glomerular deposits.
Systemic Lupus Erythematosis
the histopathologic presentation is very variable and there is combination of morphologic changes: MGN with subendothelial deposits, endocapillary and/or mesangial proliferation, crescents, combination with characteristics of membranoproliferative GN, and other patterns. In the most recent lupus nephritis classification, pure MGN (class V) is only diagnosed if there are no other active lesions; if there is combination with active lesions it is diagnosed as combination of class V and class III or IV only if there are lesions with membranous characteristics in more than 50% of the tuft in more than 50% of glomeruli. Occasional subepithelial deposits and “spikes” formation are very frequent in class III and IV lupus nephritis. In most of these cases we find C1q glomerular deposits.
Malignancy
The neoplasms more frequently associated with MGN are lung, breast, colon, stomach and kidney carcinomas, leukemia and lymphomas (Hodgkin’s and non-Hodgkin’s), but there is information of MGN in many other cancer types. Incidence of cancer in patients with MGN is approximately 1%. The histologic and immunopathologic findings and the clinical presentation are similar to those of idiopathic forms of MGN. The association between MGN and neoplasms is supported by the clinical course, the immune response of the host to the tumor and the glomerular pathology, nevertheless, in very few cases is documented an antigen of the tumor, or its antibody, in glomerular deposits. It is possible that the immune response against the neoplasm, in a propitious genetic context, allow the development of MGN. The prognosis of the glomerulopathy depend on that of the neoplasm. If there are treatment and response of this last one, the MGN tends to disappear.
References
-
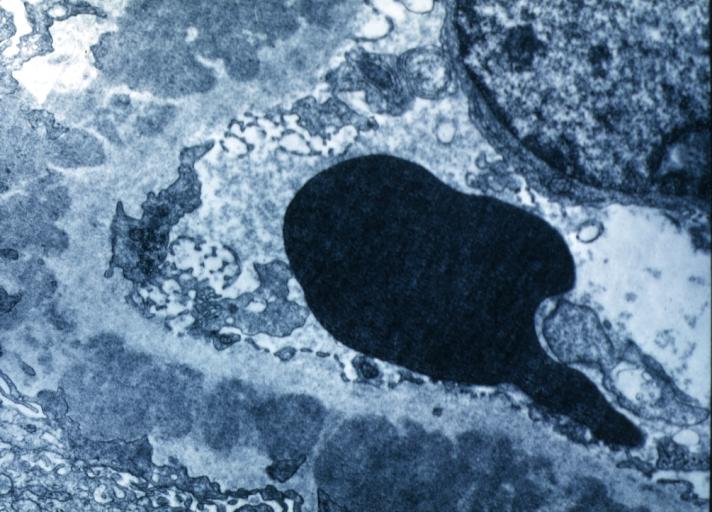
Membranous Glomerulonephritis: Electron micrography. An excellent example to show thickened basement membrane and immune complexes.
-
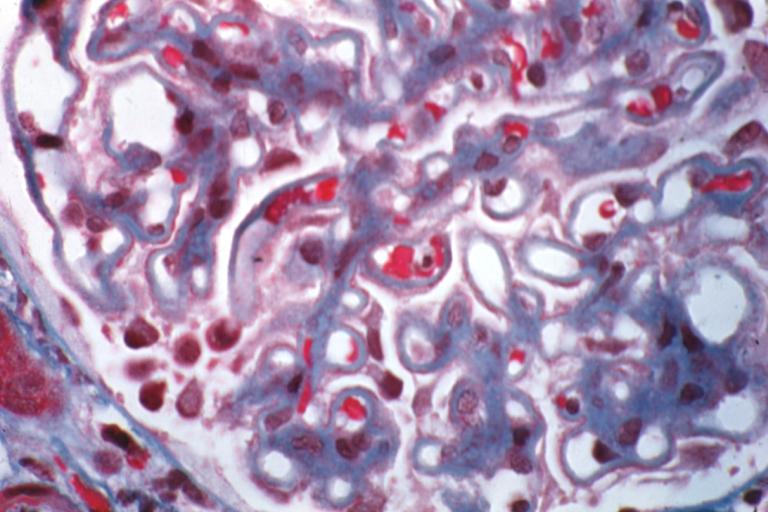
Membranous Glomerulonephritis: Micro trichrome high mag excellent to show thickened capillary basement membranes
-
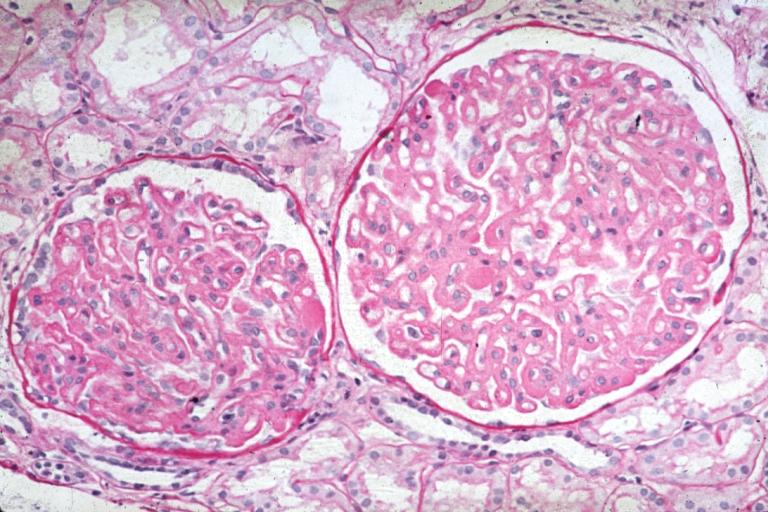
Membranous Glomerulonephritis: Micro PAS high mag excellent example of this lesion
-
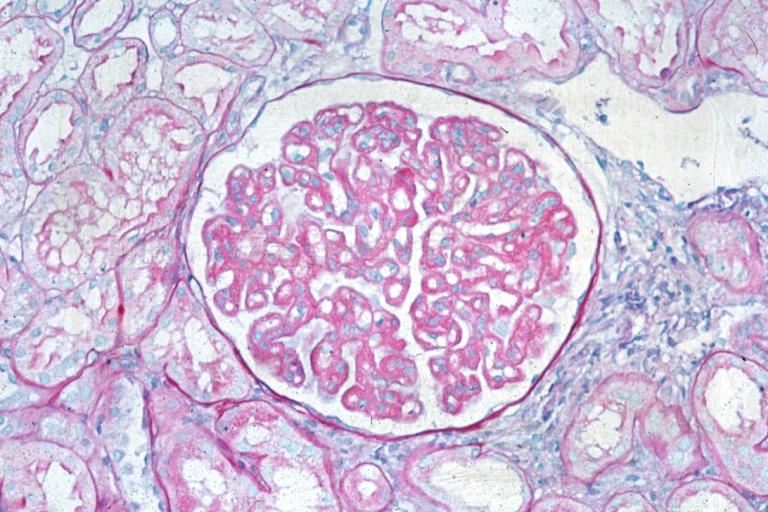
Membranous Glomerulonephritis: Micro PAS med mag