Leopard syndrome history and symptoms
|
Leopard syndrome Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Leopard syndrome history and symptoms On the Web |
|
American Roentgen Ray Society Images of Leopard syndrome history and symptoms |
|
Risk calculators and risk factors for Leopard syndrome history and symptoms |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mohamed Moubarak, M.D. [2]
Overview
History and Symptoms
The name of the condition is a mnemonic, originally coined in 1969,[1] as the condition is characterized by some of the following seven conditions, the first letters of which spell Leopard, along with the characteristic "freckling" of the skin, caused by the lentigines that is reminiscent of the large cat
- Lentigines - Reddish-brown to dark brown macules (surface skin lesion) generally occurring in a high number (10,000+) over a large portion of the skin, at times higher than 80% coverage. These can even appear inside the mouth (Buccal mucosa), or on the surface of the eye (scleral). These have irregular borders and range in size from 1 mm in diameter to café-au-lait spot's, several centimetres in diameter. Also, some areas of vitiligo-like hypopigmentation may be observed
- Electrocardiographic conduction abnormalities: Generally observed on an electrocardiograph as a bundle branch block
- Ocular hypertelorism- Wideset eyes, which lead to a similar facial resemblance between patients. Facial abnormalities are the second highest occurring symptom after the lentigines. Abnormalities also include: broad nasal root, prognathism (protruding lower jaw), or low-set, possibly rotated ears
- Pulmonary stenosis - Narrowing of the pulmonary artery as it exits the heart. Other cardiac abnormalities may be present, including aortic stenosis, or mitral valve prolapse
- Abnormal genitalia - Usually cryptorchidism (retention of testicles in body) or monorchism (single testicle). In female patients, this presents as missing or single ovaries, much harder by nature to detect. Ultrasound imaging is performed at regular intervals, from the age of 1 year, to determine if ovaries are present
- Retarded growth - Slow, or stunted growth. Most newborns with this syndrome are of normal birth weight and length, but will often slow within the first year
- Sensorineural deafness
The presence of all of these hallmarks is not needed for a diagnosis. A clinical diagnosis is considered made when, with lentigines present there are 2 other symptoms observed, such as EKG abnormalities and ocular hypertelorism, or without lentigines, 3 of the above conditions are present, with a first-degree relative (i.e. parent, child, sibling) with a clinical diagnosis.[2]
- additional dermatologic abnormalities (axillary freckling, localized hypopigmentation, interdigital webbing, hyperelastic skin)
- Mild mental retardation is observed in about 30% of those affected with the syndrome
- Nystagmus (involuntary eye movements), seizures, or hyposmia (reduced ability to smell) has been documented in a few patients
- In 2004, a patient was reported with recurrent upper extremity aneurysms that required surgical repairs.[3]
- In 2006, a Leopard syndrome patient was reported with acute myelogenous leukemia.[4]
Unfortunately, due to the rarity of the syndrome itself, it is hard to determine whether certain additional diseases are actually a threat of the syndrome. With a base population of possibly less than one thousand individuals, one or two outlying cases can skew the statistical population very quickly.
-
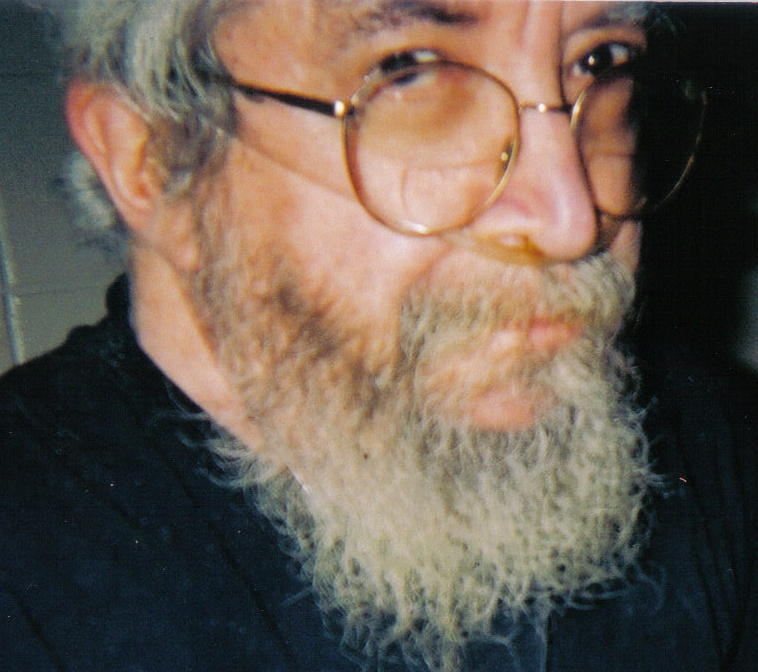
Three-quarter facial view, first generation patient showing slight prognathism and low set ears.
-
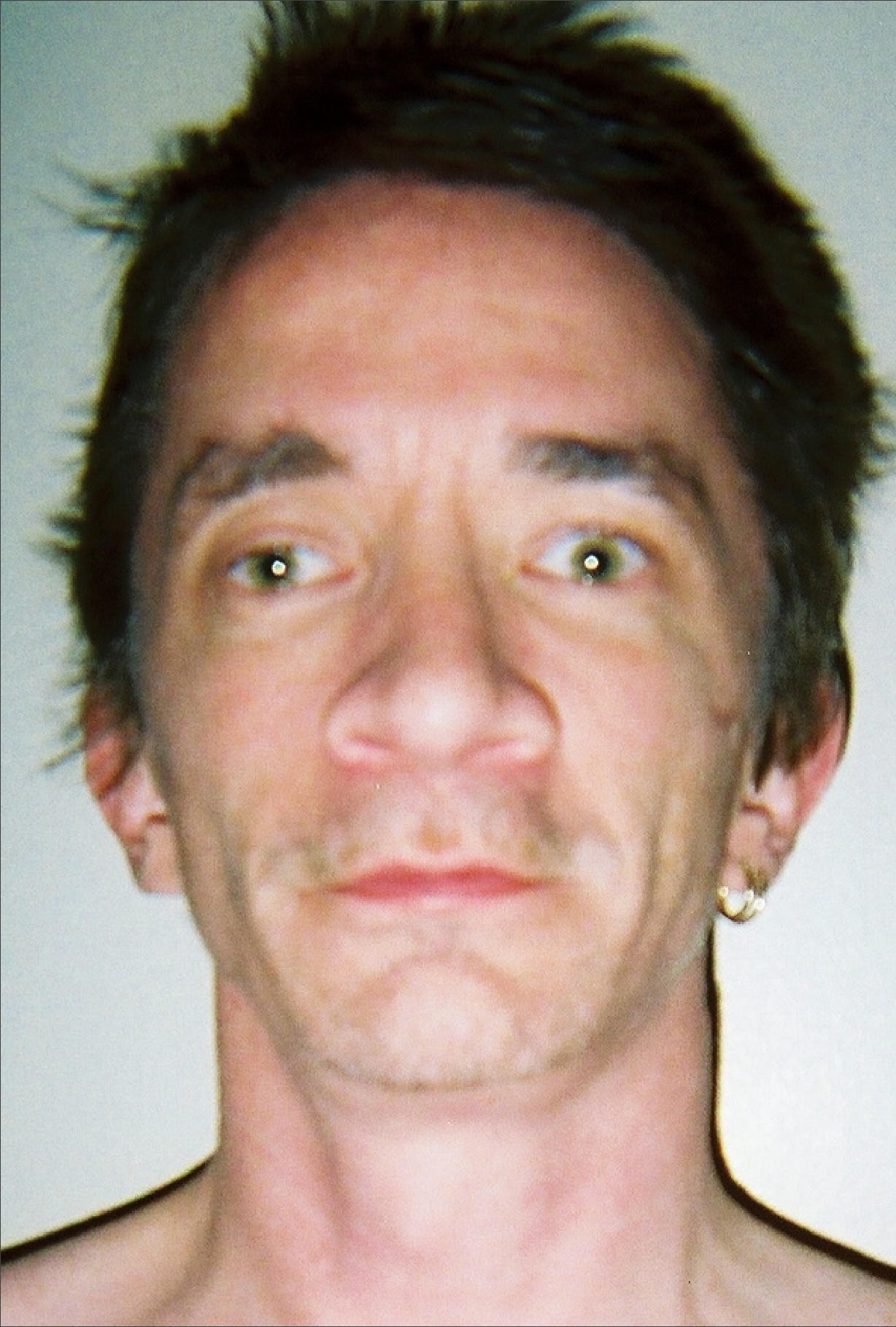
Thirty seven year old, second generation patient, exhibiting hypertelorism, broad nasal root, slight ptosis
-
Hand of thirty seven year old patient showing interdigital webbing
-
Thirty seven year old patient demonstrating hyperelasticity
-
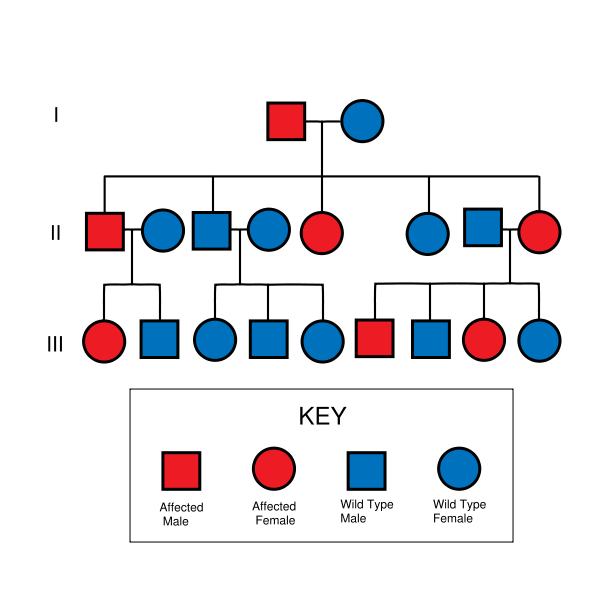
LEOPARD syndrome is inherited in an autosomal dominant fashion, although it can also arise due to spontaneous mutation.
-
21 month old, third generation patient, confirmed by genetic tests as Y279C, exhibiting ocular hyperteliorism, cephalofacial similarity.
-
Torso of thirty seven year old, second generation patient, exhibiting lentiginosis.
Referene
- ↑ Gorlin RJ, Anderson RC, Blaw M (1969). "Multiple lentigenes syndrome". Am. J. Dis. Child. 117 (6): 652–62. PMID 5771505.
- ↑ Voron DA, Hatfield HH, Kalkhoff RK (1976). "Multiple lentigines syndrome. Case report and review of the literature". Am. J. Med. 60 (3): 447–56. PMID 1258892.
- ↑ Yagubyan M, Panneton JM, Lindor NM, Conti E, Sarkozy A, Pizzuti A (2004). "LEOPARD syndrome: a new polyaneurysm association and an update on the molecular genetics of the disease". J. Vasc. Surg. 39 (4): 897–900. doi:10.1016/j.jvs.2003.11.030. PMID 15071461. Unknown parameter
|month=ignored (help) - ↑ Uçar C, Calýskan U, Martini S, Heinritz W (2006). "Acute myelomonocytic leukemia in a boy with LEOPARD syndrome (PTPN11 gene mutation positive)". J. Pediatr. Hematol. Oncol. 28 (3): 123–5. doi:10.1097/01.mph.0000199590.21797.0b. PMID 16679933. Unknown parameter
|month=ignored (help)