Ischemic stroke MRI
|
Ischemic Stroke Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Ischemic stroke MRI On the Web |
|
American Roentgen Ray Society Images of Ischemic stroke MRI |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]Associate Editor(s)-in-Chief: Aysha Anwar, M.B.B.S[2]Maryam Hadipour, M.D.[3]
Overview
MR diffusion weighted imaging is the most sensitive and specific test for diagnosing ischemic stroke and may help detect presence of infarction in few minutes of onset of symptoms. It may also help differentiate viable tissue from infarct area if combined with MR perfusion. For diagnosing ischemic stroke in the emergency setting, MRI scan has the sensitivity and specificity of 83% and 98% respectively.
MRI
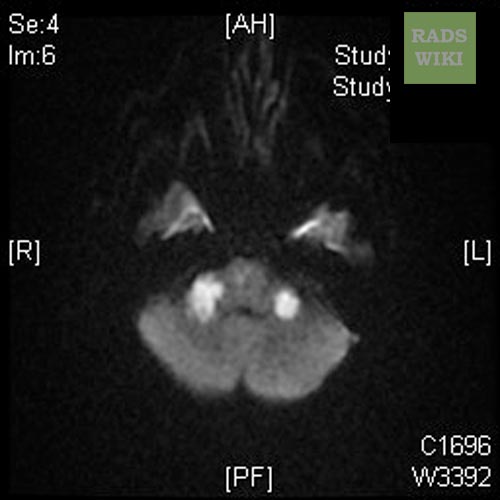
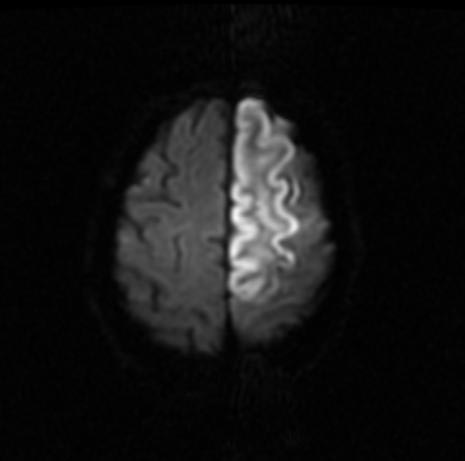
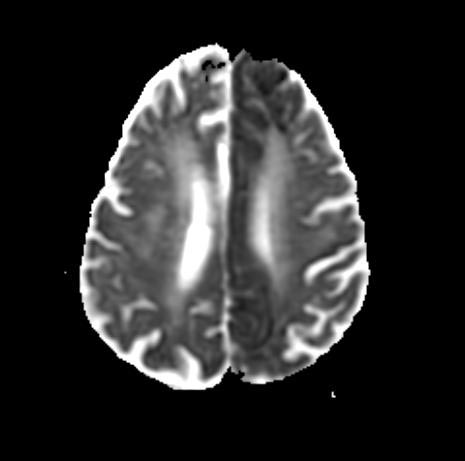
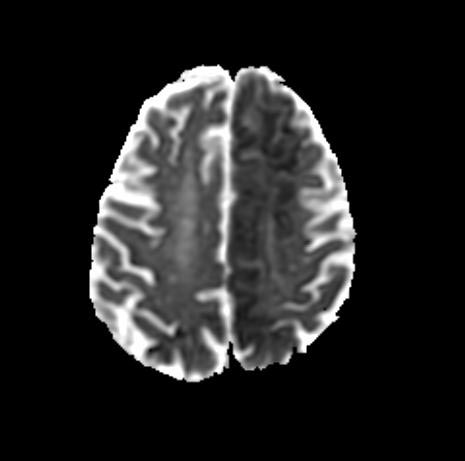
MRI diffusion weighted imaging
MR diffusion weighted imaging is the most sensitive and specific test for diagnosing ischemic stroke and may help detect presence of infarction in few minutes of onset of symptoms. It may also help differentiate viable tissue from infarct area if combined with MR perfusion. For diagnosing ischemic stroke in the emergency setting, MRI scan has the sensitivity and specificity of 83% and 98% respectively.[1] MRI scan is superior to CT scan for being more sensitive and specific in detection of lacunar and posterior fossa infarcts, differentiation between acute and chronic stroke and detection of microbleeds. Another additional advantage is absence of ionising radiation compared to CT scan. Some of the disadvantages of MRI scan may include lack of availability in acute setting, higher cost, inability to use it in patients with metallic implants. MRI with contrast cannot be used in patients with renal failure.[2][3]
MRI perfusion weighted imaging
May help determine the diagnosis, selection of patients and time window for thrombolytic therapy and to determine the prognosis in ischemic stroke. It uses contrast material to give an insight into the perfusion of cerebral tissues by blood and may help measure cerebral blood flow volume and transit time, thus helping determine infarct area and penumbra.[3][4][5]
For AHA/ASA guidelines for MRI in patients with ischemic stroke, please click here
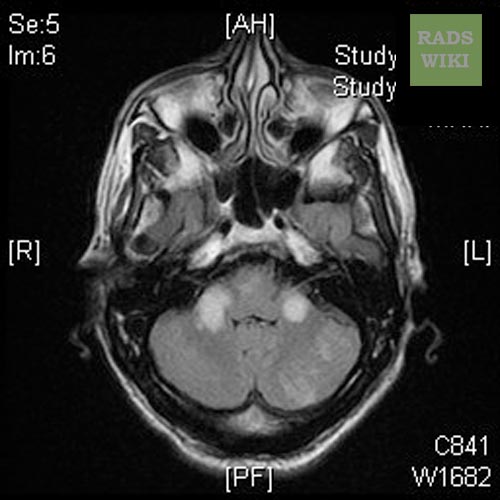
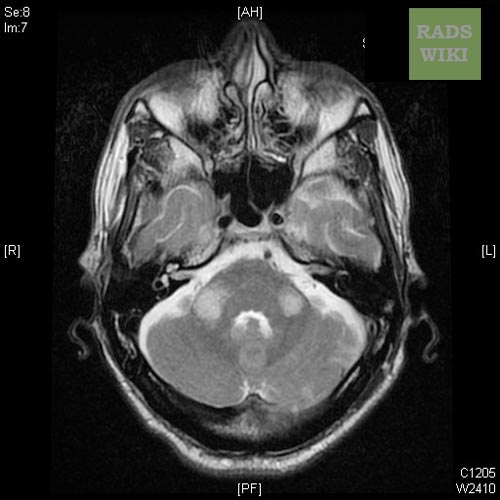
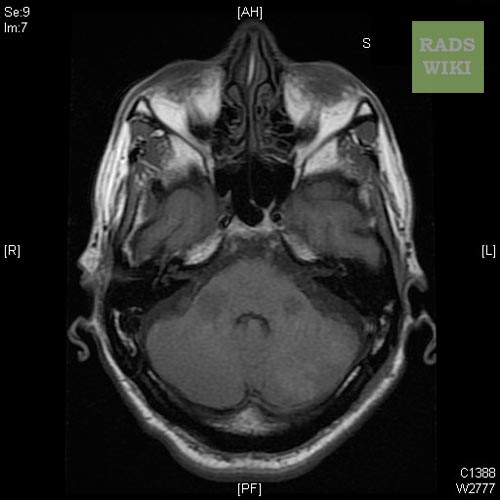
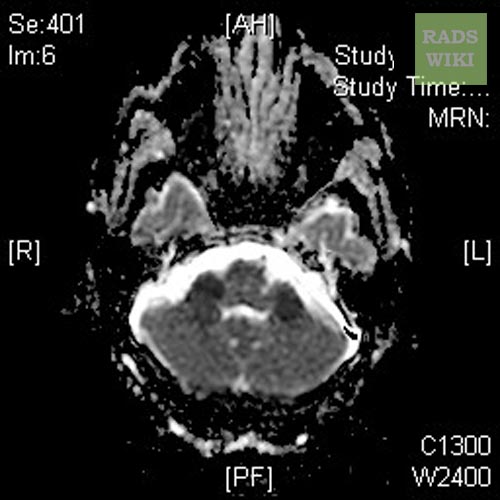
Patient No 1: Change in Mental Status (Images courtesy of RadsWiki)
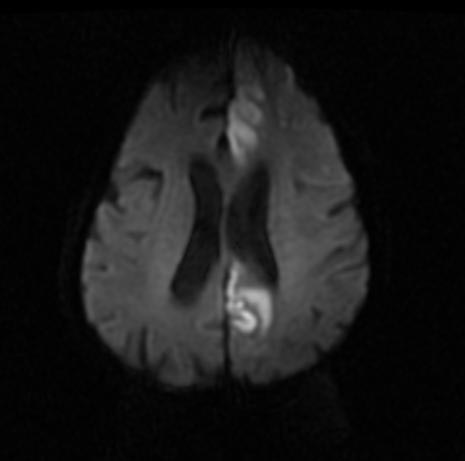
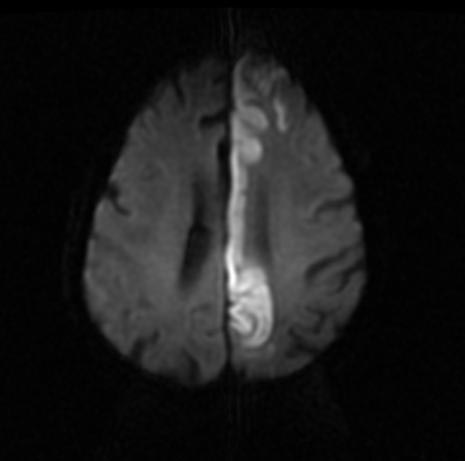
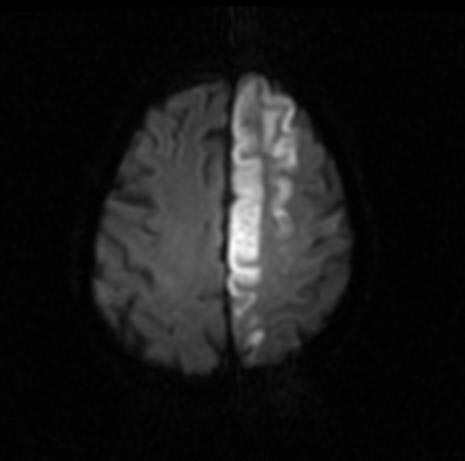
Patient No 2: Left ACA Infarction
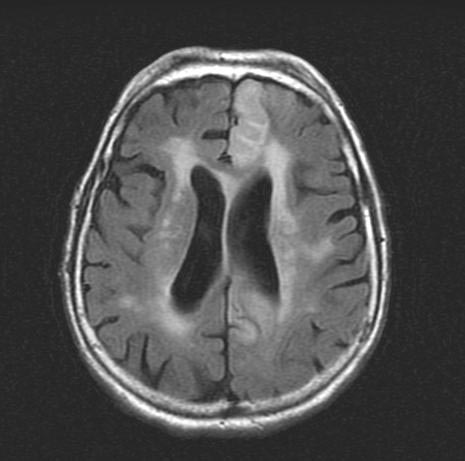
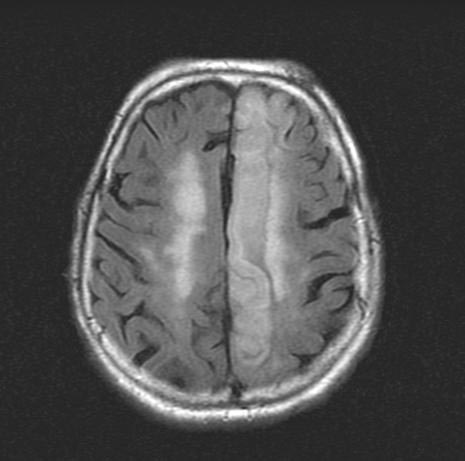
Conventional brain MRI studies can take up to one hour to complete. The study is not very good at detecting cytotoxic or intracellular edema that is seen in the acute or less than 24 hour phase of stroke. Standard MRI images (T1 and T2) are good at detecting vasogenic edema that is present in the subacute phase of stroke and is seen at greater than 24 hours to several days. Fast spin echo T2- weighted sequences can clearly demonstrate areas of edema not visible on the CT and can help identify a subacute stroke.[6]
Fluid attenuated inversion recovery (FLAIR) sequences are designed to suppress signal from the CSF so that it will appear dark. FLAIR images provide good conspicuity of acute subarachnoid hemorrhage, as compared to conventional T-1 and T-2 weighted images and are useful in the initial evaluation of the acute stroke patient suspected of having a subarachnoid hemorrhage. Subarachnoid hemorrhage appears bright on FLAIR images and so becomes readily apparent.[7]
References
- ↑ Chalela, J (2007). "Magnetic resonance imaging and computed tomography in emergency assessment of patients with suspected acute stroke: a prospective comparison". Lancet. 369 (9558): 293–8. PMID 17258669. Retrieved 2008-01-22. Unknown parameter
|coauthors=ignored (help) - ↑ Wintermark M, Sanelli PC, Albers GW, Bello J, Derdeyn C, Hetts SW; et al. (2013). "Imaging recommendations for acute stroke and transient ischemic attack patients: A joint statement by the American Society of Neuroradiology, the American College of Radiology, and the Society of NeuroInterventional Surgery". AJNR Am J Neuroradiol. 34 (11): E117–27. doi:10.3174/ajnr.A3690. PMC 4072500. PMID 23907247.
- ↑ 3.0 3.1 Leiva-Salinas C, Wintermark M (2010). "Imaging of acute ischemic stroke". Neuroimaging Clin N Am. 20 (4): 455–68. doi:10.1016/j.nic.2010.07.002. PMC 2965616. PMID 20974371.
- ↑ https://radiopaedia.org/articles/mr-perfusion-weighted-imaging-1 Accessed on November 17, 2016
- ↑ Copen WA, Schaefer PW, Wu O (2011). "MR perfusion imaging in acute ischemic stroke". Neuroimaging Clin N Am. 21 (2): 259–83, x. doi:10.1016/j.nic.2011.02.007. PMC 3135980. PMID 21640299.
- ↑ Wessels T, Wessels C, Ellsiepen A, Reuter I, Trittmacher S, Stolz E, Jauss M (January 2006). "Contribution of diffusion-weighted imaging in determination of stroke etiology". AJNR Am J Neuroradiol. 27 (1): 35–9. PMC 7976056 Check
|pmc=value (help). PMID 16418352. - ↑ Latchaw RE, Alberts MJ, Lev MH, Connors JJ, Harbaugh RE, Higashida RT, Hobson R, Kidwell CS, Koroshetz WJ, Mathews V, Villablanca P, Warach S, Walters B (November 2009). "Recommendations for imaging of acute ischemic stroke: a scientific statement from the American Heart Association". Stroke. 40 (11): 3646–78. doi:10.1161/STROKEAHA.108.192616. PMID 19797189.