Ischemic stroke history and symptoms
|
Ischemic Stroke Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Ischemic stroke history and symptoms On the Web |
|
American Roentgen Ray Society Images of Ischemic stroke history and symptoms |
|
Risk calculators and risk factors for Ischemic stroke history and symptoms |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]Associate Editor(s)-in-Chief: Aysha Anwar, M.B.B.S[2] Khizer Yaseen, M.B.B.S.[3]
Overview
The diagnosis of ischemic stroke largely depends on the history and clinical presentation of patient. Detailed history may give clue about the underlying cause, rule out differential diagnosis and determine the site of infarction. History of sudden onset muscle weakness, slurring of speech, loss of vision, and loss of consciousness may suggest stroke as one of the initial differential diagnosis. This warrants detailed neurological examination and imaging studies to make a definitive diagnosis and rule out other conditions which mimics stroke. Detailed neurological examination may help determine the site of infarction and vessel involved which may suggest the treatment options and prognosis of patient.
History and Symptoms
Past history of hypertension, diabetes mellitus, TIA and amaurosis fugax and prosthetic valves may help determine the underlying cause. The symptoms of an ischemic stroke vary widely depending on the site and blood supply of the area involved:[1][2][3][4][5][6]
Patients younger than 60 years presenting with ischemic stroke without an identified cause are more likely to have a pathogenic patent foramen ovale.[7]
| Vessel involved | Site of infarction | History and symptoms |
|---|---|---|
Anterior cerebral artery [1][2]
|
Superficial branch |
|
|
Deep branches (medial lenticulostriate, Heubner's artery)[9][10]
|
||
Middle cerebral artery[3]
|
|
|
|
| |
|
Classical lacunar syndromes[17][18][19]
| |
| Posterior cerebral artery[4][5][6] |
Cortical branches[4]'
|
Right PCA[21]
|
|
Ganglionic branches[5] |
| |
| Vertebrobasilar artery[26] |
| |
| ||
Medial pontine syndrome
| ||
| ||
|
| |
|
|
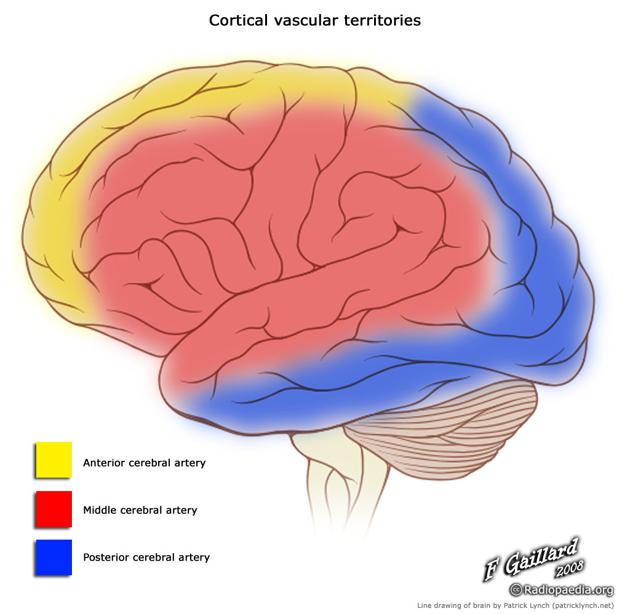
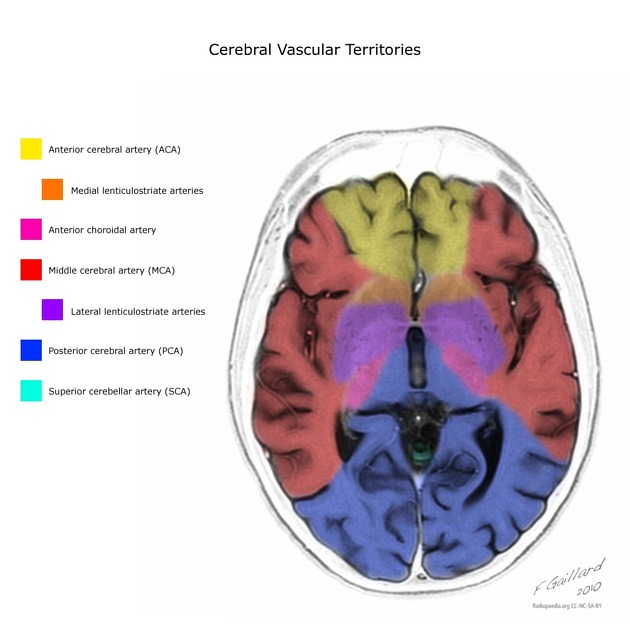
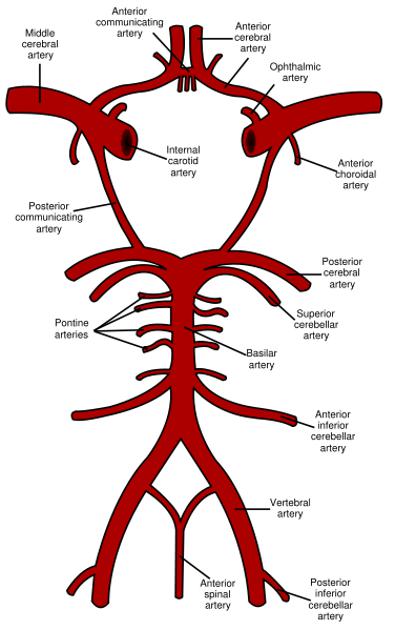
Blood supply of brain
References
- ↑ 1.0 1.1 1.2 1.3 Nagaratnam N, Davies D, Chen E (1998). "Clinical effects of anterior cerebral artery infarction". J Stroke Cerebrovasc Dis. 7 (6): 391–7. PMID 17895117.
- ↑ 2.0 2.1 2.2 2.3 2.4 Kumral E, Bayulkem G, Evyapan D, Yunten N (2002). "Spectrum of anterior cerebral artery territory infarction: clinical and MRI findings". Eur J Neurol. 9 (6): 615–24. PMID 12453077.
- ↑ 3.0 3.1 Lemieux F, Lanthier S, Chevrier MC, Gioia L, Rouleau I, Cereda C; et al. (2012). "Insular ischemic stroke: clinical presentation and outcome". Cerebrovasc Dis Extra. 2 (1): 80–7. doi:10.1159/000343177. PMC 3492997. PMID 23139684.
- ↑ 4.0 4.1 4.2 4.3 Brandt T, Steinke W, Thie A, Pessin MS, Caplan LR (2000). "Posterior cerebral artery territory infarcts: clinical features, infarct topography, causes and outcome. Multicenter results and a review of the literature". Cerebrovasc Dis. 10 (3): 170–82. doi:16053 Check
|doi=value (help). PMID 10773642. - ↑ 5.0 5.1 5.2 5.3 5.4 Cereda C, Carrera E (2012). "Posterior cerebral artery territory infarctions". Front Neurol Neurosci. 30: 128–31. doi:10.1159/000333610. PMID 22377879.
- ↑ 6.0 6.1 6.2 Yamamoto Y, Georgiadis AL, Chang HM, Caplan LR (1999). "Posterior cerebral artery territory infarcts in the New England Medical Center Posterior Circulation Registry". Arch Neurol. 56 (7): 824–32. PMID 10404984.
- ↑ Saver JL, Mattle HP, Thaler D. Patent Foramen Ovale Closure Versus Medical Therapy for Cryptogenic Ischemic Stroke: A Topical Review. Stroke. 2018 Jun;49(6):1541-1548. doi: 10.1161/STROKEAHA.117.018153. Epub 2018 May 14. PMID: 29760277.
- ↑ Alexander MP, Schmitt MA (1980). "The aphasia syndrome of stroke in the left anterior cerebral artery territory". Arch Neurol. 37 (2): 97–100. PMID 7356415.
- ↑ 9.0 9.1 9.2 den Heijer T, Ruitenberg A, Bakker J, Hertzberger L, Kerkhoff H (2007). "Neurological picture. Bilateral caudate nucleus infarction associated with variant in circle of Willis". J Neurol Neurosurg Psychiatry. 78 (11): 1175. doi:10.1136/jnnp.2006.112656. PMC 2117617. PMID 17940169.
- ↑ 10.0 10.1 Mendez MF, Adams NL, Lewandowski KS (1989). "Neurobehavioral changes associated with caudate lesions". Neurology. 39 (3): 349–54. PMID 2927642.
- ↑ 11.0 11.1 Mizuta H, Motomura N (2006). "Memory dysfunction in caudate infarction caused by Heubner's recurring artery occlusion". Brain Cogn. 61 (2): 133–8. doi:10.1016/j.bandc.2005.11.002. PMID 16510225.
- ↑ 12.0 12.1 Fridriksson J, Fillmore P, Guo D, Rorden C (2015). "Chronic Broca's Aphasia Is Caused by Damage to Broca's and Wernicke's Areas". Cereb Cortex. 25 (12): 4689–96. doi:10.1093/cercor/bhu152. PMC 4669036. PMID 25016386.
- ↑ 13.0 13.1 Henderson VW (1985). "Lesion localization in Broca's aphasia. Implications from Broca's aphasia without hemiparesis". Arch Neurol. 42 (12): 1210–2. PMID 4062622.
- ↑ 14.0 14.1 Soma Y (1997). "[Cerebrovascular disorder and the language areas]". Rinsho Shinkeigaku. 37 (12): 1117–9. PMID 9577663.
- ↑ Bang OY, Heo JH, Kim JY, Park JH, Huh K (2002). "Middle cerebral artery stenosis is a major clinical determinant in striatocapsular small, deep infarction". Arch Neurol. 59 (2): 259–63. PMID 11843697.
- ↑ Ghika J, Bogousslavsky J, Regli F (1991). "Infarcts in the territory of lenticulostriate branches from the middle cerebral artery. Etiological factors and clinical features in 65 cases". Schweiz Arch Neurol Psychiatr (1985). 142 (1): 5–18. PMID 1709298.
- ↑ Arboix A, Martí-Vilalta JL (2009). "Lacunar stroke". Expert Rev Neurother. 9 (2): 179–96. doi:10.1586/14737175.9.2.179. PMID 19210194.
- ↑ Melo TP, Bogousslavsky J, van Melle G, Regli F (1992). "Pure motor stroke: a reappraisal". Neurology. 42 (4): 789–95. PMID 1565233.
- ↑ Tei H, Uchiyama S, Maruyama S (1993). "Capsular infarcts: location, size and etiology of pure motor hemiparesis, sensorimotor stroke and ataxic hemiparesis". Acta Neurol Scand. 88 (4): 264–8. PMID 8256570.
- ↑ 20.0 20.1 Pessin MS, Lathi ES, Cohen MB, Kwan ES, Hedges TR, Caplan LR (1987). "Clinical features and mechanism of occipital infarction". Ann Neurol. 21 (3): 290–9. doi:10.1002/ana.410210311. PMID 3606035.
- ↑ 21.0 21.1 Fisher CM (1986). "The posterior cerebral artery syndrome". Can J Neurol Sci. 13 (3): 232–9. PMID 3742339.
- ↑ Damasio AR, Damasio H, Van Hoesen GW (1982). "Prosopagnosia: anatomic basis and behavioral mechanisms". Neurology. 32 (4): 331–41. PMID 7199655.
- ↑ 23.0 23.1 23.2 Caplan LR, Hedley-Whyte T (1974). "Cuing and memory dysfunction in alexia without agraphia. A case report". Brain. 97 (2): 251–62. PMID 4434176.
- ↑ 24.0 24.1 Geschwind N, Fusillo M (1966). "Color-naming defects in association with alexia". Arch Neurol. 15 (2): 137–46. PMID 5945970.
- ↑ 25.0 25.1 Melo TP, Bogousslavsky J (1992). "Hemiataxia-hypesthesia: a thalamic stroke syndrome". J Neurol Neurosurg Psychiatry. 55 (7): 581–4. PMC 489170. PMID 1640235.
- ↑ 26.0 26.1 26.2 Caplan L (2000). "Posterior circulation ischemia: then, now, and tomorrow. The Thomas Willis Lecture-2000". Stroke. 31 (8): 2011–23. PMID 10926972.
- ↑ Nouh A, Remke J, Ruland S (2014). "Ischemic posterior circulation stroke: a review of anatomy, clinical presentations, diagnosis, and current management". Front Neurol. 5: 30. doi:10.3389/fneur.2014.00030. PMC 3985033. PMID 24778625.
- ↑ Sacco RL, Freddo L, Bello JA, Odel JG, Onesti ST, Mohr JP (1993). "Wallenberg's lateral medullary syndrome. Clinical-magnetic resonance imaging correlations". Arch Neurol. 50 (6): 609–14. PMID 8503798.
- ↑ Shetty SR, Anusha R, Thomas PS, Babu SG (2012). "Wallenberg's syndrome". J Neurosci Rural Pract. 3 (1): 100–2. doi:10.4103/0976-3147.91980. PMC 3271596. PMID 22346215.
- ↑ Kim JS, Kim HG, Chung CS (1995). "Medial medullary syndrome. Report of 18 new patients and a review of the literature". Stroke. 26 (9): 1548–52. PMID 7660396.
- ↑ Kim K, Lee HS, Jung YH, Kim YD, Nam HS, Nam CM; et al. (2012). "Mechanism of medullary infarction based on arterial territory involvement". J Clin Neurol. 8 (2): 116–22. doi:10.3988/jcn.2012.8.2.116. PMC 3391616. PMID 22787495.
- ↑ Amarenco P, Hauw JJ (1989). "[Anatomy of the cerebellar arteries]". Rev Neurol (Paris). 145 (4): 267–76. PMID 2535662.