Hyperparathyroidism other imaging findings
|
Hyperparathyroidism Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Hyperparathyroidism other imaging findings On the Web |
|
American Roentgen Ray Society Images of Hyperparathyroidism other imaging findings |
|
Risk calculators and risk factors for Hyperparathyroidism other imaging findings |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief:
Overview
Imaging modalities may be helpful in preoperative localization of hyper-functioning parathyroid glands. This includes both non-invasive and invasive modalities. Non-invasive imaging modalities for preoperative localization of hyper-functioning parathyroid glands include Tc-99m sestamibi scintigraphy (sestamibi or MIBI), single positron emission computed tomography (SPECT), positron emission tomography (PET). Invasive modalities used for preoperative localization of hyper-functioning parathyroid glands include selective arteriography and angiography. Dual energy X-ray absorptiometry is helpful in detecting low bone mineral density caused by hyperparathyroidism.
Other Imaging Findings
Other imaging modalities are used for preoperative localization of hyper-functioning parathyroid glands. This includes both non-invasive and invasive modalities. Another modality used in hyperparathyroidism is dual energy X-ray absorptiomerty (DXA). DXA is helpful in detecting low bone mineral density caused by hyperparathyroidism.
Non-invasive modalities
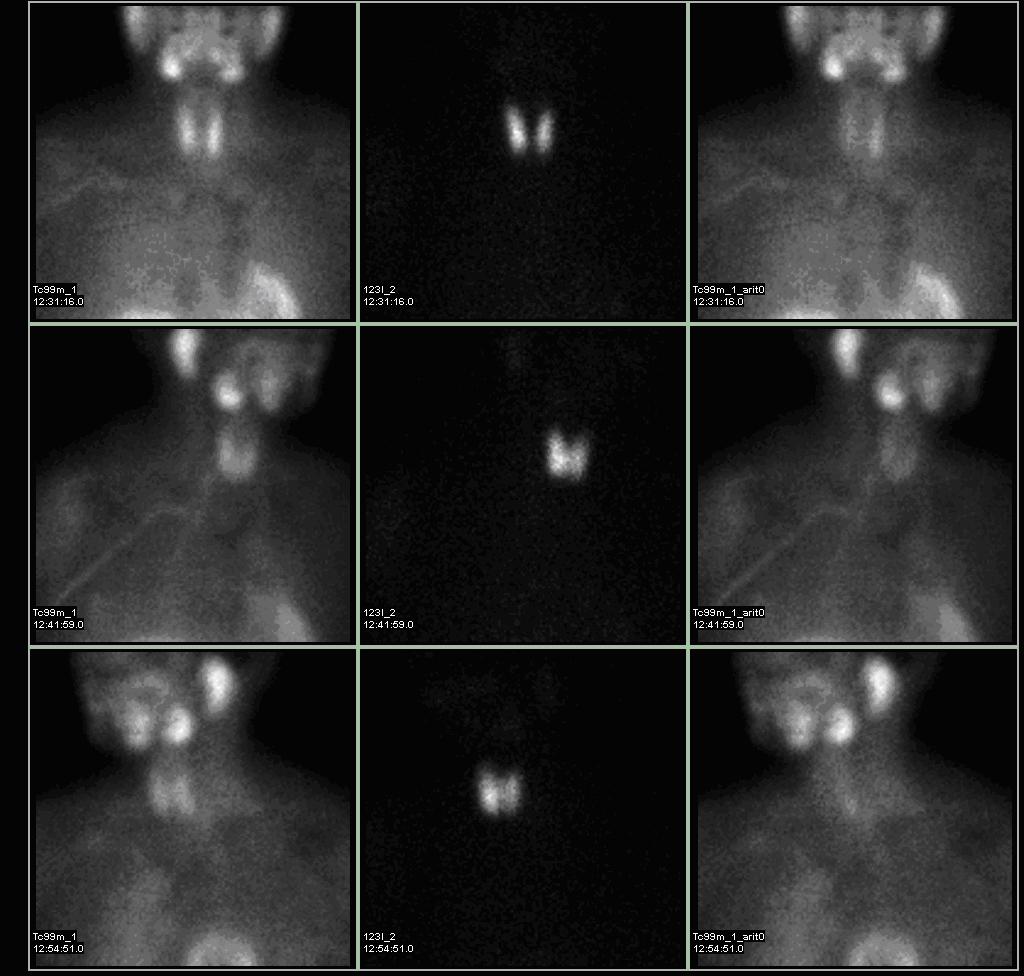
TC-99m Sestamibi Scintigraphy
- Technetium-99m-methoxyisobutylisonitrile (99mTc-sestamibi or MIBI) scintigraphy is the most popular investigation for preoperative localization of hyper-functioning parathyroid glands.[1]
- Most of the sestamibi is retained in mitochondria of thyroid and abnormal parathyroid tissue and is a function of mitochondrial activity.[2]
- The basis of this "single-isotope, double-phase technique" is that sestamibi washes out of the thyroid more rapidly than from abnormal parathyroid tissue.[3]
- Multiple planar images are obtained, typically one shortly after injection of 99mTc-sestamibi and another after two hours to identify the foci of retained sestamibi showing hyper-functioning parathyroid tissue.
- As all parathyroid lesions does not retain sestamibi nor all thyroid tissue washes out quickly, subtraction imaging may be beneficial.[4]
- Subtraction technique uses dual contrast Tc-99m sestamibi along with iodine-123 or 99m-technicium pertechnetate which is taken by thyroid tissue only. Iodine-123/99m-technicium pertechnetate images of thyroid are later digitally subtracted from Tc-99m sestamibi images leading to visualization of parathyroid tissue only.[5]
- Presence of solid thyroid nodule is the most common cause of false positive results. Other causes of false positive results may include thyroid carcinoma, lymphoma, and lymphadenopathy.
- The sensitivity of sestamibi scintigraphy can be increased by using it concomitantly with neck ultrasound and/or SPECT. [6][7]
- The sensitivity of sestamibi scintigraphy is 80% - 90%.[8][9][10]
 |
 |
Single positron emission computed tomography (SPECT)
- Single positron emission computed tomography may be used along with Tc-99m sestamibi scintigraphy for preoperative evaluation of hyper-functioning parathyroid gland.[11][12]
- Sestamibi-SPECT is also called pinhone-SPECT (P-SPECT). P-SPECT uses cone beam collimator in contrast to parallel-hole collimator used in SPECT. cone bean collimator possess more suitable geometric properties leading to high spatial resolution.[13][14]
- Using SPECT with sestamibi scintigraphy improves detection and localization of hyper-functioning parathyroid gland.[15][16]
- SPECT provides more precise result of sestamibi scitigraphy allowing surgeon to choose best route for surgical intervention.
- P-SPECT may detect glands not visible on planer images leading to increased sensitivity. It is very useful in case of uncertain result from conventional sestamibi scitigraphy.[17][18]
- P-SPECT also enables accurate interpretation sestamibi uptake in upper mediastinum leading to a higher specificity.
- In difficult cases, P-SPECT may also be adjuncted with subtraction Tc-99m sestamibi and I-123 scintigraphy or positron emission tomography.[19]
- P-SPECT is approximately 84% sensitive, 91% specific with positive predictive value of around 91% and negative predictive value of around 84%.[20]
- Fusion images of CT-MIBI-SPECT is superior to CT or MIBI-SPECT alone in preoperative localization of hyper-functioning parathyroid gland.[21]
Positron Emission Tomography (PET)
- 11C-methionine PET along with CT scan (MET-PET/CT) may be used for preoperative localization of hyper-functioning gland.[22][23]
- MET-PET/CT may be used as an complimentary imaging modality for localizing hyper-functioning parathyroid glands in patients with negative Tc-99m sestamibi scintigraphy/SPECT results.[24]
Invasive modalities
Selective arteriography
- Selective transarterial hypocalcemic stimulation is combined with nonselective venous sampling to perform selective arteriography.[25]
- Sodium citrate is injected to induce hypocalcemia. Simultaneous arteriography is performed.
- Samples are taken for superior vena cava at basaeline and timed intervals (20 sec, 40 sec, and 60 sec).
- An increase in the parathyroid hormone level to 1.4 times above the baseline or a clear blush observed on arteriography is considered as positive localization.
- Arterial stimulation venous sampling is performed simultaneously with arteriogram due to similarly high PPV.
Angiography
- Superselective arterial digital subtraction angiography (DSA) and superselective conventional angiography (CA) may be used for preoperative localization of hyper-functioning parathyroid glands in which noninvasive imaging modalities are negative or inconclusive.[26]
- Sensitivity of superselective digital subtraction angiography appears to be similar to conventional angiography.
- Superselective arterial digital subtraction angiography may be more sensitive than conventional angiography for preoperative localization of mediastinal hyper-functioning parathyroid glands.
References
- ↑ Palestro CJ, Tomas MB, Tronco GG (2005). "Radionuclide imaging of the parathyroid glands". Semin Nucl Med. 35 (4): 266–76. doi:10.1053/j.semnuclmed.2005.06.001. PMID 16150247.
- ↑ Hetrakul N, Civelek AC, Stagg CA, Udelsman R (2001). "In vitro accumulation of technetium-99m-sestamibi in human parathyroid mitochondria". Surgery. 130 (6): 1011–8. doi:10.1067/msy.2001.118371. PMID 11742331.
- ↑ Taillefer R, Boucher Y, Potvin C, Lambert R (1992). "Detection and localization of parathyroid adenomas in patients with hyperparathyroidism using a single radionuclide imaging procedure with technetium-99m-sestamibi (double-phase study)". J Nucl Med. 33 (10): 1801–7. PMID 1328564.
- ↑ Thulé P, Thakore K, Vansant J, McGarity W, Weber C, Phillips LS (1994). "Preoperative localization of parathyroid tissue with technetium-99m sestamibi 123I subtraction scanning". J Clin Endocrinol Metab. 78 (1): 77–82. doi:10.1210/jcem.78.1.8288719. PMID 8288719.
- ↑ Ryhänen EM, Schildt J, Heiskanen I, Väisänen M, Ahonen A, Löyttyniemi E; et al. (2015). "(99m)Technetium Sestamibi-(123)Iodine Scintigraphy Is More Accurate Than (99m)Technetium Sestamibi Alone before Surgery for Primary Hyperparathyroidism". Int J Mol Imaging. 2015: 391625. doi:10.1155/2015/391625. PMC 4333274. PMID 25722888.
- ↑ Eslamy HK, Ziessman HA (2008). "Parathyroid scintigraphy in patients with primary hyperparathyroidism: 99mTc sestamibi SPECT and SPECT/CT". Radiographics. 28 (5): 1461–76. doi:10.1148/rg.285075055. PMID 18794320.
- ↑ Haber RS, Kim CK, Inabnet WB (2002). "Ultrasonography for preoperative localization of enlarged parathyroid glands in primary hyperparathyroidism: comparison with (99m)technetium sestamibi scintigraphy". Clin Endocrinol (Oxf). 57 (2): 241–9. PMID 12153604.
- ↑ Chapuis Y, Fulla Y, Bonnichon P, Tarla E, Abboud B, Pitre J, Richard B (1996). "Values of ultrasonography, sestamibi scintigraphy, and intraoperative measurement of 1-84 PTH for unilateral neck exploration of primary hyperparathyroidism". World J Surg. 20 (7): 835–9, discussion 839–40. PMID 8678959.
- ↑ Prasannan S, Davies G, Bochner M, Kollias J, Malycha P (2007). "Minimally invasive parathyroidectomy using surgeon-performed ultrasound and sestamibi". ANZ J Surg. 77 (9): 774–7. doi:10.1111/j.1445-2197.2007.04227.x. PMID 17685957.
- ↑ Gómez-Ramírez J, Sancho-Insenser JJ, Pereira JA, Jimeno J, Munné A, Sitges-Serra A (2010). "Impact of thyroid nodular disease on 99mTc-sestamibi scintigraphy in patients with primary hyperparathyroidism". Langenbecks Arch Surg. 395 (7): 929–33. doi:10.1007/s00423-010-0680-8. PMID 20625763.
- ↑ Billotey C, Sarfati E, Aurengo A, Duet M, Mündler O, Toubert ME; et al. (1996). "Advantages of SPECT in technetium-99m-sestamibi parathyroid scintigraphy". J Nucl Med. 37 (11): 1773–8. PMID 8917173.
- ↑ Civelek AC, Ozalp E, Donovan P, Udelsman R (2002). "Prospective evaluation of delayed technetium-99m sestamibi SPECT scintigraphy for preoperative localization of primary hyperparathyroidism". Surgery. 131 (2): 149–57. PMID 11854692.
- ↑ Strand SE, Ivanovic M, Erlandsson K, Franceschi D, Button T, Sjögren K; et al. (1994). "Small animal imaging with pinhole single-photon emission computed tomography". Cancer. 73 (3 Suppl): 981–4. PMID 8306288.
- ↑ Jaszczak RJ, Li J, Wang H, Zalutsky MR, Coleman RE (1994). "Pinhole collimation for ultra-high-resolution, small-field-of-view SPECT". Phys Med Biol. 39 (3): 425–37. PMID 15551591.
- ↑ Schachter PP, Issa N, Shimonov M, Czerniak A, Lorberboym M (2004). "Early, postinjection MIBI-SPECT as the only preoperative localizing study for minimally invasive parathyroidectomy". Arch Surg. 139 (4): 433–7. doi:10.1001/archsurg.139.4.433. PMID 15078713.
- ↑ Perez-Monte JE, Brown ML, Shah AN, Ranger NT, Watson CG, Carty SE; et al. (1996). "Parathyroid adenomas: accurate detection and localization with Tc-99m sestamibi SPECT". Radiology. 201 (1): 85–91. doi:10.1148/radiology.201.1.8816526. PMID 8816526.
- ↑ Spanu A, Falchi A, Manca A, Marongiu P, Cossu A, Pisu N; et al. (2004). "The usefulness of neck pinhole SPECT as a complementary tool to planar scintigraphy in primary and secondary hyperparathyroidism". J Nucl Med. 45 (1): 40–8. PMID 14734671.
- ↑ Carlier T, Oudoux A, Mirallié E, Seret A, Daumy I, Leux C, Bodet-Milin C, Kraeber-Bodéré F, Ansquer C (2008). "99mTc-MIBI pinhole SPECT in primary hyperparathyroidism: comparison with conventional SPECT, planar scintigraphy and ultrasonography". Eur. J. Nucl. Med. Mol. Imaging. 35 (3): 637–43. doi:10.1007/s00259-007-0625-9. PMC 2964350. PMID 17960377.
- ↑ Nguyen BD (1999). "Parathyroid imaging with Tc-99m sestamibi planar and SPECT scintigraphy". Radiographics. 19 (3): 601–14, discussion 615-6. doi:10.1148/radiographics.19.3.g99ma10601. PMID 10336191.
- ↑ Lindqvist V, Jacobsson H, Chandanos E, Bäckdahl M, Kjellman M, Wallin G (2009). "Preoperative 99Tc(m)-sestamibi scintigraphy with SPECT localizes most pathologic parathyroid glands". Langenbecks Arch Surg. 394 (5): 811–5. doi:10.1007/s00423-009-0536-2. PMID 19578871.
- ↑ Wimmer G, Profanter C, Kovacs P, Sieb M, Gabriel M, Putzer D; et al. (2010). "CT-MIBI-SPECT image fusion predicts multiglandular disease in hyperparathyroidism". Langenbecks Arch Surg. 395 (1): 73–80. doi:10.1007/s00423-009-0545-1. PMID 19705144.
- ↑ Tang BN, Moreno-Reyes R, Blocklet D, Corvilain B, Cappello M, Delpierre I; et al. (2008). "Accurate pre-operative localization of pathological parathyroid glands using 11C-methionine PET/CT". Contrast Media Mol Imaging. 3 (4): 157–63. doi:10.1002/cmmi.243. PMID 18781582.
- ↑ Weber T, Maier-Funk C, Ohlhauser D, Hillenbrand A, Cammerer G, Barth TF; et al. (2013). "Accurate preoperative localization of parathyroid adenomas with C-11 methionine PET/CT". Ann Surg. 257 (6): 1124–8. doi:10.1097/SLA.0b013e318289b345. PMID 23478517.
- ↑ Traub-Weidinger T, Mayerhoefer ME, Koperek O, Mitterhauser M, Duan H, Karanikas G; et al. (2014). "11C-methionine PET/CT imaging of 99mTc-MIBI-SPECT/CT-negative patients with primary hyperparathyroidism and previous neck surgery". J Clin Endocrinol Metab. 99 (11): 4199–205. doi:10.1210/jc.2014-1267. PMID 25029418.
- ↑ Powell AC, Alexander HR, Chang R, Marx SJ, Skarulis M, Pingpank JF; et al. (2009). "Reoperation for parathyroid adenoma: a contemporary experience". Surgery. 146 (6): 1144–55. doi:10.1016/j.surg.2009.09.015. PMC 3467310. PMID 19958942.
- ↑ Miller DL, Chang R, Doppman JL, Norton JA (1989). "Localization of parathyroid adenomas: superselective arterial DSA versus superselective conventional angiography". Radiology. 170 (3 Pt 2): 1003–6. doi:10.1148/radiology.170.3.2644666. PMID 2644666.