Fungal meningitis laboratory findings: Difference between revisions
Prince Djan (talk | contribs) |
Prince Djan (talk | contribs) |
||
| Line 15: | Line 15: | ||
===Other CSF Findings and Serology Tests Specific to Each Particular Fungi=== | ===Other CSF Findings and Serology Tests Specific to Each Particular Fungi=== | ||
*''[[Aspergillus sp. | *''[[Aspergillus]] sp.'' | ||
**CSF culture may grow Aspergillus fumigatus complex or may be sterile<ref name="pmid26392507">{{cite journal| author=Morgand M, Rammaert B, Poirée S, Bougnoux ME, Tran H, Kania R et al.| title=Chronic Invasive Aspergillus Sinusitis and Otitis with Meningeal Extension Successfully Treated with Voriconazole. | journal=Antimicrob Agents Chemother | year= 2015 | volume= 59 | issue= 12 | pages= 7857-61 | pmid=26392507 | doi=10.1128/AAC.01506-15 | pmc=4649149 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26392507 }} </ref> | **CSF culture may grow Aspergillus fumigatus complex or may be sterile<ref name="pmid26392507">{{cite journal| author=Morgand M, Rammaert B, Poirée S, Bougnoux ME, Tran H, Kania R et al.| title=Chronic Invasive Aspergillus Sinusitis and Otitis with Meningeal Extension Successfully Treated with Voriconazole. | journal=Antimicrob Agents Chemother | year= 2015 | volume= 59 | issue= 12 | pages= 7857-61 | pmid=26392507 | doi=10.1128/AAC.01506-15 | pmc=4649149 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26392507 }} </ref> | ||
**Gomori-Grocott staining may reveale hyaline septate hyphae<ref name="pmid26392507">{{cite journal| author=Morgand M, Rammaert B, Poirée S, Bougnoux ME, Tran H, Kania R et al.| title=Chronic Invasive Aspergillus Sinusitis and Otitis with Meningeal Extension Successfully Treated with Voriconazole. | journal=Antimicrob Agents Chemother | year= 2015 | volume= 59 | issue= 12 | pages= 7857-61 | pmid=26392507 | doi=10.1128/AAC.01506-15 | pmc=4649149 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26392507 }} </ref> | **Gomori-Grocott staining may reveale hyaline septate hyphae<ref name="pmid26392507">{{cite journal| author=Morgand M, Rammaert B, Poirée S, Bougnoux ME, Tran H, Kania R et al.| title=Chronic Invasive Aspergillus Sinusitis and Otitis with Meningeal Extension Successfully Treated with Voriconazole. | journal=Antimicrob Agents Chemother | year= 2015 | volume= 59 | issue= 12 | pages= 7857-61 | pmid=26392507 | doi=10.1128/AAC.01506-15 | pmc=4649149 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26392507 }} </ref> | ||
Revision as of 16:14, 2 February 2017
|
Fungal meningitis Microchapters |
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Fungal meningitis laboratory findings On the Web |
|
American Roentgen Ray Society Images of Fungal meningitis laboratory findings |
|
Risk calculators and risk factors for Fungal meningitis laboratory findings |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Rim Halaby; Prince Tano Djan, BSc, MBChB [2]
Overview
A lumbar puncture is essential for the diagnosis of fungal meningitis and initiation of the appropriate treatment. The cerebrospinal fluid (CSF) of a patient having bacterial meningitis is distinguished by the presence of lymphocytosis, low glucose level and high proteins level. Specific CSF stains and cultures as well as serologies help in determining the specific nature of the causative fungi.
Biopsy of skin lesions, chest radiography, ophthalmologic examination, computed tomography or MRI of the brain, in addition to cultures of CSF, blood, and sputum, may provide essential diagnostic clues.
Laboratory Findings
The General Characteristic CSF Findings in Fungal Meningitis:
General characteristic CSF findings in fungal meningitis may show the following[1]
- Mononuclear or lymphocytic pleocytosis
- An elevated protein concentration
- A decreased glucose concentration
Other CSF Findings and Serology Tests Specific to Each Particular Fungi
- Aspergillus sp.
- CSF culture may grow Aspergillus fumigatus complex or may be sterile[2]
- Gomori-Grocott staining may reveale hyaline septate hyphae[2]
- Baseline serum and CSF 1,3-β-d-glucan (BDG) measurements are positive whereas serum and CSF galactomannan (GM) antigen test results are negative in an Aspergillus fumigatus-specific PCR assay.[2]
- Blastomyces dermatitidis
- Fungal stain and culture of CSF
- Biopsy and culture of skin and lung lesions
- Antibody detection in serum
- Cryptococcus neoformans
- India ink or fungal wet mount of CSF (budding yeast)
- Mucicarmine stain provides specific staining of the polysaccharide cell wall
- Blood and urine cultures
- Antigen detection in CSF
- Coccidioides immitis
- Antibody detection in CSF and serum
- Candida sp.
- Fungal stain and culture of CSF
- Histoplasma capsulatum
- Fungal stain and culture of large volumes of CSF
- Antigen detection in CSF, serum, and urine
- Antibody detection in serum and CSF
- Sporothrix schenckii
- Antibody detection in CSF and serum
- CSF culture[3]
Fungal Stains
-
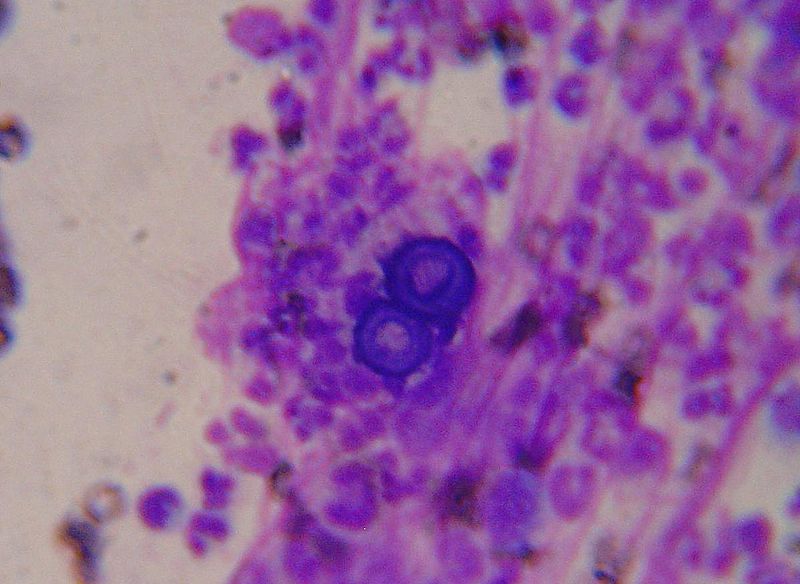
Blastomyces: Broad based budding
-
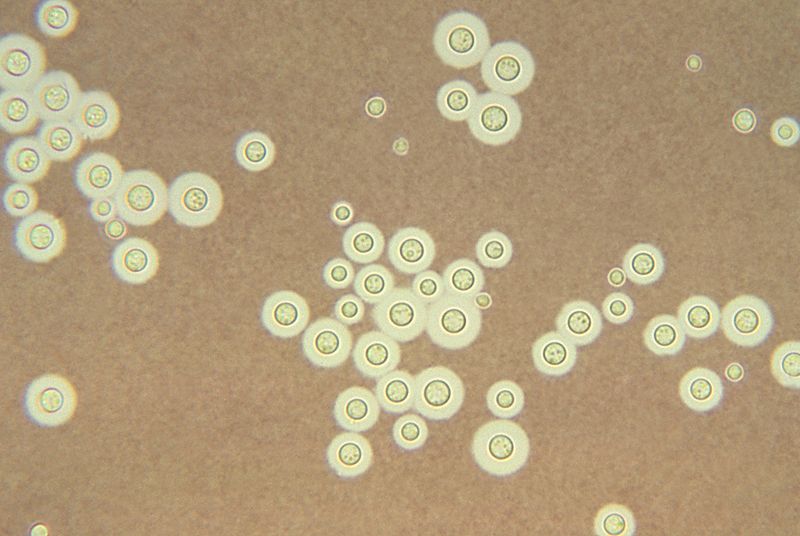
Cryptococcus: clear halo visualized by the india ink stain
-
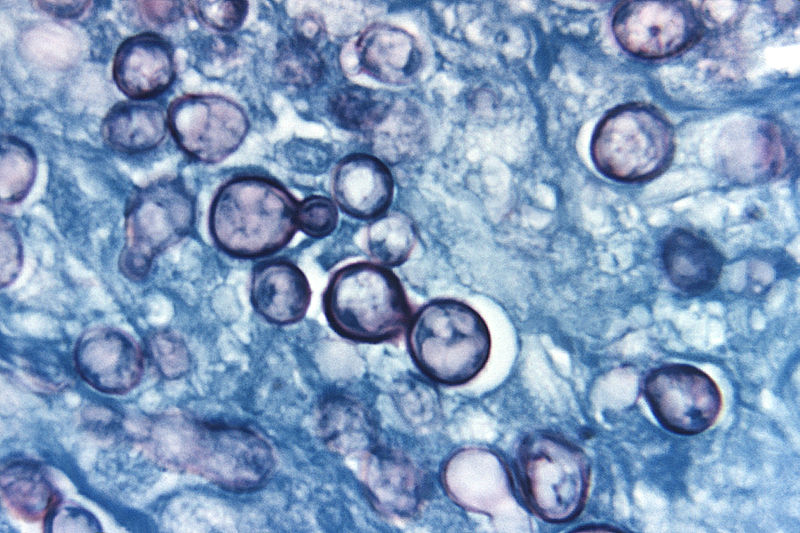
Histoplama capsulatum
References
- ↑ Banarer M, Cost K, Rychwalski P, Bryant KA (2005). "Chronic lymphocytic meningitis in an adolescent". J Pediatr. 147 (5): 686–90. doi:10.1016/j.jpeds.2005.07.010. PMID 16291364.
- ↑ 2.0 2.1 2.2 Morgand M, Rammaert B, Poirée S, Bougnoux ME, Tran H, Kania R; et al. (2015). "Chronic Invasive Aspergillus Sinusitis and Otitis with Meningeal Extension Successfully Treated with Voriconazole". Antimicrob Agents Chemother. 59 (12): 7857–61. doi:10.1128/AAC.01506-15. PMC 4649149. PMID 26392507.
- ↑ Koroshetz WJ. Chapter 382. Chronic and Recurrent Meningitis. In: Longo DL, Fauci AS, Kasper DL, Hauser SL, Jameson JL, Loscalzo J, eds. Harrison's Principles of Internal Medicine. 18th ed. New York: McGraw-Hill; 2012.