Fibroma CT: Difference between revisions
No edit summary |
|||
| (13 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Fibroma}} | {{Fibroma}} | ||
{{CMG}}; {{AE}} {{Simrat}} | {{CMG}}; {{AE}}{{M.N}}, {{Simrat}} | ||
==Overview== | ==Overview== | ||
CT scan may be helpful in the diagnosis of fibroma. Findings on | [[CT scan]] may be helpful in the [[diagnosis]] of fibroma. Findings on [[CT]] suggestive of a particular fibroma depends on the type of the fibroma. Findings on [[CT scan]] of [[ossifying fibroma]] include a well-circumscribed lesion, intracortical [[osteolysis]] with a characteristic sclerotic band, and moderate [[Cortical area|cortical]] expansion. Findings on [[CT scan]] of non- ossifying fibroma include sharply demarcated, asymmetrical, [[Cortical area|cortical]]<nowiki/>ly based lucencies with a thin sclerotic rim. Findings on [[CT scan]] of chondromyxoid fibroma include a mild cortical expansion and characteristic lack of mineralization within [[chondromyxoid fibroma]]. Findings on [[CT scan]] of [[cemento-ossifying fibroma]] include a well circumscribed masses which expand the underlying [[bone]]. | ||
==CT Findings== | ==CT Findings== | ||
===Ossifying Fibroma=== | ===Ossifying Fibroma=== | ||
Findings on CT scan of ossifying fibroma includes the following:<ref name="KawaguchiKato2018">{{cite journal|last1=Kawaguchi|first1=Masaya|last2=Kato|first2=Hiroki|last3=Miyazaki|first3=Tatsuhiko|last4=Kato|first4=Keizo|last5=Hatakeyama|first5=Daijiro|last6=Mizuta|first6=Keisuke|last7=Aoki|first7=Mitsuhiro|last8=Matsuo|first8=Masayuki|title=CT and MR imaging characteristics of histological subtypes of head and neck ossifying fibroma|journal=Dentomaxillofacial Radiology|volume=47|issue=6|year=2018|pages=20180085|issn=0250-832X|doi=10.1259/dmfr.20180085}}</ref><ref name="OwoshoHughes2015">{{cite journal|last1=Owosho|first1=Adepitan A.|last2=Hughes|first2=Marion A.|last3=Prasad|first3=Joanne L.|last4=Potluri|first4=Anitha|last5=Costello|first5=Bernard J.|last6=Branstetter|first6=Barton F.|title=Is Computed Tomography an Adequate Imaging Modality for the Evaluation of Juvenile Ossifying Fibroma? A Comparison of 2 Imaging Modalities (Computed Tomography and Magnetic Resonance Imaging)|journal=Journal of Oral and Maxillofacial Surgery|volume=73|issue=7|year=2015|pages=1304–1313|issn=02782391|doi=10.1016/j.joms.2015.01.013}}</ref><ref name="YangWang2012">{{cite journal|last1=Yang|first1=B.T.|last2=Wang|first2=Y.Z.|last3=Wang|first3=X.Y.|last4=Wang|first4=Z.C.|title=Imaging study of ossifying fibroma with associated aneurysmal bone cyst in the paranasal sinus|journal=European Journal of Radiology|volume=81|issue=11|year=2012|pages=3450–3455|issn=0720048X|doi=10.1016/j.ejrad.2012.05.010}}</ref> | Findings on [[CT scan]] of ossifying fibroma includes the following:<ref name="KawaguchiKato2018">{{cite journal|last1=Kawaguchi|first1=Masaya|last2=Kato|first2=Hiroki|last3=Miyazaki|first3=Tatsuhiko|last4=Kato|first4=Keizo|last5=Hatakeyama|first5=Daijiro|last6=Mizuta|first6=Keisuke|last7=Aoki|first7=Mitsuhiro|last8=Matsuo|first8=Masayuki|title=CT and MR imaging characteristics of histological subtypes of head and neck ossifying fibroma|journal=Dentomaxillofacial Radiology|volume=47|issue=6|year=2018|pages=20180085|issn=0250-832X|doi=10.1259/dmfr.20180085}}</ref><ref name="OwoshoHughes2015">{{cite journal|last1=Owosho|first1=Adepitan A.|last2=Hughes|first2=Marion A.|last3=Prasad|first3=Joanne L.|last4=Potluri|first4=Anitha|last5=Costello|first5=Bernard J.|last6=Branstetter|first6=Barton F.|title=Is Computed Tomography an Adequate Imaging Modality for the Evaluation of Juvenile Ossifying Fibroma? A Comparison of 2 Imaging Modalities (Computed Tomography and Magnetic Resonance Imaging)|journal=Journal of Oral and Maxillofacial Surgery|volume=73|issue=7|year=2015|pages=1304–1313|issn=02782391|doi=10.1016/j.joms.2015.01.013}}</ref><ref name="YangWang2012">{{cite journal|last1=Yang|first1=B.T.|last2=Wang|first2=Y.Z.|last3=Wang|first3=X.Y.|last4=Wang|first4=Z.C.|title=Imaging study of ossifying fibroma with associated aneurysmal bone cyst in the paranasal sinus|journal=European Journal of Radiology|volume=81|issue=11|year=2012|pages=3450–3455|issn=0720048X|doi=10.1016/j.ejrad.2012.05.010}}</ref> | ||
*Seen as a well-circumscribed lesion | *Seen as a well-circumscribed [[lesion]] | ||
*Demonstrates evidence of intracortical osteolysis with a characteristic sclerotic band ( | *Demonstrates evidence of intracortical [[osteolysis]] with a characteristic sclerotic band ([[osteoblast]]<nowiki/>ic rimming) | ||
*Moderate cortical expansion | *Moderate [[Cortical area|cortical]] expansion | ||
===Non-ossifying Fibroma=== | ===Non-ossifying Fibroma=== | ||
*Non-ossifying fibromas are typically sharply demarcated, asymmetrical, cortically based lucencies with a thin sclerotic rim.<ref name="Sabaté-LloberaNotta2015">{{cite journal|last1=Sabaté-Llobera|first1=A.|last2=Notta|first2=P.C.|last3=Pons-Escoda|first3=A.|last4=Puig-Calvo|first4=O.|last5=Martín-Comín|first5=J.|title=Scintigraphic depiction of non-ossifying fibromas and the role of SPECT/CT|journal=Revista Española de Medicina Nuclear e Imagen Molecular|volume=34|issue=3|year=2015|pages=181–184|issn=2253654X|doi=10.1016/j.remn.2014.10.004}}</ref> | *Non-ossifying fibromas are typically sharply demarcated, asymmetrical, [[Cortical area|cortically]] based lucencies with a thin sclerotic rim.<ref name="Sabaté-LloberaNotta2015">{{cite journal|last1=Sabaté-Llobera|first1=A.|last2=Notta|first2=P.C.|last3=Pons-Escoda|first3=A.|last4=Puig-Calvo|first4=O.|last5=Martín-Comín|first5=J.|title=Scintigraphic depiction of non-ossifying fibromas and the role of SPECT/CT|journal=Revista Española de Medicina Nuclear e Imagen Molecular|volume=34|issue=3|year=2015|pages=181–184|issn=2253654X|doi=10.1016/j.remn.2014.10.004}}</ref> | ||
*They often appear multiloculated. | *They often appear multiloculated. | ||
*They are located in the metaphysis | *They are located in the [[metaphysis]]. However, as the [[patient]] [[age]]<nowiki/>s, they seem to migrate away from the growth plate. | ||
*They have no associated periosteal reaction, cortical breach or associated soft tissue mass. | *They have no associated [[periosteal reaction]], [[Cortical area|cortical]] breach or associated [[soft tissue]] [[mass]]. | ||
===Ovarian Fibromas=== | ===Ovarian Fibromas=== | ||
* | *They usually manifest as [[diffuse]], slightly hypoattenuating masses with poor, very slow contrast enhancement. [[Calcification]] and bilaterality are both uncommon.<ref>{{Cite journal | ||
| author = [[Mariana Horta]] & [[Teresa Margarida Cunha]] | |||
| title = Sex cord-stromal tumors of the ovary: a comprehensive review and update for radiologists | |||
| journal = [[Diagnostic and interventional radiology (Ankara, Turkey)]] | |||
| volume = 21 | |||
| issue = 4 | |||
| pages = 277–286 | |||
| year = 2015 | |||
| month = July-August | |||
| doi = 10.5152/dir.2015.34414 | |||
| pmid = 26054417 | |||
}}</ref><ref>{{Cite journal | |||
| author = [[Meng-yu Liu]], [[Hua-dan Xue]] & [[Zheng-yu Jin]] | |||
| title = [CT findings of ovarian fibroma in 9 patients] | |||
| journal = [[Zhongguo yi xue ke xue yuan xue bao. Acta Academiae Medicinae Sinicae]] | |||
| volume = 34 | |||
| issue = 2 | |||
| pages = 104–108 | |||
| year = 2012 | |||
| month = April | |||
| doi = 10.3881/j.issn.1000-503X.2012.02.002 | |||
| pmid = 22776593 | |||
}}</ref><ref name="ZhangWu2014">{{cite journal|last1=Zhang|first1=Zhixu|last2=Wu|first2=Yan|last3=Gao|first3=Jianbo|title=CT Diagnosis in the Thecoma–Fibroma Group of the Ovarian Stromal Tumors|journal=Cell Biochemistry and Biophysics|volume=71|issue=2|year=2014|pages=937–943|issn=1085-9195|doi=10.1007/s12013-014-0288-7}}</ref> | |||
===Pleural Fibromas=== | ===Pleural Fibromas=== | ||
*Tends to have soft tissue attenuation on unenhanced scans and show relatively homogenous intense background enhancement on contrast enhanced scans.<ref name=" | *Tends to have [[soft tissue]] [[Attenuation (electromagnetic radiation)|attenuation]] on unenhanced scans and show relatively [[homogenous]] intense background enhancement on [[Contrast enhanced CT|contrast enhanced]] scans.<ref name="BickelhauptShah2015">{{cite journal|last1=Bickelhaupt|first1=S.|last2=Shah|first2=R.|last3=Schneider|first3=S.|last4=Wrazidlo|first4=W.|last5=Schlemmer|first5=H.|last6=Lederer|first6=W.|title=Computer- und magnetresonanztomografische Charakterisierung eines solitären fibrösen Tumors der Pleura|journal=RöFo - Fortschritte auf dem Gebiet der Röntgenstrahlen und der bildgebenden Verfahren|volume=187|issue=06|year=2015|pages=489–491|issn=1438-9029|doi=10.1055/s-0034-1385819}}</ref><ref name="MittalMittal2013">{{cite journal|last1=Mittal|first1=MaheshKumar|last2=Mittal|first2=Aliza|last3=Sinha|first3=Mukul|last4=Sureka|first4=Binit|last5=Thukral|first5=BrijBhushan|title=Radiological review of pleural tumors|journal=Indian Journal of Radiology and Imaging|volume=23|issue=4|year=2013|pages=313|issn=0971-3026|doi=10.4103/0971-3026.125577}}</ref><ref name="CardinaleArdissone2017">{{cite journal|last1=Cardinale|first1=Luciano|last2=Ardissone|first2=Francesco|last3=Garetto|first3=Irene|last4=Marci|first4=Valerio|last5=Volpicelli|first5=Giovanni|last6=Solitro|first6=Federica|last7=Fava|first7=Cesare|title=Imaging of benign solitary fibrous tumor of the pleura: a pictorial essay|journal=Rare Tumors|volume=2|issue=1|year=2017|pages=1–4|issn=2036-3613|doi=10.4081/rt.2010.e1}}</ref> | ||
*Non-enhancing areas may be present corresponding to necrosis, myxoid degeneration, or haemorrhage within the | *Non-enhancing areas may be present corresponding to [[necrosis]], myxoid [[degeneration]], or [[haemorrhage]] within the [[tumor]]. A pedicular attachment may also be seen. | ||
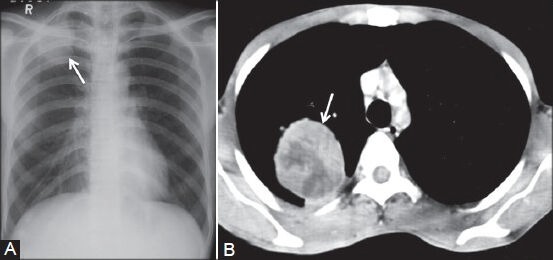
[[File:CT image of pleural fibroma.jpg|400px|thumb|none|Pleural fibroma: (A) Chest radiograph showing lobulated pleural-based opacity (arrow) in right apical region; (B) axial contrast-enhanced CT scan showing heterogeneously enhancing peripheral mass lesion (arrow) in a biopsy-proven case of benign pleural fibroma,Sureka B, Thukral BB, Mittal MK, Mittal A, Sinha M. Radiological review of pleural tumors. Indian J Radiol Imaging. 2013;23(4):313–320. doi:10.4103/0971-3026.125577,https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3932573/]] | |||
===Cardiac Fibromas=== | ===Cardiac Fibromas=== | ||
* | *On [[CT-scans|CT]], cardiac fibromas are [[homogeneous]] [[soft-tissue]] masses that are usually sharply marginated, but also can be infiltrative. [[Dystrophic calcification]] is common. | ||
===Chondromyxoid Fibroma=== | ===Chondromyxoid Fibroma=== | ||
*On computed tomography (CT), mild cortical expansion may be observed, and the lesions have a density greater than fluid throughout.<ref name=" | *On [[computed tomography]] (CT), mild [[Cortical area|cortical]] expansion may be observed, and the [[lesions]] have a density greater than fluid throughout.<ref name="TarhanYologlu2000">{{cite journal|last1=Tarhan|first1=N. C.|last2=Yologlu|first2=Z.|last3=Tutar|first3=N. U.|last4=Coskun|first4=M.|last5=Agildere|first5=A. M.|last6=Arikan|first6=U.|title=Chondromyxoid fibroma of the temporal bone: CT and MRI findings|journal=European Radiology|volume=10|issue=10|year=2000|pages=1678–1680|issn=0938-7994|doi=10.1007/s003300000323}}</ref><ref name="CappellePans2016">{{cite journal|last1=Cappelle|first1=Sarah|last2=Pans|first2=Steven|last3=Sciot|first3=Raf|title=Imaging features of chondromyxoid fibroma: report of 15 cases and literature review|journal=The British Journal of Radiology|volume=89|issue=1064|year=2016|pages=20160088|issn=0007-1285|doi=10.1259/bjr.20160088}}</ref><ref name="ShenChen2017">{{cite journal|last1=Shen|first1=Shuai|last2=Chen|first2=Miao|last3=Jug|first3=Rachel|last4=Yu|first4=Cheng-Qian|last5=Zhang|first5=Wan-Lin|last6=Yang|first6=Lian-He|last7=Wang|first7=Liang|last8=Yu|first8=Juan-Han|last9=Lin|first9=Xu-Yong|last10=Xu|first10=Hong-Tao|last11=Ma|first11=Shuang|title=Radiological presentation of chondromyxoid fibroma in the sellar region|journal=Medicine|volume=96|issue=49|year=2017|pages=e9049|issn=0025-7974|doi=10.1097/MD.0000000000009049}}</ref> | ||
*CT scans also exhibit characteristic lack of mineralization within chondromyxoid fibromas. | *[[CT scans]] also exhibit characteristic lack of [[mineralization]] within chondromyxoid fibromas. | ||
===Cemento-ossifying Fibroma=== | ===Cemento-ossifying Fibroma=== | ||
*Cemento-ossifying fibromas are usually well circumscribed masses which expand the underlying bone. | *Cemento-ossifying fibromas are usually well circumscribed masses which expand the underlying [[bone]]. | ||
*They are usually small, but can become large. This is particularly the case when they arise from the maxilla or paranasal sinuses because there is more room to expand. | *They are usually small, but can become large. This is particularly the case when they arise from the [[maxilla]] or [[paranasal sinuses]] because there is more room to expand. | ||
* | *As they mature, they gradually develop increasing amounts of [[calcification]]/[[ossification]] as they mature. | ||
*They usually expand the bone without cortical breach. | *They usually expand the [[bone]] without [[Cortical area|cortical]] breach. | ||
*Following administration of contrast, the soft tissue component usually enhances on CT. | *Following administration of contrast, the [[soft tissue]] component usually enhances on [[CT-scans|CT]]. | ||
===Uterine Fibroma=== | ===Uterine Fibroma=== | ||
*On CT scans, fibromas are usually of soft tissue density but may exhibit coarse peripheral or central calcification. | *On [[CT scans]], fibromas are usually of [[soft tissue]] density but may exhibit coarse peripheral or central [[calcification]].<ref name="OhgiyaSeino2017">{{cite journal|last1=Ohgiya|first1=Yoshimitsu|last2=Seino|first2=Noritaka|last3=Miyamoto|first3=Shingo|last4=Takeyama|first4=Nobuyuki|last5=Hatano|first5=Kumi|last6=Munechika|first6=Jiro|last7=Ishizuka|first7=Kumiko|last8=Hirose|first8=Masanori|last9=Ohike|first9=Nobuyuki|last10=Hashimoto|first10=Toshi|last11=Sekizawa|first11=Akihiko|last12=Gokan|first12=Takehiko|title=CT features for diagnosing acute torsion of uterine subserosal leiomyoma|journal=Japanese Journal of Radiology|volume=36|issue=3|year=2017|pages=209–214|issn=1867-1071|doi=10.1007/s11604-017-0712-1}}</ref><ref name="RoyBierry2004">{{cite journal|last1=Roy|first1=C.|last2=Bierry|first2=G.|last3=Ghali|first3=S. El|last4=Buy|first4=X.|last5=Rossini|first5=A.|title=Acute torsion of uterine leiomyoma: CT features|journal=Abdominal Imaging|volume=30|issue=1|year=2004|pages=120–123|issn=0942-8925|doi=10.1007/s00261-004-0240-1}}</ref> | ||
*They may distort the usually smooth uterine contour | |||
*They may distort the usually smooth [[uterine]] contour | |||
*Enhancement pattern is variable | *Enhancement pattern is variable | ||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
| Line 50: | Line 80: | ||
[[Category:Oncology]] | [[Category:Oncology]] | ||
[[Category:Types of cancer]] | [[Category:Types of cancer]] | ||
[[Category:Up-To-Date]] | |||
[[Category:Medicine]] | [[Category:Medicine]] | ||
[[Category:Radiology]] | |||
Latest revision as of 17:35, 9 July 2019
|
Fibroma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Fibroma CT On the Web |
|
American Roentgen Ray Society Images of Fibroma CT |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Maneesha Nandimandalam, M.B.B.S.[2], Simrat Sarai, M.D. [3]
Overview
CT scan may be helpful in the diagnosis of fibroma. Findings on CT suggestive of a particular fibroma depends on the type of the fibroma. Findings on CT scan of ossifying fibroma include a well-circumscribed lesion, intracortical osteolysis with a characteristic sclerotic band, and moderate cortical expansion. Findings on CT scan of non- ossifying fibroma include sharply demarcated, asymmetrical, cortically based lucencies with a thin sclerotic rim. Findings on CT scan of chondromyxoid fibroma include a mild cortical expansion and characteristic lack of mineralization within chondromyxoid fibroma. Findings on CT scan of cemento-ossifying fibroma include a well circumscribed masses which expand the underlying bone.
CT Findings
Ossifying Fibroma
Findings on CT scan of ossifying fibroma includes the following:[1][2][3]
- Seen as a well-circumscribed lesion
- Demonstrates evidence of intracortical osteolysis with a characteristic sclerotic band (osteoblastic rimming)
- Moderate cortical expansion
Non-ossifying Fibroma
- Non-ossifying fibromas are typically sharply demarcated, asymmetrical, cortically based lucencies with a thin sclerotic rim.[4]
- They often appear multiloculated.
- They are located in the metaphysis. However, as the patient ages, they seem to migrate away from the growth plate.
- They have no associated periosteal reaction, cortical breach or associated soft tissue mass.
Ovarian Fibromas
- They usually manifest as diffuse, slightly hypoattenuating masses with poor, very slow contrast enhancement. Calcification and bilaterality are both uncommon.[5][6][7]
Pleural Fibromas
- Tends to have soft tissue attenuation on unenhanced scans and show relatively homogenous intense background enhancement on contrast enhanced scans.[8][9][10]
- Non-enhancing areas may be present corresponding to necrosis, myxoid degeneration, or haemorrhage within the tumor. A pedicular attachment may also be seen.
Cardiac Fibromas
- On CT, cardiac fibromas are homogeneous soft-tissue masses that are usually sharply marginated, but also can be infiltrative. Dystrophic calcification is common.
Chondromyxoid Fibroma
- On computed tomography (CT), mild cortical expansion may be observed, and the lesions have a density greater than fluid throughout.[11][12][13]
- CT scans also exhibit characteristic lack of mineralization within chondromyxoid fibromas.
Cemento-ossifying Fibroma
- Cemento-ossifying fibromas are usually well circumscribed masses which expand the underlying bone.
- They are usually small, but can become large. This is particularly the case when they arise from the maxilla or paranasal sinuses because there is more room to expand.
- As they mature, they gradually develop increasing amounts of calcification/ossification as they mature.
- They usually expand the bone without cortical breach.
- Following administration of contrast, the soft tissue component usually enhances on CT.
Uterine Fibroma
- On CT scans, fibromas are usually of soft tissue density but may exhibit coarse peripheral or central calcification.[14][15]
- They may distort the usually smooth uterine contour
- Enhancement pattern is variable
References
- ↑ Kawaguchi, Masaya; Kato, Hiroki; Miyazaki, Tatsuhiko; Kato, Keizo; Hatakeyama, Daijiro; Mizuta, Keisuke; Aoki, Mitsuhiro; Matsuo, Masayuki (2018). "CT and MR imaging characteristics of histological subtypes of head and neck ossifying fibroma". Dentomaxillofacial Radiology. 47 (6): 20180085. doi:10.1259/dmfr.20180085. ISSN 0250-832X.
- ↑ Owosho, Adepitan A.; Hughes, Marion A.; Prasad, Joanne L.; Potluri, Anitha; Costello, Bernard J.; Branstetter, Barton F. (2015). "Is Computed Tomography an Adequate Imaging Modality for the Evaluation of Juvenile Ossifying Fibroma? A Comparison of 2 Imaging Modalities (Computed Tomography and Magnetic Resonance Imaging)". Journal of Oral and Maxillofacial Surgery. 73 (7): 1304–1313. doi:10.1016/j.joms.2015.01.013. ISSN 0278-2391.
- ↑ Yang, B.T.; Wang, Y.Z.; Wang, X.Y.; Wang, Z.C. (2012). "Imaging study of ossifying fibroma with associated aneurysmal bone cyst in the paranasal sinus". European Journal of Radiology. 81 (11): 3450–3455. doi:10.1016/j.ejrad.2012.05.010. ISSN 0720-048X.
- ↑ Sabaté-Llobera, A.; Notta, P.C.; Pons-Escoda, A.; Puig-Calvo, O.; Martín-Comín, J. (2015). "Scintigraphic depiction of non-ossifying fibromas and the role of SPECT/CT". Revista Española de Medicina Nuclear e Imagen Molecular. 34 (3): 181–184. doi:10.1016/j.remn.2014.10.004. ISSN 2253-654X.
- ↑ Mariana Horta & Teresa Margarida Cunha (2015). "Sex cord-stromal tumors of the ovary: a comprehensive review and update for radiologists". Diagnostic and interventional radiology (Ankara, Turkey). 21 (4): 277–286. doi:10.5152/dir.2015.34414. PMID 26054417. Unknown parameter
|month=ignored (help) - ↑ Meng-yu Liu, Hua-dan Xue & Zheng-yu Jin (2012). "[CT findings of ovarian fibroma in 9 patients]". Zhongguo yi xue ke xue yuan xue bao. Acta Academiae Medicinae Sinicae. 34 (2): 104–108. doi:10.3881/j.issn.1000-503X.2012.02.002. PMID 22776593. Unknown parameter
|month=ignored (help) - ↑ Zhang, Zhixu; Wu, Yan; Gao, Jianbo (2014). "CT Diagnosis in the Thecoma–Fibroma Group of the Ovarian Stromal Tumors". Cell Biochemistry and Biophysics. 71 (2): 937–943. doi:10.1007/s12013-014-0288-7. ISSN 1085-9195.
- ↑ Bickelhaupt, S.; Shah, R.; Schneider, S.; Wrazidlo, W.; Schlemmer, H.; Lederer, W. (2015). "Computer- und magnetresonanztomografische Charakterisierung eines solitären fibrösen Tumors der Pleura". RöFo - Fortschritte auf dem Gebiet der Röntgenstrahlen und der bildgebenden Verfahren. 187 (06): 489–491. doi:10.1055/s-0034-1385819. ISSN 1438-9029.
- ↑ Mittal, MaheshKumar; Mittal, Aliza; Sinha, Mukul; Sureka, Binit; Thukral, BrijBhushan (2013). "Radiological review of pleural tumors". Indian Journal of Radiology and Imaging. 23 (4): 313. doi:10.4103/0971-3026.125577. ISSN 0971-3026.
- ↑ Cardinale, Luciano; Ardissone, Francesco; Garetto, Irene; Marci, Valerio; Volpicelli, Giovanni; Solitro, Federica; Fava, Cesare (2017). "Imaging of benign solitary fibrous tumor of the pleura: a pictorial essay". Rare Tumors. 2 (1): 1–4. doi:10.4081/rt.2010.e1. ISSN 2036-3613.
- ↑ Tarhan, N. C.; Yologlu, Z.; Tutar, N. U.; Coskun, M.; Agildere, A. M.; Arikan, U. (2000). "Chondromyxoid fibroma of the temporal bone: CT and MRI findings". European Radiology. 10 (10): 1678–1680. doi:10.1007/s003300000323. ISSN 0938-7994.
- ↑ Cappelle, Sarah; Pans, Steven; Sciot, Raf (2016). "Imaging features of chondromyxoid fibroma: report of 15 cases and literature review". The British Journal of Radiology. 89 (1064): 20160088. doi:10.1259/bjr.20160088. ISSN 0007-1285.
- ↑ Shen, Shuai; Chen, Miao; Jug, Rachel; Yu, Cheng-Qian; Zhang, Wan-Lin; Yang, Lian-He; Wang, Liang; Yu, Juan-Han; Lin, Xu-Yong; Xu, Hong-Tao; Ma, Shuang (2017). "Radiological presentation of chondromyxoid fibroma in the sellar region". Medicine. 96 (49): e9049. doi:10.1097/MD.0000000000009049. ISSN 0025-7974.
- ↑ Ohgiya, Yoshimitsu; Seino, Noritaka; Miyamoto, Shingo; Takeyama, Nobuyuki; Hatano, Kumi; Munechika, Jiro; Ishizuka, Kumiko; Hirose, Masanori; Ohike, Nobuyuki; Hashimoto, Toshi; Sekizawa, Akihiko; Gokan, Takehiko (2017). "CT features for diagnosing acute torsion of uterine subserosal leiomyoma". Japanese Journal of Radiology. 36 (3): 209–214. doi:10.1007/s11604-017-0712-1. ISSN 1867-1071.
- ↑ Roy, C.; Bierry, G.; Ghali, S. El; Buy, X.; Rossini, A. (2004). "Acute torsion of uterine leiomyoma: CT features". Abdominal Imaging. 30 (1): 120–123. doi:10.1007/s00261-004-0240-1. ISSN 0942-8925.