Extranodal NK-T-cell lymphoma pathophysiology: Difference between revisions
No edit summary |
|||
| (29 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Extranodal NK-T-cell lymphoma}} | {{Extranodal NK-T-cell lymphoma}} | ||
{{CMG}}; {{AE}} {{ | {{CMG}}; {{AE}} {{RG}} | ||
==Overview== | ==Overview== | ||
== | |||
[[Natural killer cell|NK cells]] are [[CD3]] and [[myloperoxidase]] negative on their surface. [[Natural killer cell|NK cell]]<nowiki/>s have [[germline]] configuration of T-cell receptor and immunoglobulin genes. [[NK cells]] originate from a bipotent NK/T-progenitor cell so they have a lot in common with T cells. [[NK cells]] express T-associate markers such as [[CD2]], [[CD3]]<nowiki/>e, [[CD7]], [[CD8]], [[CD16]], [[CD56]], [[CD57]]. Most tumors involve NK cells but also involve T cells as neoplastic cells, that is the main reason of classification as NK/T-cell lymphoma rather than NK-cell [[lymphoma]]. the immunophenotype of NK lymphoma cells is classically positive for [[CD2]], [[CD56]], and cytoplasmic [[CD3]] epsilon. they are negative for surface [[CD3]]. Unlike normal NK cells, the tumor cells are usually negative for [[CD7]] and [[CD16]]. they express cytotoxic granule associated proteins [[granzyme B]], T-cell restricted intracellular antigen (TIA-1), and [[perforin]]. [[Extranodal NK-T-cell lymphoma|NK/T cell lymphoma]] expressing [[CD56]] is rare but most commonly occurs int he head and neck region, skin, and soft tissue. genes involved in the pathogenesis of [[extranodal NK-T-cell lymphoma]] include.:[[HLA-DQ|HLA DQA1*0501]], [[HLA-DQ|HLA DQB1*0201]]. these genes also are relevant with [[celiac disease]].On gross pathology, angiocentric and angiodestructive pattern of growth with associated geographical [[necrosis]] and [[ulceration]] are characteristic findings of [[extranodal NK-T-cell lymphoma]].[[Coagulative necrosis]] and [[apoptotic]] bodies are frequently encountered., [[Extranodal NK/T-cell lymphoma]], nasal type occurs in nasal cavity and upper aerodigestive tract., [[Extranodal NK-T-cell lymphoma|Extranodal NK/T cell lymphoma]], nasal type affects the nose and facial mid line exhibiting aggressive destruction., on microscopic histopathological analysis, medium sized tumor cells and polymorphic infiltrate of non-neoplastic inflammatory cells are characteristic findings of [[extranodal NK-T-cell lymphoma]]. the tumor cells are small to medium in size with occasional large and anaplastic forms. the lymphoma cells may be admixed with a polymorphic infiltrate of nonneoplastic [[Inflammation|inflammatory]] cells including small [[lymphocytes]], [[plasma cells]], [[histiocytes]], and [[eosinophils]]. | |||
==Pathophysiology== | |||
=== Physiology === | |||
* NK cells are [[CD3]] and [[myloperoxidase]] negative on their surface.<ref name="HamKo2010">{{cite journal|last1=Ham|first1=Maria Francisca|last2=Ko|first2=Young-Hyeh|title=Natural killer cell neoplasm: biology and pathology|journal=International Journal of Hematology|volume=92|issue=5|year=2010|pages=681–689|issn=0925-5710|doi=10.1007/s12185-010-0738-y}}</ref> | |||
* NK cells have [[germline]] configuration of T-cell receptor and immunoglobulin genes.<ref name="Canadian cancer">Extranodal NK/T-cell lymphoma, nasal type. Canadian Cancer Society. http://www.cancer.ca/en/cancer-information/cancer-type/non-hodgkin-lymphoma/non-hodgkin-lymphoma/types-of-nhl/extranodal-nk-t-cell-lymphoma-nasal-type/?region=on. Accessed on February 19, 2016 </ref> | |||
*NK cells originate from a bipotent NK/T-progenitor cell so they have a lot in common with T cells.<ref name="Hindawi">Extranodal Natural-Killer/T-Cell Lymphoma, Nasal Type. Hindawi Publishing Corporation. http://www.hindawi.com/journals/ah/2010/627401/. Accessed on February 18, 2016 </ref> | |||
*<nowiki/><nowiki/><nowiki/>NK cells express T-associate markers such as [[CD2]], [[CD3]]<nowiki/>e, [[CD7]], [[CD8]], [[CD16]], [[CD56]], [[CD57]].<ref name="pmid17492716">{{cite journal| author=Stewart CA, Walzer T, Robbins SH, Malissen B, Vivier E, Prinz I| title=Germ-line and rearranged Tcrd transcription distinguish bona fide NK cells and NK-like gammadelta T cells. | journal=Eur J Immunol | year= 2007 | volume= 37 | issue= 6 | pages= 1442-52 | pmid=17492716 | doi=10.1002/eji.200737354 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17492716 }}</ref> | |||
*<nowiki/>Most tumors involve NK cells but also involve T cells<nowiki/> as neoplastic cells, that is the main reason of classification as NK/T-cell lymphoma rather than NK-cell [[lymphoma]].<ref name="pmid23281437">{{cite journal |vauthors=Jaffe ES, Nicolae A, Pittaluga S |title=Peripheral T-cell and NK-cell lymphomas in the WHO classification: pearls and pitfalls |journal=Mod. Pathol. |volume=26 Suppl 1 |issue= |pages=S71–87 |date=January 2013 |pmid=23281437 |pmc=6324567 |doi=10.1038/modpathol.2012.181 |url=}}</ref> <nowiki/> | |||
* | |||
===Immunotype=== | ===Immunotype=== | ||
* The immunophenotype of NK lymphoma cells is classically positive for [[CD2]], [[CD56]], and cytoplasmic [[CD3]] epsilon. | * The immunophenotype of NK lymphoma cells is classically positive for [[CD2]], [[CD56]], and cytoplasmic [[CD3]] epsilon.<ref name="KoCho2004">{{cite journal|last1=Ko|first1=Y H|last2=Cho|first2=E-Y|last3=Kim|first3=J-E|last4=Lee|first4=S-S|last5=Huh|first5=J-R|last6=Chang|first6=H-K|last7=Yang|first7=W-I|last8=Kim|first8=C-W|last9=Kim|first9=S-W|last10=Ree|first10=H J|title=NK and NK-like T-cell lymphoma in extranasal sites: a comparative clinicopathological study according to site and EBV status|journal=Histopathology|volume=44|issue=5|year=2004|pages=480–489|issn=0309-0167|doi=10.1111/j.1365-2559.2004.01867.x}}</ref> | ||
* They are negative for surface [[CD3]]. Unlike normal NK cells, the tumor cells are usually negative for [[CD7]] and [[CD16]]. | * They are negative for surface [[CD3]]. Unlike normal NK cells, the tumor cells are usually negative for [[CD7]] and [[CD16]]. | ||
* They express cytotoxic granule associated proteins [[granzyme B]], T-cell restricted intracellular antigen (TIA-1), and [[perforin]]. | * They express cytotoxic granule associated proteins [[granzyme B]], T-cell restricted intracellular antigen (TIA-1), and [[perforin]]. | ||
*NK/T cell lymphoma expressing [[CD56]] is rare but most commonly occurs int he head and neck region, skin, and soft tissue. | |||
==Genetics== | |||
Genes involved in the pathogenesis of [[extranodal NK-T-cell lymphoma]] include.<ref name="ISBN9789283244943">{{cite book|last=Swerdlow|first=Steven|title=WHO classification of tumours of haematopoietic and lymphoid tissues|publisher=International Agency for Research on Cancer|location=Lyon|year=2017|isbn=9789283244943}}</ref>: | |||
*[[HLA-DQ|HLA DQA1*0501]] | |||
*[[HLA-DQ|HLA DQB1*0201]] | |||
These genes also are relevant with [[celiac disease]]. | |||
==Gross Pathology== | ==Gross Pathology== | ||
* On gross pathology, angiocentric and angiodestructive pattern of growth with associated geographical [[necrosis]] and [[ulceration]] are characteristic findings of extranodal NK-T-cell lymphoma. | * On gross pathology, angiocentric and angiodestructive pattern of growth with associated geographical [[necrosis]] and [[ulceration]] are characteristic findings of [[extranodal NK-T-cell lymphoma]].<ref name="KoCho20042">{{cite journal|last1=Ko|first1=Y H|last2=Cho|first2=E-Y|last3=Kim|first3=J-E|last4=Lee|first4=S-S|last5=Huh|first5=J-R|last6=Chang|first6=H-K|last7=Yang|first7=W-I|last8=Kim|first8=C-W|last9=Kim|first9=S-W|last10=Ree|first10=H J|title=NK and NK-like T-cell lymphoma in extranasal sites: a comparative clinicopathological study according to site and EBV status|journal=Histopathology|volume=44|issue=5|year=2004|pages=480–489|issn=0309-0167|doi=10.1111/j.1365-2559.2004.01867.x}}</ref> | ||
* [[Coagulative necrosis]] and [[apoptotic]] bodies are frequently encountered. | * [[Coagulative necrosis]] and [[apoptotic]] bodies are frequently encountered. | ||
*[[Extranodal NK/T-cell lymphoma]], nasal type occurs in nasal cavity and upper aerodigestive tract. | |||
*[[Extranodal NK-T-cell lymphoma|Extranodal NK/T cell lymphoma]], nasal type affects the nose and facial mid line exhibiting aggressive destruction. | |||
[[File:PMC4702053 CTO-14-04-g-007.png|center|250px|thumbnail|Adopted from OPEN-I. Nasal extranodal natural killer cell/T cell lymphoma with destruction of the midline<ref name="urlGMS | GMS Current Topics in Otorhinolaryngology - Head and Neck Surgery | Orphan diseases of the nose and paranasal sinuses: Pathogenesis – clinic – therapy">{{cite web |url=https://www.egms.de/static/en/journals/cto/2015-14/cto000119.shtml |title=GMS | GMS Current Topics in Otorhinolaryngology - Head and Neck Surgery | Orphan diseases of the nose and paranasal sinuses: Pathogenesis – clinic – therapy |format= |work= |accessdate=}}</ref>]] | |||
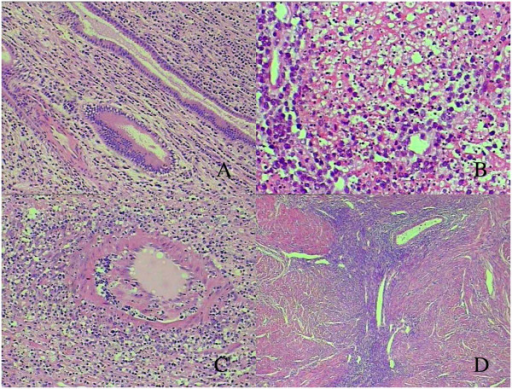
==Microscopic Pathology== | ==Microscopic Pathology== | ||
* On microscopic histopathological analysis, medium sized tumor cells and polymorphic infiltrate of non-neoplastic inflammatory cells are characteristic findings of extranodal NK-T-cell lymphoma. | * On microscopic histopathological analysis, medium sized tumor cells and polymorphic infiltrate of non-neoplastic inflammatory cells are characteristic findings of extranodal NK-T-cell lymphoma.<ref name="LiuTsai2018">{{cite journal|last1=Liu|first1=Chih-Yi|last2=Tsai|first2=Hui-Chih|title=Comparison of Diagnostic Cytomorphology of Natural Killer/T-Cell Lymphoma (Nasal Type) in Conventional Smears, Liquid-Based Preparations, and Histopathology|journal=Case Reports in Pathology|volume=2018|year=2018|pages=1–7|issn=2090-6781|doi=10.1155/2018/6264810}}</ref> | ||
* The tumor cells are small to medium in size with occasional large and anaplastic forms. | * The tumor cells are small to medium in size with occasional large and anaplastic forms. | ||
* The lymphoma cells may be admixed with a polymorphic infiltrate of nonneoplastic inflammatory cells including small [[lymphocytes]], [[plasma cells]], [[histiocytes]], and [[eosinophils]]. | * The lymphoma cells may be admixed with a polymorphic infiltrate of nonneoplastic inflammatory cells including small [[lymphocytes]], [[plasma cells]], [[histiocytes]], and [[eosinophils]]. | ||
[[File:PMC4052815 1746-1596-9-95-2.png|center|250ptx|thumbnail|Primary extranodal NK/T cell lymphoma, nasal-type<ref name="FangZhou2014">{{cite journal|last1=Fang|first1=Jian-chen|last2=Zhou|first2=Jue|last3=Li|first3=Zheng|last4=Xia|first4=Zhao-xia|title=Primary extranodal NK/T cell lymphoma, nasal-type of uterus with adenomyosis: a case report|journal=Diagnostic Pathology|volume=9|issue=1|year=2014|issn=1746-1596|doi=10.1186/1746-1596-9-95}}</ref>]] | |||
==References== | ==References== | ||
| Line 28: | Line 48: | ||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
[[Category:Up-To-Date]] | |||
[[Category:Oncology]] | |||
[[Category:Medicine]] | |||
[[Category:Hematology]] | |||
[[Category:Immunology]] | |||
Latest revision as of 18:59, 24 October 2019
|
Extranodal NK-T-cell lymphoma Microchapters |
|
Differentiating Extranodal NK-T-cell lymphoma from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Extranodal NK-T-cell lymphoma pathophysiology On the Web |
|
American Roentgen Ray Society Images of Extranodal NK-T-cell lymphoma pathophysiology |
|
Risk calculators and risk factors for Extranodal NK-T-cell lymphoma pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Ramyar Ghandriz MD[2]
Overview
NK cells are CD3 and myloperoxidase negative on their surface. NK cells have germline configuration of T-cell receptor and immunoglobulin genes. NK cells originate from a bipotent NK/T-progenitor cell so they have a lot in common with T cells. NK cells express T-associate markers such as CD2, CD3e, CD7, CD8, CD16, CD56, CD57. Most tumors involve NK cells but also involve T cells as neoplastic cells, that is the main reason of classification as NK/T-cell lymphoma rather than NK-cell lymphoma. the immunophenotype of NK lymphoma cells is classically positive for CD2, CD56, and cytoplasmic CD3 epsilon. they are negative for surface CD3. Unlike normal NK cells, the tumor cells are usually negative for CD7 and CD16. they express cytotoxic granule associated proteins granzyme B, T-cell restricted intracellular antigen (TIA-1), and perforin. NK/T cell lymphoma expressing CD56 is rare but most commonly occurs int he head and neck region, skin, and soft tissue. genes involved in the pathogenesis of extranodal NK-T-cell lymphoma include.:HLA DQA1*0501, HLA DQB1*0201. these genes also are relevant with celiac disease.On gross pathology, angiocentric and angiodestructive pattern of growth with associated geographical necrosis and ulceration are characteristic findings of extranodal NK-T-cell lymphoma.Coagulative necrosis and apoptotic bodies are frequently encountered., Extranodal NK/T-cell lymphoma, nasal type occurs in nasal cavity and upper aerodigestive tract., Extranodal NK/T cell lymphoma, nasal type affects the nose and facial mid line exhibiting aggressive destruction., on microscopic histopathological analysis, medium sized tumor cells and polymorphic infiltrate of non-neoplastic inflammatory cells are characteristic findings of extranodal NK-T-cell lymphoma. the tumor cells are small to medium in size with occasional large and anaplastic forms. the lymphoma cells may be admixed with a polymorphic infiltrate of nonneoplastic inflammatory cells including small lymphocytes, plasma cells, histiocytes, and eosinophils.
Pathophysiology
Physiology
- NK cells are CD3 and myloperoxidase negative on their surface.[1]
- NK cells have germline configuration of T-cell receptor and immunoglobulin genes.[2]
- NK cells originate from a bipotent NK/T-progenitor cell so they have a lot in common with T cells.[3]
- NK cells express T-associate markers such as CD2, CD3e, CD7, CD8, CD16, CD56, CD57.[4]
- Most tumors involve NK cells but also involve T cells as neoplastic cells, that is the main reason of classification as NK/T-cell lymphoma rather than NK-cell lymphoma.[5]
Immunotype
- The immunophenotype of NK lymphoma cells is classically positive for CD2, CD56, and cytoplasmic CD3 epsilon.[6]
- They are negative for surface CD3. Unlike normal NK cells, the tumor cells are usually negative for CD7 and CD16.
- They express cytotoxic granule associated proteins granzyme B, T-cell restricted intracellular antigen (TIA-1), and perforin.
- NK/T cell lymphoma expressing CD56 is rare but most commonly occurs int he head and neck region, skin, and soft tissue.
Genetics
Genes involved in the pathogenesis of extranodal NK-T-cell lymphoma include.[7]:
These genes also are relevant with celiac disease.
Gross Pathology
- On gross pathology, angiocentric and angiodestructive pattern of growth with associated geographical necrosis and ulceration are characteristic findings of extranodal NK-T-cell lymphoma.[8]
- Coagulative necrosis and apoptotic bodies are frequently encountered.
- Extranodal NK/T-cell lymphoma, nasal type occurs in nasal cavity and upper aerodigestive tract.
- Extranodal NK/T cell lymphoma, nasal type affects the nose and facial mid line exhibiting aggressive destruction.

Microscopic Pathology
- On microscopic histopathological analysis, medium sized tumor cells and polymorphic infiltrate of non-neoplastic inflammatory cells are characteristic findings of extranodal NK-T-cell lymphoma.[10]
- The tumor cells are small to medium in size with occasional large and anaplastic forms.
- The lymphoma cells may be admixed with a polymorphic infiltrate of nonneoplastic inflammatory cells including small lymphocytes, plasma cells, histiocytes, and eosinophils.
References
- ↑ Ham, Maria Francisca; Ko, Young-Hyeh (2010). "Natural killer cell neoplasm: biology and pathology". International Journal of Hematology. 92 (5): 681–689. doi:10.1007/s12185-010-0738-y. ISSN 0925-5710.
- ↑ Extranodal NK/T-cell lymphoma, nasal type. Canadian Cancer Society. http://www.cancer.ca/en/cancer-information/cancer-type/non-hodgkin-lymphoma/non-hodgkin-lymphoma/types-of-nhl/extranodal-nk-t-cell-lymphoma-nasal-type/?region=on. Accessed on February 19, 2016
- ↑ Extranodal Natural-Killer/T-Cell Lymphoma, Nasal Type. Hindawi Publishing Corporation. http://www.hindawi.com/journals/ah/2010/627401/. Accessed on February 18, 2016
- ↑ Stewart CA, Walzer T, Robbins SH, Malissen B, Vivier E, Prinz I (2007). "Germ-line and rearranged Tcrd transcription distinguish bona fide NK cells and NK-like gammadelta T cells". Eur J Immunol. 37 (6): 1442–52. doi:10.1002/eji.200737354. PMID 17492716.
- ↑ Jaffe ES, Nicolae A, Pittaluga S (January 2013). "Peripheral T-cell and NK-cell lymphomas in the WHO classification: pearls and pitfalls". Mod. Pathol. 26 Suppl 1: S71–87. doi:10.1038/modpathol.2012.181. PMC 6324567. PMID 23281437.
- ↑ Ko, Y H; Cho, E-Y; Kim, J-E; Lee, S-S; Huh, J-R; Chang, H-K; Yang, W-I; Kim, C-W; Kim, S-W; Ree, H J (2004). "NK and NK-like T-cell lymphoma in extranasal sites: a comparative clinicopathological study according to site and EBV status". Histopathology. 44 (5): 480–489. doi:10.1111/j.1365-2559.2004.01867.x. ISSN 0309-0167.
- ↑ Swerdlow, Steven (2017). WHO classification of tumours of haematopoietic and lymphoid tissues. Lyon: International Agency for Research on Cancer. ISBN 9789283244943.
- ↑ Ko, Y H; Cho, E-Y; Kim, J-E; Lee, S-S; Huh, J-R; Chang, H-K; Yang, W-I; Kim, C-W; Kim, S-W; Ree, H J (2004). "NK and NK-like T-cell lymphoma in extranasal sites: a comparative clinicopathological study according to site and EBV status". Histopathology. 44 (5): 480–489. doi:10.1111/j.1365-2559.2004.01867.x. ISSN 0309-0167.
- ↑ "GMS | GMS Current Topics in Otorhinolaryngology - Head and Neck Surgery | Orphan diseases of the nose and paranasal sinuses: Pathogenesis – clinic – therapy".
- ↑ Liu, Chih-Yi; Tsai, Hui-Chih (2018). "Comparison of Diagnostic Cytomorphology of Natural Killer/T-Cell Lymphoma (Nasal Type) in Conventional Smears, Liquid-Based Preparations, and Histopathology". Case Reports in Pathology. 2018: 1–7. doi:10.1155/2018/6264810. ISSN 2090-6781.
- ↑ Fang, Jian-chen; Zhou, Jue; Li, Zheng; Xia, Zhao-xia (2014). "Primary extranodal NK/T cell lymphoma, nasal-type of uterus with adenomyosis: a case report". Diagnostic Pathology. 9 (1). doi:10.1186/1746-1596-9-95. ISSN 1746-1596.