Euthyroid sick syndrome pathophysiology: Difference between revisions
Akshun Kalia (talk | contribs) |
Akshun Kalia (talk | contribs) |
||
| (6 intermediate revisions by 2 users not shown) | |||
| Line 4: | Line 4: | ||
{{CMG}}; {{AE}}{{Akshun}} | {{CMG}}; {{AE}}{{Akshun}} | ||
==Overview== | ==Overview== | ||
[[Euthyroid]] sick syndrome is not a primary [[thyroid]] disorder but instead results from changes induced by the nonthyroidal illness. The cause of [[euthyroid]] sick syndrome is multifactorial. It is thought that [[euthyroid]] sick syndrome is the result of severe [[illness]] and [[inflammation]]. During these [[Stress (medicine)|stress]] conditions, [[hypermetabolism]] occur, that lead to increased [[energy]] expenditure, [[hyperglycemia]], and [[muscle]] loss. It is speculated, that the body induces some degree of [[hypothyroidism]] by inhibiting deiodination of [[T4]] to [[T3]] by the [[enzyme]] 5’-monodeiodinase, in order to contain the [[hypermetabolism]]. This is an [[adaptive]] process by which the [[Human body|body]] prevents further [[muscle]] and [[calorie]] loss. [[Inflammation]] leads to increased production of [[cytokines]] that severely | [[Euthyroid]] sick syndrome is not a primary [[thyroid]] disorder but instead results from changes induced by the nonthyroidal illness. The cause of [[euthyroid]] sick syndrome is multifactorial. It is thought that [[euthyroid]] sick syndrome is the result of severe [[illness]] and [[inflammation]]. During these [[Stress (medicine)|stress]] conditions, [[hypermetabolism]] occur, that lead to increased [[energy]] expenditure, [[hyperglycemia]], and [[muscle]] loss. It is speculated, that the body induces some degree of [[hypothyroidism]] by inhibiting deiodination of [[T4]] to [[T3]] by the [[enzyme]] 5’-monodeiodinase, in order to contain the [[hypermetabolism]]. This is an [[adaptive]] process by which the [[Human body|body]] prevents further [[muscle]] and [[calorie]] loss. [[Inflammation]] leads to increased production of [[cytokines]] that severely affects [[genes]] involved in the production and release of [[T4]] and [[T3]]. There is also [[downregulation]] of [[Thyrotropin-releasing hormone|TRH]] and [[Thyroid-stimulating hormone|TSH]] release from the [[hypothalamus]] and [[pituitary gland]] respectively. This downregulation may be signalled by a decrease in [[leptin]] caused by [[malnutrition]]. On [[gross pathology]], [[euthyroid]] sick syndrome, does not appear to be [[dysfunctional]]. On [[microscopic]] histopathological analysis, [[euthyroid]] sick syndrome presents with normal [[thyroid]] histology. | ||
==Pathophysiology== | ==Pathophysiology== | ||
| Line 10: | Line 10: | ||
===Pathogenesis=== | ===Pathogenesis=== | ||
* [[T3]] ([[triiodothyronine]]) is the biologically active form of [[thyroid hormone]]. Normally most of the [[T3]] ([[triiodothyronine]]) is produced by peripheral deiodination of circulating [[T4]] ([[thyroxine]]) by the enzyme 5’-monodeiodinase (type I). | * [[T3]] ([[triiodothyronine]]) is the biologically active form of [[thyroid hormone]]. Normally most of the [[T3]] ([[triiodothyronine]]) is produced by peripheral deiodination of circulating [[T4]] ([[thyroxine]]) by the enzyme 5’-monodeiodinase (type I). | ||
* In [[euthyroid]] sick syndrome there occurs [[inhibition]] of the [[enzyme]] | * In [[euthyroid]] sick syndrome there occurs [[inhibition]] of the [[enzyme]] 5’-monodeiodinase (type I) which leads to decrease conversion of [[T4]] to [[T3]] and an increase in [[reverse T3]] from decreased metabolism. | ||
* [[Euthyroid]] sick syndrome is seen in [[conditions]] of [[starvation]] and [[critical illness]] such as [[sepsis]], [[surgery]], severe [[trauma]], [[burns]], [[metabolic disorders]], [[bone marrow transplantation]], and [[malignancy]].<ref name="pmid8940342">{{cite journal |vauthors=Boelen A, Maas MA, Lowik CW, Platvoet MC, Wiersinga WM |title=Induced illness in interleukin-6 (IL-6) knock-out mice: a causal role of IL-6 in the development of the low 3,5,3'-triiodothyronine syndrome |journal=Endocrinology |volume=137 |issue=12 |pages=5250–4 |year=1996 |pmid=8940342 |doi=10.1210/endo.137.12.8940342 |url=}}</ref><ref name="GRASBERGERGOLCHER2002">{{cite journal|last1=GRASBERGER|first1=Helmut|last2=GOLCHER|first2=Henriette M.B.|last3=FINGERHUT|first3=Anja|last4=JANSSEN|first4=Onno E.|title=Loop variants of the serpin thyroxine-binding globulin: implications for hormone release upon limited proteolysis|journal=Biochemical Journal|volume=365|issue=1|year=2002|pages=311–316|issn=0264-6021|doi=10.1042/bj20020014}}</ref><ref name="pmid10554534">{{cite journal |vauthors=Schilling JU, Zimmermann T, Albrecht S, Zwipp H, Saeger HD |title=[Low T3 syndrome in multiple trauma patients--a phenomenon or important pathogenetic factor?] |language=German |journal=Med. Klin. (Munich) |volume=94 Suppl 3 |issue= |pages=66–9 |year=1999 |pmid=10554534 |doi= |url=}}</ref><ref name="WongHershman1992">{{cite journal|last1=Wong|first1=Timothy K.|last2=Hershman|first2=Jerome M.|title=Changes in thyroid function in nonthyroid illness|journal=Trends in Endocrinology & Metabolism|volume=3|issue=1|year=1992|pages=8–12|issn=10432760|doi=10.1016/1043-2760(92)90085-F}}</ref><ref name="DocterKrenning1993">{{cite journal|last1=Docter|first1=R.|last2=Krenning|first2=E. P.|last3=Jong|first3=M.|last4=Hennemann|first4=G.|title=The sick euthyroid syndrome: changes in thyroid hormone serum parameters and hormone metabolism|journal=Clinical Endocrinology|volume=39|issue=5|year=1993|pages=499–518|issn=0300-0664|doi=10.1111/j.1365-2265.1993.tb02401.x}}</ref><ref name="BartalenaBogazzi1998">{{cite journal|last1=Bartalena|first1=L|last2=Bogazzi|first2=F|last3=Brogioni|first3=S|last4=Grasso|first4=L|last5=Martino|first5=E|title=Role of cytokines in the pathogenesis of the euthyroid sick syndrome|journal=European Journal of Endocrinology|volume=138|issue=6|year=1998|pages=603–614|issn=0804-4643|doi=10.1530/eje.0.1380603}}</ref> | * [[Euthyroid]] sick syndrome is seen in [[conditions]] of [[starvation]] and [[critical illness]] such as [[sepsis]], [[surgery]], severe [[trauma]], [[burns]], [[metabolic disorders]], [[bone marrow transplantation]], and [[malignancy]].<ref name="pmid8940342">{{cite journal |vauthors=Boelen A, Maas MA, Lowik CW, Platvoet MC, Wiersinga WM |title=Induced illness in interleukin-6 (IL-6) knock-out mice: a causal role of IL-6 in the development of the low 3,5,3'-triiodothyronine syndrome |journal=Endocrinology |volume=137 |issue=12 |pages=5250–4 |year=1996 |pmid=8940342 |doi=10.1210/endo.137.12.8940342 |url=}}</ref><ref name="GRASBERGERGOLCHER2002">{{cite journal|last1=GRASBERGER|first1=Helmut|last2=GOLCHER|first2=Henriette M.B.|last3=FINGERHUT|first3=Anja|last4=JANSSEN|first4=Onno E.|title=Loop variants of the serpin thyroxine-binding globulin: implications for hormone release upon limited proteolysis|journal=Biochemical Journal|volume=365|issue=1|year=2002|pages=311–316|issn=0264-6021|doi=10.1042/bj20020014}}</ref><ref name="pmid10554534">{{cite journal |vauthors=Schilling JU, Zimmermann T, Albrecht S, Zwipp H, Saeger HD |title=[Low T3 syndrome in multiple trauma patients--a phenomenon or important pathogenetic factor?] |language=German |journal=Med. Klin. (Munich) |volume=94 Suppl 3 |issue= |pages=66–9 |year=1999 |pmid=10554534 |doi= |url=}}</ref><ref name="WongHershman1992">{{cite journal|last1=Wong|first1=Timothy K.|last2=Hershman|first2=Jerome M.|title=Changes in thyroid function in nonthyroid illness|journal=Trends in Endocrinology & Metabolism|volume=3|issue=1|year=1992|pages=8–12|issn=10432760|doi=10.1016/1043-2760(92)90085-F}}</ref><ref name="DocterKrenning1993">{{cite journal|last1=Docter|first1=R.|last2=Krenning|first2=E. P.|last3=Jong|first3=M.|last4=Hennemann|first4=G.|title=The sick euthyroid syndrome: changes in thyroid hormone serum parameters and hormone metabolism|journal=Clinical Endocrinology|volume=39|issue=5|year=1993|pages=499–518|issn=0300-0664|doi=10.1111/j.1365-2265.1993.tb02401.x}}</ref><ref name="BartalenaBogazzi1998">{{cite journal|last1=Bartalena|first1=L|last2=Bogazzi|first2=F|last3=Brogioni|first3=S|last4=Grasso|first4=L|last5=Martino|first5=E|title=Role of cytokines in the pathogenesis of the euthyroid sick syndrome|journal=European Journal of Endocrinology|volume=138|issue=6|year=1998|pages=603–614|issn=0804-4643|doi=10.1530/eje.0.1380603}}</ref> | ||
** During these [[Stress (medicine)|stress]] conditions, there occurs [[hypermetabolism]], increased [[energy]] expenditure, [[hyperglycemia]], and [[muscle]] loss. It is speculated, that the body in order to contain this [[hypermetabolism]] induces some degree of [[hypothyroidism]] by inhibiting deiodination of [[T4]] to [[T3]] by the [[enzyme]] 5’-monodeiodinase. This is an [[adaptive]] process by which the [[Human body|body]] prevents further [[muscle]] and [[calorie]] loss. | ** During these [[Stress (medicine)|stress]] conditions, there occurs [[hypermetabolism]], increased [[energy]] expenditure, [[hyperglycemia]], and [[muscle]] loss. It is speculated, that the body in order to contain this [[hypermetabolism]] induces some degree of [[hypothyroidism]] by inhibiting deiodination of [[T4]] to [[T3]] by the [[enzyme]] 5’-monodeiodinase. This is an [[adaptive]] process by which the [[Human body|body]] prevents further [[muscle]] and [[calorie]] loss. | ||
** During illness, there is also [[downregulation]] of [[Thyrotropin-releasing hormone|TRH]] and [[Thyroid-stimulating hormone|TSH]] release from the [[hypothalamus]] and [[pituitary gland]] respectively. It may be signalled by a decrease in leptin caused by malnutrition. Under normal conditions, leptin prevents neuropeptide Y (NPY) and agouti-related protein (AGRP) induced downregulation of TRH. | ** During illness, there is also [[downregulation]] of [[Thyrotropin-releasing hormone|TRH]] and [[Thyroid-stimulating hormone|TSH]] release from the [[hypothalamus]] and [[pituitary gland]] respectively. It may be signalled by a decrease in [[leptin]] caused by [[malnutrition]]. Under normal conditions, leptin prevents neuropeptide Y (NPY) and agouti-related protein (AGRP) induced downregulation of [[TRH]]. | ||
** [[In vitro]] studies have shown that high concentrations of [[cytokines]] severely affect [[genes]] involved in the production and release of [[T4]] and [[T3]]. | ** [[In vitro]] studies have shown that high concentrations of [[cytokines]] severely affect [[genes]] involved in the production and release of [[T4]] and [[T3]]. | ||
** Any chronic [[illness]] may impair [[plasma protein]] binding of [[thyroid hormones]], resulting in [[reduced]] levels of total hormones. | ** Any chronic [[illness]] may impair [[plasma protein]] binding of [[thyroid hormones]], resulting in [[reduced]] levels of total hormones. | ||
| Line 20: | Line 20: | ||
==Genetics== | ==Genetics== | ||
[[ | [[Pathogenesis]] of [[euthyroid]] sick syndrome include [[mutation]] in [[LEP]] gene. | ||
*[[LEP]] gene [[mutation]]:<ref name="pmid9165050">{{cite journal |vauthors=Légrádi G, Emerson CH, Ahima RS, Flier JS, Lechan RM |title=Leptin prevents fasting-induced suppression of prothyrotropin-releasing hormone messenger ribonucleic acid in neurons of the hypothalamic paraventricular nucleus |journal=Endocrinology |volume=138 |issue=6 |pages=2569–76 |year=1997 |pmid=9165050 |doi=10.1210/endo.138.6.5209 |url=}}</ref><ref name="RoggeJones2008">{{cite journal|last1=Rogge|first1=G.|last2=Jones|first2=D.|last3=Hubert|first3=G. W.|last4=Lin|first4=Y.|last5=Kuhar|first5=M. J.|title=CART peptides: regulators of body weight, reward and other functions|journal=Nature Reviews Neuroscience|volume=9|issue=10|year=2008|pages=747–758|issn=1471-003X|doi=10.1038/nrn2493}}</ref><ref name="FroguelClément1998">{{cite journal|last1=Froguel|first1=Philippe|last2=Clément|first2=Karine|last3=Vaisse|first3=Christian|last4=Lahlou|first4=Najiba|last5=Cabrol|first5=Sylvie|last6=Pelloux|first6=Veronique|last7=Cassuto|first7=Dominique|last8=Gourmelen|first8=Micheline|last9=Dina|first9=Christian|last10=Chambaz|first10=Jean|last11=Lacorte|first11=Jean-Marc|last12=Basdevant|first12=Arnaud|last13=Bougnères|first13=Pierre|last14=Lebouc|first14=Yves|last15=Guy-Grand|first15=Bernard|title=A mutation in the human leptin receptor gene causes obesity and pituitary dysfunction|journal=Nature|volume=392|issue=6674|year=1998|pages=398–401|issn=00280836|doi=10.1038/32911}}</ref><ref name="pmid16131331">{{cite journal |vauthors=Lechan RM, Fekete C |title=Role of thyroid hormone deiodination in the hypothalamus |journal=Thyroid |volume=15 |issue=8 |pages=883–97 |year=2005 |pmid=16131331 |doi=10.1089/thy.2005.15.883 |url=}}</ref> | *[[LEP]] gene [[mutation]]:<ref name="pmid9165050">{{cite journal |vauthors=Légrádi G, Emerson CH, Ahima RS, Flier JS, Lechan RM |title=Leptin prevents fasting-induced suppression of prothyrotropin-releasing hormone messenger ribonucleic acid in neurons of the hypothalamic paraventricular nucleus |journal=Endocrinology |volume=138 |issue=6 |pages=2569–76 |year=1997 |pmid=9165050 |doi=10.1210/endo.138.6.5209 |url=}}</ref><ref name="RoggeJones2008">{{cite journal|last1=Rogge|first1=G.|last2=Jones|first2=D.|last3=Hubert|first3=G. W.|last4=Lin|first4=Y.|last5=Kuhar|first5=M. J.|title=CART peptides: regulators of body weight, reward and other functions|journal=Nature Reviews Neuroscience|volume=9|issue=10|year=2008|pages=747–758|issn=1471-003X|doi=10.1038/nrn2493}}</ref><ref name="FroguelClément1998">{{cite journal|last1=Froguel|first1=Philippe|last2=Clément|first2=Karine|last3=Vaisse|first3=Christian|last4=Lahlou|first4=Najiba|last5=Cabrol|first5=Sylvie|last6=Pelloux|first6=Veronique|last7=Cassuto|first7=Dominique|last8=Gourmelen|first8=Micheline|last9=Dina|first9=Christian|last10=Chambaz|first10=Jean|last11=Lacorte|first11=Jean-Marc|last12=Basdevant|first12=Arnaud|last13=Bougnères|first13=Pierre|last14=Lebouc|first14=Yves|last15=Guy-Grand|first15=Bernard|title=A mutation in the human leptin receptor gene causes obesity and pituitary dysfunction|journal=Nature|volume=392|issue=6674|year=1998|pages=398–401|issn=00280836|doi=10.1038/32911}}</ref><ref name="pmid16131331">{{cite journal |vauthors=Lechan RM, Fekete C |title=Role of thyroid hormone deiodination in the hypothalamus |journal=Thyroid |volume=15 |issue=8 |pages=883–97 |year=2005 |pmid=16131331 |doi=10.1089/thy.2005.15.883 |url=}}</ref> | ||
**The [[LEP]] [[gene]] encodes for [[leptin]]. | **The [[LEP]] [[gene]] encodes for [[leptin]]. | ||
**Normally, [[α-MSH]] stimulates [[TRH]] gene expression. [[Leptin]] enhances this effect of [[α-MSH]] on [[TRH]] gene expression. | **Normally, [[α-MSH]] stimulates [[TRH]] gene expression. | ||
**[[Leptin]] enhances this effect of [[α-MSH]] on [[TRH]] gene expression. | |||
**[[Leptin]] also decreases [[neuropeptide Y]] (NPY) and [[Agouti-related peptide|agouti-related protein]] (AGRP) induced decrease in [[TRH]] gene expression. | **[[Leptin]] also decreases [[neuropeptide Y]] (NPY) and [[Agouti-related peptide|agouti-related protein]] (AGRP) induced decrease in [[TRH]] gene expression. | ||
** Any chronic [[illness]] or [[starvation]] can lead to decrease in [[leptin]] production. | ** Any chronic [[illness]] or [[starvation]] can lead to decrease in [[leptin]] production. | ||
| Line 38: | Line 39: | ||
*Other [[inflammatory]] conditions | *Other [[inflammatory]] conditions | ||
*[[Metabolic disorders]] | *[[Metabolic disorders]] | ||
*Any major condition of | *Any major condition of: | ||
**[[Cardiovascular system]]: [[Myocardial infarction]] | **[[Cardiovascular system]]: [[Myocardial infarction]] | ||
**[[Respiratory system]] : [[Pneumonia]] | **[[Respiratory system]] : [[Pneumonia]] | ||
| Line 45: | Line 46: | ||
==Gross Pathology== | ==Gross Pathology== | ||
In [[euthyroid]] sick syndrome the [[thyroid gland]] | In [[euthyroid]] sick syndrome the [[thyroid gland]] appears normal on gross pathology. | ||
==Microscopic Pathology== | ==Microscopic Pathology== | ||
Latest revision as of 16:10, 4 November 2017
|
Euthyroid sick syndrome Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Euthyroid sick syndrome pathophysiology On the Web |
|
American Roentgen Ray Society Images of Euthyroid sick syndrome pathophysiology |
|
Risk calculators and risk factors for Euthyroid sick syndrome pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Akshun Kalia M.B.B.S.[2]
Overview
Euthyroid sick syndrome is not a primary thyroid disorder but instead results from changes induced by the nonthyroidal illness. The cause of euthyroid sick syndrome is multifactorial. It is thought that euthyroid sick syndrome is the result of severe illness and inflammation. During these stress conditions, hypermetabolism occur, that lead to increased energy expenditure, hyperglycemia, and muscle loss. It is speculated, that the body induces some degree of hypothyroidism by inhibiting deiodination of T4 to T3 by the enzyme 5’-monodeiodinase, in order to contain the hypermetabolism. This is an adaptive process by which the body prevents further muscle and calorie loss. Inflammation leads to increased production of cytokines that severely affects genes involved in the production and release of T4 and T3. There is also downregulation of TRH and TSH release from the hypothalamus and pituitary gland respectively. This downregulation may be signalled by a decrease in leptin caused by malnutrition. On gross pathology, euthyroid sick syndrome, does not appear to be dysfunctional. On microscopic histopathological analysis, euthyroid sick syndrome presents with normal thyroid histology.
Pathophysiology
Pathogenesis
- T3 (triiodothyronine) is the biologically active form of thyroid hormone. Normally most of the T3 (triiodothyronine) is produced by peripheral deiodination of circulating T4 (thyroxine) by the enzyme 5’-monodeiodinase (type I).
- In euthyroid sick syndrome there occurs inhibition of the enzyme 5’-monodeiodinase (type I) which leads to decrease conversion of T4 to T3 and an increase in reverse T3 from decreased metabolism.
- Euthyroid sick syndrome is seen in conditions of starvation and critical illness such as sepsis, surgery, severe trauma, burns, metabolic disorders, bone marrow transplantation, and malignancy.[1][2][3][4][5][6]
- During these stress conditions, there occurs hypermetabolism, increased energy expenditure, hyperglycemia, and muscle loss. It is speculated, that the body in order to contain this hypermetabolism induces some degree of hypothyroidism by inhibiting deiodination of T4 to T3 by the enzyme 5’-monodeiodinase. This is an adaptive process by which the body prevents further muscle and calorie loss.
- During illness, there is also downregulation of TRH and TSH release from the hypothalamus and pituitary gland respectively. It may be signalled by a decrease in leptin caused by malnutrition. Under normal conditions, leptin prevents neuropeptide Y (NPY) and agouti-related protein (AGRP) induced downregulation of TRH.
- In vitro studies have shown that high concentrations of cytokines severely affect genes involved in the production and release of T4 and T3.
- Any chronic illness may impair plasma protein binding of thyroid hormones, resulting in reduced levels of total hormones.
- Euthyroid sick syndrome presents with low serum T3. Depending upon the severity and duration of the stress inducing condition, the thyroid-stimulating hormone(TSH), thyroxine (T4), and free T4 (FT4) are affected in variable proportions. The drop in levels of T3 and T4 are more with more severe illnesses. Mortality rate is high when there is a marked decrease in serum T3 and T4.
Genetics
Pathogenesis of euthyroid sick syndrome include mutation in LEP gene.
- LEP gene mutation:[7][8][9][10]
- The LEP gene encodes for leptin.
- Normally, α-MSH stimulates TRH gene expression.
- Leptin enhances this effect of α-MSH on TRH gene expression.
- Leptin also decreases neuropeptide Y (NPY) and agouti-related protein (AGRP) induced decrease in TRH gene expression.
- Any chronic illness or starvation can lead to decrease in leptin production.
- Patients who have a defective LEP or leptin receptor due to genetic mutations and who develop chronic illness later in life show reduced TRH secretion and features of euthyroid sick syndrome.[11][12][13]
Associated Conditions
Euthyroid sick syndrome is seen with starvation and severe illness such as:[14][15]
- Sepsis
- Malignancy
- Trauma
- Surgery
- Burns
- Bone marrow transplantation
- Other inflammatory conditions
- Metabolic disorders
- Any major condition of:
Gross Pathology
In euthyroid sick syndrome the thyroid gland appears normal on gross pathology.
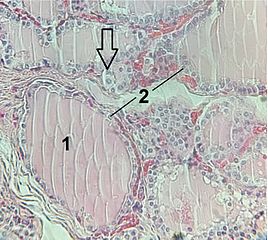
Microscopic Pathology
On microscopic histopathological analysis, euthyroid sick syndrome presents with normal thyroid histology.
References
- ↑ Boelen A, Maas MA, Lowik CW, Platvoet MC, Wiersinga WM (1996). "Induced illness in interleukin-6 (IL-6) knock-out mice: a causal role of IL-6 in the development of the low 3,5,3'-triiodothyronine syndrome". Endocrinology. 137 (12): 5250–4. doi:10.1210/endo.137.12.8940342. PMID 8940342.
- ↑ GRASBERGER, Helmut; GOLCHER, Henriette M.B.; FINGERHUT, Anja; JANSSEN, Onno E. (2002). "Loop variants of the serpin thyroxine-binding globulin: implications for hormone release upon limited proteolysis". Biochemical Journal. 365 (1): 311–316. doi:10.1042/bj20020014. ISSN 0264-6021.
- ↑ Schilling JU, Zimmermann T, Albrecht S, Zwipp H, Saeger HD (1999). "[Low T3 syndrome in multiple trauma patients--a phenomenon or important pathogenetic factor?]". Med. Klin. (Munich) (in German). 94 Suppl 3: 66–9. PMID 10554534.
- ↑ Wong, Timothy K.; Hershman, Jerome M. (1992). "Changes in thyroid function in nonthyroid illness". Trends in Endocrinology & Metabolism. 3 (1): 8–12. doi:10.1016/1043-2760(92)90085-F. ISSN 1043-2760.
- ↑ Docter, R.; Krenning, E. P.; Jong, M.; Hennemann, G. (1993). "The sick euthyroid syndrome: changes in thyroid hormone serum parameters and hormone metabolism". Clinical Endocrinology. 39 (5): 499–518. doi:10.1111/j.1365-2265.1993.tb02401.x. ISSN 0300-0664.
- ↑ Bartalena, L; Bogazzi, F; Brogioni, S; Grasso, L; Martino, E (1998). "Role of cytokines in the pathogenesis of the euthyroid sick syndrome". European Journal of Endocrinology. 138 (6): 603–614. doi:10.1530/eje.0.1380603. ISSN 0804-4643.
- ↑ Légrádi G, Emerson CH, Ahima RS, Flier JS, Lechan RM (1997). "Leptin prevents fasting-induced suppression of prothyrotropin-releasing hormone messenger ribonucleic acid in neurons of the hypothalamic paraventricular nucleus". Endocrinology. 138 (6): 2569–76. doi:10.1210/endo.138.6.5209. PMID 9165050.
- ↑ Rogge, G.; Jones, D.; Hubert, G. W.; Lin, Y.; Kuhar, M. J. (2008). "CART peptides: regulators of body weight, reward and other functions". Nature Reviews Neuroscience. 9 (10): 747–758. doi:10.1038/nrn2493. ISSN 1471-003X.
- ↑ Froguel, Philippe; Clément, Karine; Vaisse, Christian; Lahlou, Najiba; Cabrol, Sylvie; Pelloux, Veronique; Cassuto, Dominique; Gourmelen, Micheline; Dina, Christian; Chambaz, Jean; Lacorte, Jean-Marc; Basdevant, Arnaud; Bougnères, Pierre; Lebouc, Yves; Guy-Grand, Bernard (1998). "A mutation in the human leptin receptor gene causes obesity and pituitary dysfunction". Nature. 392 (6674): 398–401. doi:10.1038/32911. ISSN 0028-0836.
- ↑ Lechan RM, Fekete C (2005). "Role of thyroid hormone deiodination in the hypothalamus". Thyroid. 15 (8): 883–97. doi:10.1089/thy.2005.15.883. PMID 16131331.
- ↑ Abo-Zenah HA, Shoeb SA, Sabry AA, Ismail HA (2008). "Relating circulating thyroid hormone concentrations to serum interleukins-6 and -10 in association with non-thyroidal illnesses including chronic renal insufficiency". BMC Endocr Disord. 8: 1. doi:10.1186/1472-6823-8-1. PMC 2254394. PMID 18211669.
- ↑ Stouthard JM, van der Poll T, Endert E, Bakker PJ, Veenhof CH, Sauerwein HP, Romijn JA (1994). "Effects of acute and chronic interleukin-6 administration on thyroid hormone metabolism in humans". J. Clin. Endocrinol. Metab. 79 (5): 1342–6. doi:10.1210/jcem.79.5.7962327. PMID 7962327.
- ↑ Wawrzynska L, Sakowicz A, Rudzinski P, Langfort R, Kurzyna M (2003). "The conversion of thyroxine to triiodothyronine in the lung: comparison of activity of type I iodothyronine 5' deiodinase in lung cancer with peripheral lung tissues". Monaldi Arch Chest Dis. 59 (2): 140–5. PMID 14635503.
- ↑ Silva MH, Araujo MC, Diniz EM, Ceccon ME, Carvalho WB (2015). "Nonthyroidal illnesses syndrome in full-term newborns with sepsis". Arch Endocrinol Metab. 59 (6): 528–34. doi:10.1590/2359-3997000000111. PMID 26677087.
- ↑ Frączek MM, Gackowski A, Przybylik-Mazurek E, Nessler J (2016). "[The relation between the low T3 syndrome in the clinical course of myocardial infarction and heart failure]". Pol. Merkur. Lekarski (in Polish). 40 (240): 380–3. PMID 27403906.