Esophageal cancer differential diagnosis: Difference between revisions
Jump to navigation
Jump to search
m (Bot: Removing from Primary care) |
|||
| (9 intermediate revisions by one other user not shown) | |||
| Line 96: | Line 96: | ||
|- | |- | ||
! align="center" style="background:#DCDCDC;" + |[[Esophageal stricture]] | ! align="center" style="background:#DCDCDC;" + |[[Esophageal stricture]] | ||
| align=" | | align="center" style="background:#F5F5F5;" + |Sudden onset and gradual progressive dysphasia to solids | ||
| align="center" style="background:#F5F5F5;" + | | | align="center" style="background:#F5F5F5;" + |± | ||
| align="center" style="background:#F5F5F5;" + | | | align="center" style="background:#F5F5F5;" + |± | ||
| align="left" style="background:#F5F5F5;" + | | | align="left" style="background:#F5F5F5;" + | | ||
* [[Odynophagia]] | * [[Odynophagia]] | ||
| Line 120: | Line 120: | ||
* [[Esophagogram|Barium esophagogram]] | * [[Esophagogram|Barium esophagogram]] | ||
|- | |- | ||
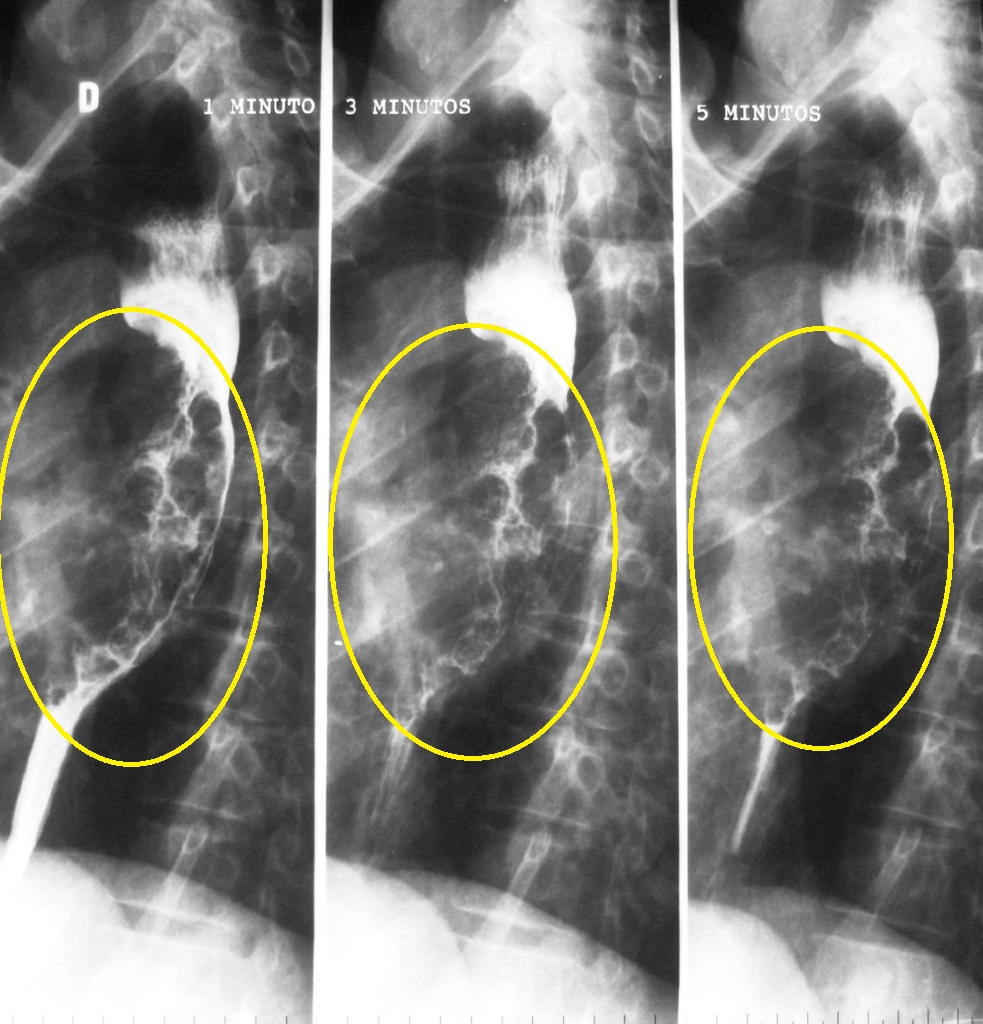
! align="center" style="background:#DCDCDC;" + |[[Diffuse esophageal spasm]] | |||
|Sudden non-progressive dysphagia to solid and liquid | | align="center" style="background:#F5F5F5;" + |Sudden non-progressive dysphagia to solid and liquid | ||
| | | align="center" style="background:#F5F5F5;" + | + | ||
| | | align="center" style="background:#F5F5F5;" + | + | ||
| | | align="left" style="background:#F5F5F5;" + | | ||
* [[Chest pain]] | * [[Chest pain]] | ||
| | | align="left" style="background:#F5F5F5;" + | | ||
* Nonperistaltic and nonpropulsive contractions | * Nonperistaltic and nonpropulsive contractions | ||
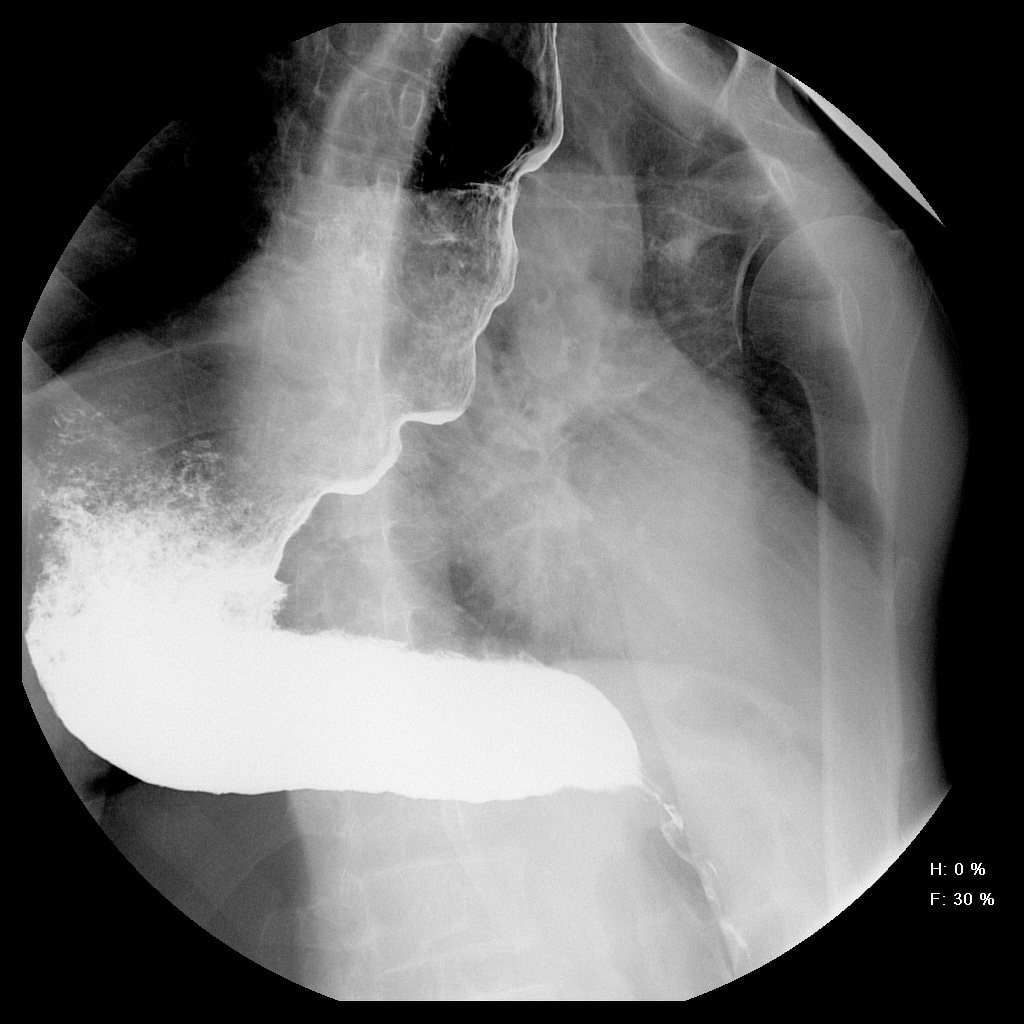
* Corkscrew or rosary bead esophagus | * Corkscrew or rosary bead esophagus | ||
[[Image:DES radio.png|center|200px|thumb|Barium swallow appearance of DES<br>Source:By Nevit Dilmen [CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0)]] | [[Image:DES radio.png|center|200px|thumb|Barium swallow appearance of DES<br>Source:By Nevit Dilmen [CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0)]] | ||
| | | align="left" style="background:#F5F5F5;" + | | ||
* Inconclusive | * Inconclusive | ||
<div style="width:350px">{{#ev:youtube|2ipA34iMA3c}}</div> | <div style="width:350px">{{#ev:youtube|2ipA34iMA3c}}</div> | ||
| | | align="left" style="background:#F5F5F5;" + | | ||
*[[Manometry]] shows high-amplitude [[esophageal]] contractions | *[[Manometry]] shows high-amplitude [[esophageal]] contractions | ||
*[[CT scan]] may show [[hypertrophy]] of esophageal muscles | *[[CT scan]] may show [[hypertrophy]] of esophageal muscles | ||
| | | align="left" style="background:#F5F5F5;" + | | ||
* [[Manometry]] | * [[Manometry]] | ||
|- | |- | ||
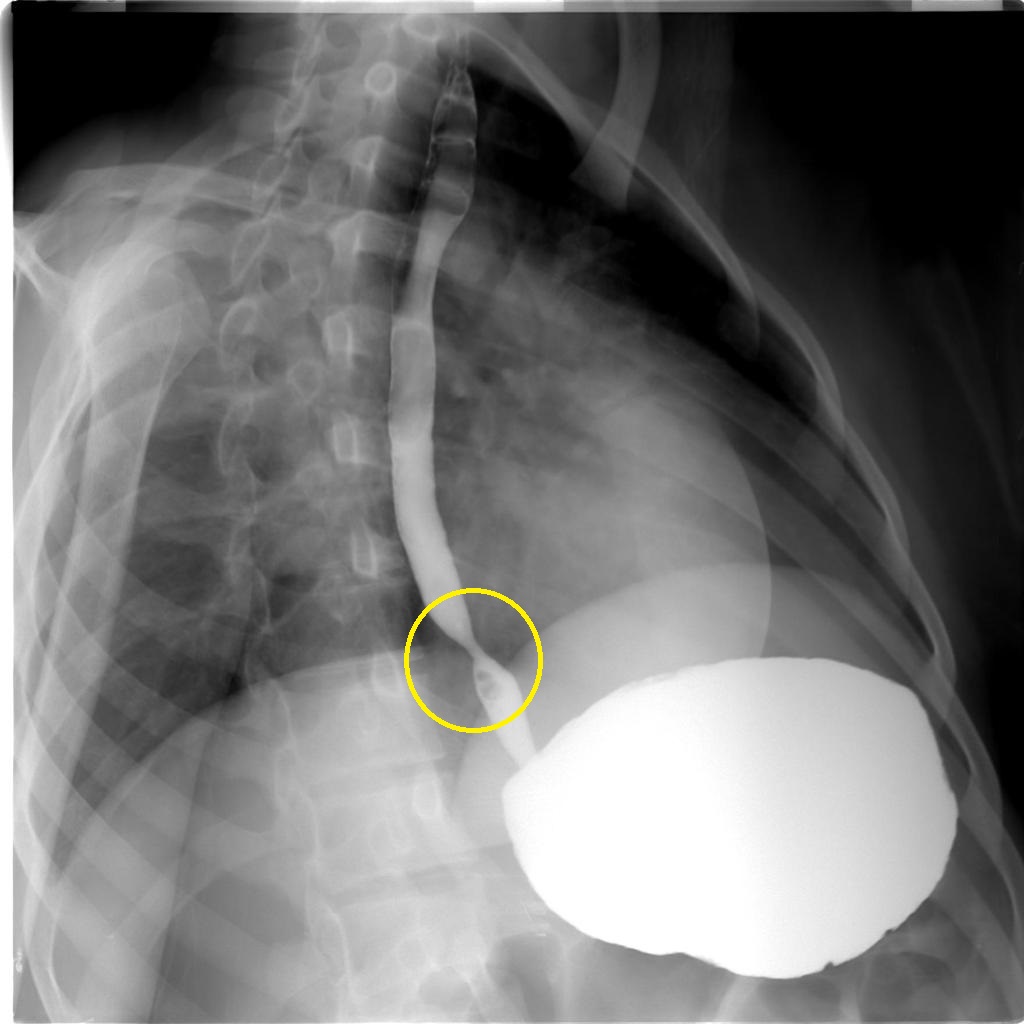
! align="center" style="background:#DCDCDC;" + |[[Achalasia]] | |||
|Gradual non-progressive dysphagia to | | align="center" style="background:#F5F5F5;" + |Gradual non-progressive dysphagia to solid and liquid | ||
solid and liquid | | align="center" style="background:#F5F5F5;" + |± | ||
| + | | align="center" style="background:#F5F5F5;" + | - | ||
| - | | align="left" style="background:#F5F5F5;" + | | ||
| | * [[Dyspnea]] | ||
* [[Regurgitation]] of undigested food | * [[Regurgitation]] of undigested food | ||
* [[Chest pain]] | * [[Chest pain]] | ||
| | * [[Cough]] | ||
| align="left" style="background:#F5F5F5;" + | | |||
* "Bird's beak" or "rat tail" appearance | * "Bird's beak" or "rat tail" appearance | ||
* Dilated esophageal body | * Dilated esophageal body | ||
| Line 153: | Line 154: | ||
* Absence of an intragastric air bubble | * Absence of an intragastric air bubble | ||
[[Image:Achalasia-2.jpg|center|200px|thumb|Case courtesy of Dr Mario Umana, Radiopaedia.org, rID: 38071]] | [[Image:Achalasia-2.jpg|center|200px|thumb|Case courtesy of Dr Mario Umana, Radiopaedia.org, rID: 38071]] | ||
| | | align="left" style="background:#F5F5F5;" + | | ||
* Dilated [[esophagus]] | * Dilated [[esophagus]] | ||
* Residual food fragments | * Residual food fragments | ||
* Normal [[mucosa]] | * Normal [[mucosa]] | ||
<div style="width:350px">{{#ev:youtube|ydLcskQzEjM}}</div> | <div style="width:350px">{{#ev:youtube|ydLcskQzEjM}}</div> | ||
| | | align="left" style="background:#F5F5F5;" + | | ||
* Residual pressure of [[Lower esophageal sphincter|LES]] > 10 mmHg | * Residual pressure of [[Lower esophageal sphincter|LES]] > 10 mmHg | ||
* Incomplete relaxation of the [[Lower esophageal sphincter|LES]] | * Incomplete relaxation of the [[Lower esophageal sphincter|LES]] | ||
* Increased resting tone of [[Lower esophageal sphincter|LES]] | * Increased resting tone of [[Lower esophageal sphincter|LES]] | ||
* Aperistalsis | * Aperistalsis | ||
| | | align="left" style="background:#F5F5F5;" + | | ||
* History of [[dysphagia]] with positive [[endoscopy]] and [[manometry]] | * History of [[dysphagia]] with positive [[endoscopy]] and [[manometry]] | ||
|- | |- | ||
! align="center" style="background:#DCDCDC;" + |[[Systemic sclerosis]] | |||
|Gradual progressive dysphasia to | | align="center" style="background:#F5F5F5;" + |Gradual progressive dysphasia to solid and liquid | ||
solid and liquid | | align="center" style="background:#F5F5F5;" + |± | ||
| + | | align="center" style="background:#F5F5F5;" + | + | ||
| + | | align="left" style="background:#F5F5F5;" + | | ||
| | |||
* [[Muscle pain|Muscle]] and [[Arthralgia|joint pain]] | * [[Muscle pain|Muscle]] and [[Arthralgia|joint pain]] | ||
* [[Raynaud's phenomenon]] | * [[Raynaud's phenomenon]] | ||
* [[Skin changes]] | * [[Skin changes]] | ||
| | | align="left" style="background:#F5F5F5;" + | | ||
* Dysmotility | * Dysmotility | ||
* Patulous [[esophagus]] | * Patulous [[esophagus]] | ||
| | | align="left" style="background:#F5F5F5;" + | | ||
* [[Mucosal]] damage | * [[Mucosal]] damage | ||
* [[Peptic]] stricture (advanced cases) | * [[Peptic]] stricture (advanced cases) | ||
|Positive serology for | | align="left" style="background:#F5F5F5;" + |Positive serology for | ||
* [[Antinuclear antibodies]] | * [[Antinuclear antibodies]] | ||
* [[Rheumatoid factor]] | * [[Rheumatoid factor]] | ||
* [[Creatine kinase]] | * [[Creatine kinase]] | ||
* [[ESR]] | * [[ESR]] | ||
| | | align="left" style="background:#F5F5F5;" + | | ||
* [[Skin biopsy]] | * [[Skin biopsy]] | ||
|- | |- | ||
! align="center" style="background:#DCDCDC;" + |[[Zenker's diverticulum]] | |||
|Gradual dysphasia to | | align="center" style="background:#F5F5F5;" + |Gradual dysphasia to solid | ||
solid | | align="center" style="background:#F5F5F5;" + |± | ||
| + | | align="center" style="background:#F5F5F5;" + | - | ||
| - | | align="left" style="background:#F5F5F5;" + | | ||
| | |||
* Food [[regurgitation]] | * Food [[regurgitation]] | ||
* [[Halitosis]] | * [[Halitosis]] | ||
* [[Coughing|Cough]] | * [[Coughing|Cough]] | ||
* [[Hoarseness]] | * [[Hoarseness]] | ||
| | | align="left" style="background:#F5F5F5;" + | | ||
* Thin projections on [[esophageal]] wall over [[Killian's dehiscence|Killian's triangle]] | * Thin projections on [[esophageal]] wall over [[Killian's dehiscence|Killian's triangle]] | ||
| | | align="left" style="background:#F5F5F5;" + | | ||
* Outpouching of posterior [[pharyngeal]] wall | * Outpouching of posterior [[pharyngeal]] wall | ||
* Exclude the presence of [[Squamous cell carcinoma|SCC]] | * Exclude the presence of [[Squamous cell carcinoma|SCC]] | ||
<div style="width:350px">{{#ev:youtube|FdEruFsNdVA}}</div> | <div style="width:350px">{{#ev:youtube|FdEruFsNdVA}}</div> | ||
| | | align="left" style="background:#F5F5F5;" + | | ||
* [[CT]] & [[MRI]] shows out-pouching over the posterior esophagus in the Killian's triangle | * [[CT]] & [[MRI]] shows out-pouching over the posterior esophagus in the Killian's triangle | ||
| | | align="left" style="background:#F5F5F5;" + | | ||
* Barium [[Esophagogram|esophagography]] | * Barium [[Esophagogram|esophagography]] | ||
|- | |- | ||
! align="center" style="background:#DCDCDC;" + |[[Stroke]] ([[Cerebral hemorrhage]]) | |||
([[Cerebral hemorrhage]]) | | align="center" style="background:#F5F5F5;" + |Sudden progressive dysphasia to solid and liquid | ||
|Sudden progressive dysphasia to | | align="center" style="background:#F5F5F5;" + | + | ||
solid and liquid | | align="center" style="background:#F5F5F5;" + |± | ||
| | | align="left" style="background:#F5F5F5;" + | | ||
| | |||
| | |||
* [[Dysarthria]] | * [[Dysarthria]] | ||
* Limb [[weakness]] | * Limb [[weakness]] | ||
* [[Fatigue]] | * [[Fatigue]] | ||
| | | align="left" style="background:#F5F5F5;" + | | ||
* Pooling of [[Contrast medium|contrast]] in the [[pharynx]] | * Pooling of [[Contrast medium|contrast]] in the [[pharynx]] | ||
* [[Aspiration]] of [[barium]] [[Contrast medium|contrast]] into the [[airway]] | * [[Aspiration]] of [[barium]] [[Contrast medium|contrast]] into the [[airway]] | ||
| | | align="left" style="background:#F5F5F5;" + | | ||
* Reduced opening of [[upper esophageal sphincter]] | * Reduced opening of [[upper esophageal sphincter]] | ||
* Reduced [[larynx]] elevation | * Reduced [[larynx]] elevation | ||
| | | align="left" style="background:#F5F5F5;" + | | ||
* [[CT]] without [[contrast]] shows acute [[hemorrhage]] as a hyperattenuating [[clot]] | * [[CT]] without [[contrast]] shows acute [[hemorrhage]] as a hyperattenuating [[clot]] | ||
| | | align="left" style="background:#F5F5F5;" + | | ||
* [[CT]] without [[Contrast medium|contrast]] | * [[CT]] without [[Contrast medium|contrast]] | ||
|- | |- | ||
! align="center" style="background:#DCDCDC;" + |Motor disorders ([[Myasthenia gravis]]) | |||
([[Myasthenia gravis]]) | | align="center" style="background:#F5F5F5;" + |Gradual progressive dysphasia to solid and liquid | ||
|Gradual progressive dysphasia to | | align="center" style="background:#F5F5F5;" + |± | ||
solid and liquid | | align="center" style="background:#F5F5F5;" + | | ||
| | | align="left" style="background:#F5F5F5;" + | | ||
| | |||
| | |||
* [[Ptosis]] | * [[Ptosis]] | ||
* [[Diplopia]] | * [[Diplopia]] | ||
* [[Fatigue]] | * [[Fatigue]] | ||
| | | align="left" style="background:#F5F5F5;" + | | ||
* Stasis in [[pharynx]] and pooling in pharyngeal recesses | * Stasis in [[pharynx]] and pooling in pharyngeal recesses | ||
| | | align="left" style="background:#F5F5F5;" + | | ||
* [[Velopharyngeal insufficiency]] | * [[Velopharyngeal insufficiency]] | ||
* Delayed [[swallowing]] function | * Delayed [[swallowing]] function | ||
| | | align="left" style="background:#F5F5F5;" + | | ||
* CT may show anterior [[mediastinal]] mass ([[thymoma]]) | * CT may show anterior [[mediastinal]] mass ([[thymoma]]) | ||
* Positive tensilon test | * Positive tensilon test | ||
| | | align="left" style="background:#F5F5F5;" + | | ||
* Anti–acetylcholine receptor antibody test | * Anti–acetylcholine receptor antibody test | ||
|- | |- | ||
! align="center" style="background:#DCDCDC;" + |[[GERD]] | |||
|Sudden onset gradual progressive dysphasia to | | align="center" style="background:#F5F5F5;" + |Sudden onset gradual progressive dysphasia to solid | ||
solid | | align="center" style="background:#F5F5F5;" + |± | ||
| + | | align="center" style="background:#F5F5F5;" + | + | ||
| + | | align="left" style="background:#F5F5F5;" + | | ||
| | |||
* [[Cough]] | * [[Cough]] | ||
* [[Hoarseness]] | * [[Hoarseness]] | ||
| | * Retrosternal burning [[chest pain]] | ||
| align="left" style="background:#F5F5F5;" + | | |||
* Free acid reflux | * Free acid reflux | ||
* [[Esophagitis]] with scarring | * [[Esophagitis]] with scarring | ||
* [[Strictures]] | * [[Strictures]] | ||
* [[Barrett's oesophagus]] | * [[Barrett's oesophagus]] | ||
| | | align="left" style="background:#F5F5F5;" + | | ||
* [[Erythema]], erosions and [[ulceration]] | * [[Erythema]], erosions and [[ulceration]] | ||
* [[Barrett's esophagus]] | * [[Barrett's esophagus]] | ||
| | | align="left" style="background:#F5F5F5;" + | | ||
* Esophageal [[manometry]] may show decreased tone of [[Lower esophageal sphincter|LES]] | * Esophageal [[manometry]] may show decreased tone of [[Lower esophageal sphincter|LES]] | ||
| | | align="left" style="background:#F5F5F5;" + | | ||
* 24 hour [[esophageal]] pH monitoring | * 24 hour [[esophageal]] pH monitoring | ||
|- | |- | ||
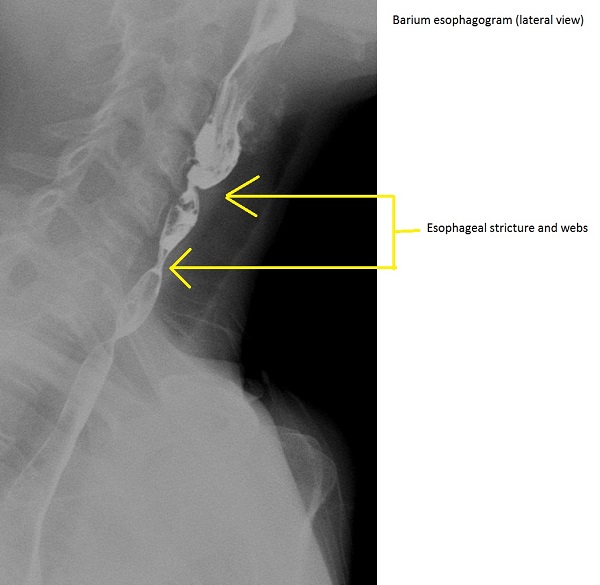
! align="center" style="background:#DCDCDC;" + |[[Esophageal web]] | |||
|Gradual progressive dysphasia to | | align="center" style="background:#F5F5F5;" + |Gradual progressive dysphasia to solid and/or liquid | ||
solid and/or liquid | | align="center" style="background:#F5F5F5;" + | - | ||
| - | | align="center" style="background:#F5F5F5;" + |± | ||
| + | | align="left" style="background:#F5F5F5;" + | | ||
| | |||
* Findings of the underlying cause such as [[iron deficiency anemia]] or [[bullous pemphigoid]] | * Findings of the underlying cause such as [[iron deficiency anemia]] or [[bullous pemphigoid]] | ||
| | | align="left" style="background:#F5F5F5;" + | | ||
* Symmetrical narrowing of the [[esophagus]] | * Symmetrical narrowing of the [[esophagus]] | ||
| | | align="left" style="background:#F5F5F5;" + | | ||
* Smooth membrane not encircling the whole [[Lumen (anatomy)|lumen]] | * Smooth membrane not encircling the whole [[Lumen (anatomy)|lumen]] | ||
| | | align="left" style="background:#F5F5F5;" + | | ||
* Videofluoroscopy shows [[mucosal]] and [[submucosal]] foldings | * Videofluoroscopy shows [[mucosal]] and [[submucosal]] foldings | ||
| | | align="left" style="background:#F5F5F5;" + | | ||
* Barium [[esophagogram]] | * Barium [[esophagogram]] | ||
|} | |} | ||
| Line 375: | Line 287: | ||
{{reflist|2}} | {{reflist|2}} | ||
[[Category: | [[Category:Medicine]] | ||
[[Category:Gastroenterology]] | [[Category:Gastroenterology]] | ||
[[Category:Oncology]] | [[Category:Oncology]] | ||
[[Category:Surgery]] | [[Category:Surgery]] | ||
[[Category:Up-To-Date]] | |||
[[Category:Differential diagnosis]] | [[Category:Differential diagnosis]] | ||
Latest revision as of 21:40, 29 July 2020

Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]Associate Editor(s)-in-Chief: Parminder Dhingra, M.D. [2]Hadeel Maksoud M.D.[3]
Overview
Esophageal cancer must be differentiated from gastroesophageal reflux disease (GERD), Barrett's esophagus, esophageal achalasia, gastritis, gastric ulcer, and stomach cancer.
Differentiating Esophageal cancer from other Diseases
Approach to dysphasia
| Dysphagia | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Oropharyngeal dysphagia | Esophageal dysphagia | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Solids only | Solids and Liquids | Solids only | Solids and Liquids | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
❑Zenker's diverticulum ❑Neoplasm ❑Webs | Neurogenic | Myogenic | Pain | ❑Achalasia ❑Scleroderma ❑DES | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
❑Myasthenia gravis ❑Connective tissue disorder ❑Myotonic dystrophy | No | Yes | ❑Heart burn | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Barium swallow | Mental status | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
❑Pill esophagitis ❑Caustic injury ❑Chemotherapy | Yes | No | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Impaired | Normal | Non progressive | Progressive | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Sac | Webs | Mass | ❑Scleroderma | ❑Achalasia ❑DES | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
❑Stroke | ❑ALS ❑Parkinsonism | ❑Rings ❑Webs | ❑Strictures ❑Cancer | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
❑Zenker's diverticulum | ❑Plummer-Vinson syndrome | ❑Carcinoma | Chest pain and manometry | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Barium swallow | Weight loss | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Increase LES pressure | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
❑Rings | ❑Webs | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Rapid | Slow | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
❑Achalasia | ❑DES | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
❑Esophageal cancer | ❑Strictures/GERD | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Differentiating Esophageal cancer from other Diseases
- Esophageal adenocarcinoma must be differentiated from other causes of dysphagia, odynophagia and food regurgitation such as GERD, esophageal stricture, reflux esophagitis, systemic sclerosis, esophageal spasm, pseudoachalasia, stroke, esophageal candidiasis and Chagas disease.[1][2][3][4][5][6][7][8][9][10][11]
| Disease | Signs and Symptoms | Barium esophagogram | Endoscopy | Other imaging and laboratory findings | Gold Standard | |||
|---|---|---|---|---|---|---|---|---|
| Dysphagia | Weight loss | Heartburn | Other findings | |||||
| Esophageal carcinoma | Gradual progressive dysphasia to solid and liquid | + | ± |
 |
{{#ev:youtube|5ucSlgqGAno}}
|
|||
| Plummer-Vinson syndrome | Gradual non-progressive dysphagia to solids | ± | - |
|
 |
{{#ev:youtube|HFfsTgsB6Pg}}
|
|
Triad of |
| Esophageal stricture | Sudden onset and gradual progressive dysphasia to solids | ± | ± |
 |
{{#ev:youtube|vax5E-jMnQ}}
|
|
||
| Diffuse esophageal spasm | Sudden non-progressive dysphagia to solid and liquid | + | + |
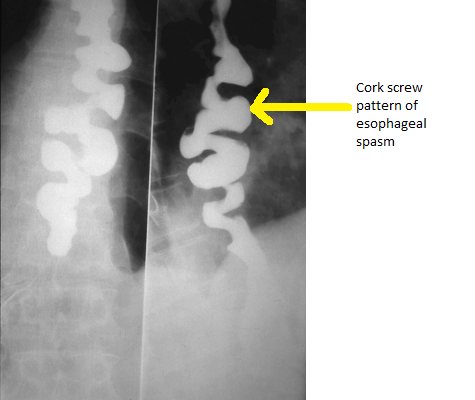 Source:By Nevit Dilmen [CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0) |
{{#ev:youtube|2ipA34iMA3c}}
|
|
||
| Achalasia | Gradual non-progressive dysphagia to solid and liquid | ± | - |
|
 |
{{#ev:youtube|ydLcskQzEjM}}
|
||
| Systemic sclerosis | Gradual progressive dysphasia to solid and liquid | ± | + |
|
Positive serology for | |||
| Zenker's diverticulum | Gradual dysphasia to solid | ± | - |
|
{{#ev:youtube|FdEruFsNdVA}}
|
| ||
| Stroke (Cerebral hemorrhage) | Sudden progressive dysphasia to solid and liquid | + | ± |
|
|
|
||
| Motor disorders (Myasthenia gravis) | Gradual progressive dysphasia to solid and liquid | ± |
|
|
|
| ||
| GERD | Sudden onset gradual progressive dysphasia to solid | ± | + |
|
|
|
| |
| Esophageal web | Gradual progressive dysphasia to solid and/or liquid | - | ± |
|
|
|
|
|
References
- ↑ Ferri, Fred (2015). Ferri's clinical advisor 2015 : 5 books in 1. Philadelphia, PA: Elsevier/Mosby. ISBN 978-0323083751.
- ↑ Boeckxstaens GE, Zaninotto G, Richter JE (2013). "Achalasia". Lancet. doi:10.1016/S0140-6736(13)60651-0. PMID 23871090.
- ↑ Badillo R, Francis D (2014). "Diagnosis and treatment of gastroesophageal reflux disease". World J Gastrointest Pharmacol Ther. 5 (3): 105–12. doi:10.4292/wjgpt.v5.i3.105. PMC 4133436. PMID 25133039.
- ↑ Napier KJ, Scheerer M, Misra S (2014). "Esophageal cancer: A Review of epidemiology, pathogenesis, staging workup and treatment modalities". World J Gastrointest Oncol. 6 (5): 112–20. doi:10.4251/wjgo.v6.i5.112. PMC 4021327. PMID 24834141.
- ↑ Matsuura H (2017). "Diffuse Esophageal Spasm: Corkscrew Esophagus". Am. J. Med. doi:10.1016/j.amjmed.2017.08.041. PMID 28943381.
- ↑ Lassen JF, Jensen TM (1992). "[Corkscrew esophagus]". Ugeskr. Laeg. (in Danish). 154 (5): 277–80. PMID 1736462.
- ↑ Ruigómez A, García Rodríguez LA, Wallander MA, Johansson S, Eklund S (2006). "Esophageal stricture: incidence, treatment patterns, and recurrence rate". Am. J. Gastroenterol. 101 (12): 2685–92. doi:10.1111/j.1572-0241.2006.00828.x. PMID 17227515.
- ↑ Shami VM (2014). "Endoscopic management of esophageal strictures". Gastroenterol Hepatol (N Y). 10 (6): 389–91. PMC 4080876. PMID 25013392.
- ↑ López Rodríguez MJ, Robledo Andrés P, Amarilla Jiménez A, Roncero Maíllo M, López Lafuente A, Arroyo Carrera I (2002). "Sideropenic dysphagia in an adolescent". J. Pediatr. Gastroenterol. Nutr. 34 (1): 87–90. PMID 11753173.
- ↑ Chisholm M (1974). "The association between webs, iron and post-cricoid carcinoma". Postgrad Med J. 50 (582): 215–9. PMC 2495558. PMID 4449772.
- ↑ Larsson LG, Sandström A, Westling P (1975). "Relationship of Plummer-Vinson disease to cancer of the upper alimentary tract in Sweden". Cancer Res. 35 (11 Pt. 2): 3308–16. PMID 1192404.