Entamoeba histolytica
|
Amoebiasis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Entamoeba histolytica On the Web |
|
American Roentgen Ray Society Images of Entamoeba histolytica |
| style="background:#Template:Taxobox colour;"|Entamoeba histolytica | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
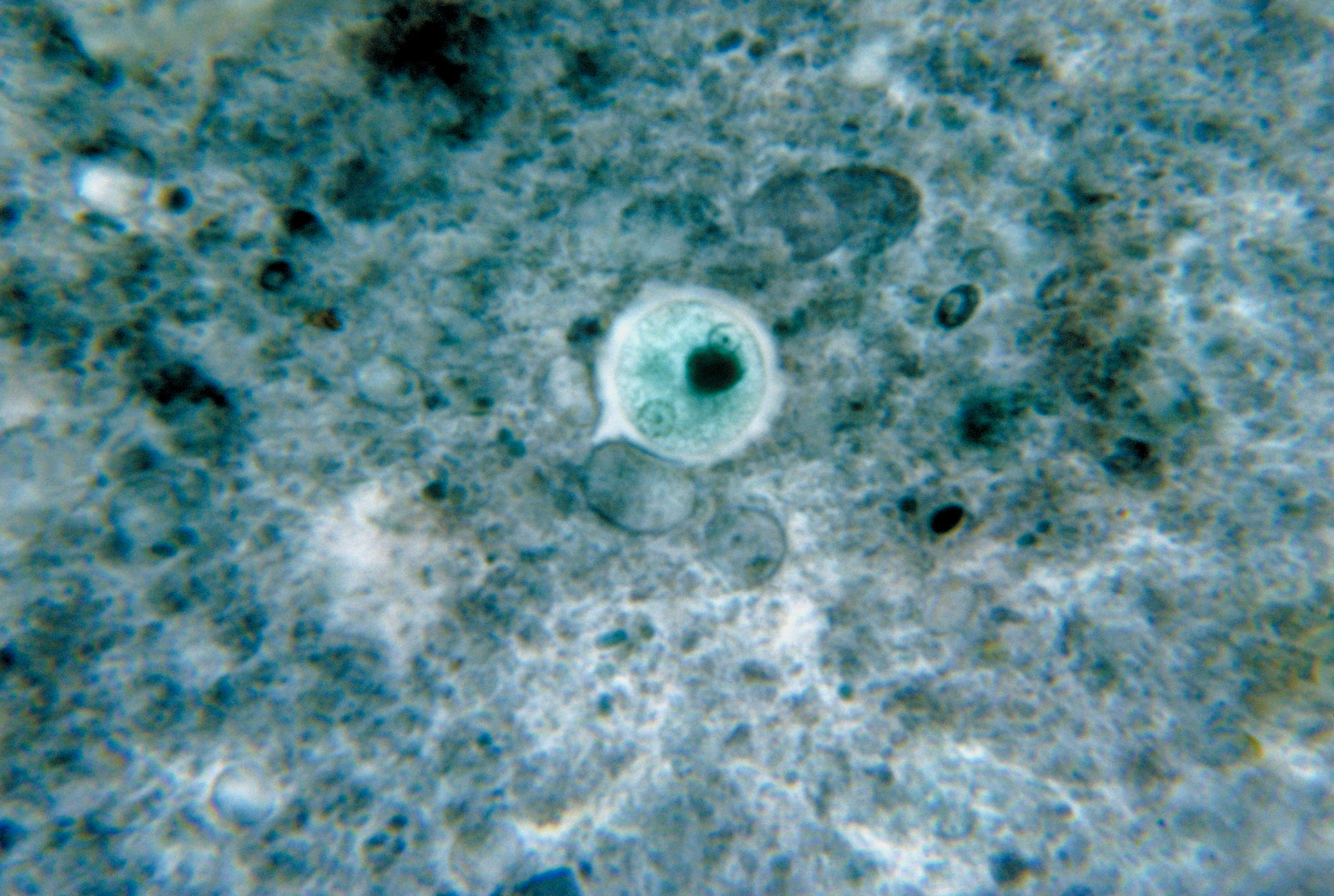 Entamoeba histolytica cyst
| ||||||||||
| style="background:#Template:Taxobox colour;" | Scientific classification | ||||||||||
|
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Jesus Rosario Hernandez, M.D. [2]
Overview
Higher Order Classification
Cellular organisms; Eukaryota; Protista; Amoebozoa; Archamoebae; Entamoeba
Natural Reservoir
- Usually humans (only)
- Reports of animals as natural reservoirs of E. histolytica have been described.
Microbiological Characteristics
| Genus and Species | Entamoeba histolytica |
| Etiologic Agent of: | Amoebiasis; Amoebic dysentery; Extraintestinal Amoebiasis, usually Amoebic Liver Abscess = “anchovy sauce”); Amoeba Cutis; Amoebic Lung Abscess (“liver-colored sputum”) |
| Infective stage | Cyst |
| Definitive Host | Human |
| Portal of Entry | Mouth |
| Mode of Transmission | Ingestion of mature cyst through contaminated food or water |
| Habitat | Colon and Cecum |
| Pathogenic Stage | Trophozoite |
| Locomotive apparatus | Pseudopodia (“False Foot”) |
| Motility | Active, Progressive and Directional |
| Nucleus | 'Ring and dot' appearance: peripheral chromatin and central karyosome |
| Mode of Reproduction | Binary Fission |
| Pathogenesis | Lytic necrosis (it looks like “flask-shaped” holes in Gastrointestinal tract sections (GIT) |
| Type of Encystment | Protective and Reproductive |
| Lab Diagnosis | Most common is Direct Fecal Smear (DFS) and staining (but does not allow identification to species level); Enzyme immunoassay (EIA); Indirect Hemagglutination (IHA); Antigen detection – monoclonal antibody; PCR for species identification. Culture: From faecal samples - Robinson's medium, Jones' medium |
| Treatment | Metronidazole for the invasive trophozoites PLUS a luminal amoebicide for those still in the intestine (Paromomycin is the most widely used) |
| Trophozoite Stage | |
| Pathognomonic/Diagnostic Feature | Ingested RBC; distinctive nucleus |
| Cyst Stage | |
| Chromatoidal Body | 'Cigar' shaped bodies (made up of crystalline ribosomes) |
| Number of Nuclei | 1 in early stages, 4 when mature |
| Pathognomonic/Diagnostic Feature | 'Ring and dot' nucleus and chromatoid bodies |
Genome
Life Cycle
[Image:Amebiasis_LifeCycle.gif]
Retrieved from the Centers for Disease Control and Prevention
- Cysts and trophozoites are passed in human feces. Cysts are typically found in formed stool, whereas trophozoites are typically found in diarrheal stool.
- Infection by Entamoeba histolytica occurs by ingestion of mature cysts in fecally contaminated food, water, or hands.
- Excystation occurs in the small intestine and trophozoites are released, which migrate to the large intestine.
- The trophozoites multiply by binary fission and produce cysts, and both stages are passed in the feces.
- Because of the protection conferred by their walls, the cysts can survive days to weeks in the external environment and are responsible for transmission.
- Trophozoites passed in the stool are rapidly destroyed once outside the body, and if ingested would not survive exposure to the gastric environment.
- In many cases, the trophozoites remain confined to the intestinal lumen (A: noninvasive infection) of individuals who are asymptomatic carriers, passing cysts in their stool.
- In some patients the trophozoites invade the intestinal mucosa (B: intestinal disease), or, through the bloodstream, extraintestinal sites such as the liver, brain, and lungs (C: extraintestinal disease), with resultant pathologic manifestations.
- It has been established that the invasive and noninvasive forms represent two separate species, respectively E. histolytica and E. dispar. These two species are morphologically indistinguishable unless E. histolytica is observed with ingested red blood cells (erythrophagocystosis).
- Transmission can also occur through exposure to fecal matter during sexual contact (in which case not only cysts, but also trophozoites could prove infective).
Gallery
-
Entamoeba histolytica. From Public Health Image Library (PHIL). [1]
-
Entamoeba histolytica. From Public Health Image Library (PHIL). [1]
-
Entamoeba histolytica. From Public Health Image Library (PHIL). [1]
-
Entamoeba histolytica. From Public Health Image Library (PHIL). [1]
-
Entamoeba histolytica. From Public Health Image Library (PHIL). [1]
-
Entamoeba histolytica. From Public Health Image Library (PHIL). [1]
-
Entamoeba histolytica. From Public Health Image Library (PHIL). [1]
-
Entamoeba histolytica. From Public Health Image Library (PHIL). [1]
-
Entamoeba histolytica. From Public Health Image Library (PHIL). [1]
-
Entamoeba histolytica. From Public Health Image Library (PHIL). [1]
-
Entamoeba histolytica. From Public Health Image Library (PHIL). [1]
-
Entamoeba histolytica. From Public Health Image Library (PHIL). [1]
-
Entamoeba histolytica. From Public Health Image Library (PHIL). [1]
![Entamoeba histolytica. From Public Health Image Library (PHIL). [1]](/images/5/5d/Entamoeba_histolytica01.jpeg)
![Entamoeba histolytica. From Public Health Image Library (PHIL). [1]](/images/1/11/Entamoeba_histolytica02.jpeg)
![Entamoeba histolytica. From Public Health Image Library (PHIL). [1]](/images/8/8d/Entamoeba_histolytica03.jpeg)
![Entamoeba histolytica. From Public Health Image Library (PHIL). [1]](/images/e/ec/Entamoeba_histolytica04.jpeg)
![Entamoeba histolytica. From Public Health Image Library (PHIL). [1]](/images/7/74/Entamoeba_histolytica05.jpeg)
![Entamoeba histolytica. From Public Health Image Library (PHIL). [1]](/images/d/d9/Entamoeba_histolytica06.jpeg)
![Entamoeba histolytica. From Public Health Image Library (PHIL). [1]](/images/b/bc/Entamoeba_histolytica07.jpeg)
![Entamoeba histolytica. From Public Health Image Library (PHIL). [1]](/images/2/24/Entamoeba_histolytica08.jpeg)
![Entamoeba histolytica. From Public Health Image Library (PHIL). [1]](/images/e/e0/Entamoeba_histolytica09.jpeg)
![Entamoeba histolytica. From Public Health Image Library (PHIL). [1]](/images/0/0b/Entamoeba_histolytica11.jpeg)
![Entamoeba histolytica. From Public Health Image Library (PHIL). [1]](/images/e/e9/Entamoeba_histolytica12.jpeg)
![Entamoeba histolytica. From Public Health Image Library (PHIL). [1]](/images/2/2b/Entamoeba_histolytica13.jpeg)
![Entamoeba histolytica. From Public Health Image Library (PHIL). [1]](/images/1/10/Entamoeba_histolytica14.jpeg)