Endocarditis pathophysiology: Difference between revisions
No edit summary |
No edit summary |
||
| Line 50: | Line 50: | ||
* The exact pathogenesis of nonbacterial thrombotic endocarditis is not completely understood. | * The exact pathogenesis of nonbacterial thrombotic endocarditis is not completely understood. | ||
*[[Nonbacterial thrombotic endocarditis]] (NBTE), also called '''marantic endocarditis''' is most commonly found on previously undamaged valves. | |||
*The vegetations in nonbacterial thrombotic endocarditis are sterile and small. | |||
*The vegetations mostly aggregate at the edges of the valve or the cusps. | |||
* We can divide the pathogenesis pathway of nonbacterial endocarditis into to phase: | * We can divide the pathogenesis pathway of nonbacterial endocarditis into to phase: | ||
** Initiating phase | ** Initiating phase | ||
| Line 58: | Line 61: | ||
****Some studies demonstrated that hypoxia may lead to tissue factor activation. | ****Some studies demonstrated that hypoxia may lead to tissue factor activation. | ||
****Higher tissue factor level has an association with higher rate of endocarditis. | ****Higher tissue factor level has an association with higher rate of endocarditis. | ||
****Other studies implies that the rate of endocarditis is higher in smokers and patients with chronic lung disease and possibly hypoxia. | ****Other studies implies that the rate of endocarditis is higher in smokers and patients with chronic lung disease and possibly hypoxia. | ||
*** Hypercoagulability<ref name="pmid13403513">{{cite journal |vauthors=MACDONALD RA, ROBBINS SL |title=The significance of nonbacterial thrombotic endocarditis: an autopsy and clinical study of 78 cases |journal=Ann. Intern. Med. |volume=46 |issue=2 |pages=255–73 |date=February 1957 |pmid=13403513 |doi=10.7326/0003-4819-46-2-255 |url=}}</ref><ref name="pmid834136">{{cite journal |vauthors=Sack GH, Levin J, Bell WR |title=Trousseau's syndrome and other manifestations of chronic disseminated coagulopathy in patients with neoplasms: clinical, pathophysiologic, and therapeutic features |journal=Medicine (Baltimore) |volume=56 |issue=1 |pages=1–37 |date=January 1977 |pmid=834136 |doi= |url=}}</ref> | *** Hypercoagulability<ref name="pmid13403513">{{cite journal |vauthors=MACDONALD RA, ROBBINS SL |title=The significance of nonbacterial thrombotic endocarditis: an autopsy and clinical study of 78 cases |journal=Ann. Intern. Med. |volume=46 |issue=2 |pages=255–73 |date=February 1957 |pmid=13403513 |doi=10.7326/0003-4819-46-2-255 |url=}}</ref><ref name="pmid834136">{{cite journal |vauthors=Sack GH, Levin J, Bell WR |title=Trousseau's syndrome and other manifestations of chronic disseminated coagulopathy in patients with neoplasms: clinical, pathophysiologic, and therapeutic features |journal=Medicine (Baltimore) |volume=56 |issue=1 |pages=1–37 |date=January 1977 |pmid=834136 |doi= |url=}}</ref> | ||
****There is an association between hypercoagulable state and clotting factor abnormalities with initiation of nonbacterial thrombotic endocarditis. | ****There is an association between hypercoagulable state and clotting factor abnormalities with initiation of nonbacterial thrombotic endocarditis. | ||
| Line 69: | Line 72: | ||
***** | ***** | ||
** Verrucae formation | ** Verrucae formation | ||
== Genetics == | == Genetics == | ||
Revision as of 16:35, 2 January 2020
| https://https://www.youtube.com/watch?v=kW-85yk0ErQ%7C350}} |
|
Endocarditis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease |
|
Case Studies |
|
Endocarditis pathophysiology On the Web |
|
Risk calculators and risk factors for Endocarditis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Maliha Shakil, M.D. [2]
Overview
The pathogenesis of infective endocarditis includes valvular damage, altered and turbulent flow, bacteremia, and lack of blood supply to the valves. Damaged endothelium becomes a site for attachment of infectious agents in infectious endocarditis. Nonbacterial thrombotic endocarditis is related to hypercoaguable states such as pregnancy or systemic bacterial infection. The characteristic lesion of endocarditis is a vegetation. Vegetations are composed of fibrin, inflammatory cells, platelets, and microorganisms.
Pathophysiology
Pathogenesis
Infective Endocarditis
| Pathogenic Factors | Mechanism |
|---|---|
|
|
|
|
|
|
Nonbacterial Thrombotic Endocarditis
- The exact pathogenesis of nonbacterial thrombotic endocarditis is not completely understood.
- Nonbacterial thrombotic endocarditis (NBTE), also called marantic endocarditis is most commonly found on previously undamaged valves.
- The vegetations in nonbacterial thrombotic endocarditis are sterile and small.
- The vegetations mostly aggregate at the edges of the valve or the cusps.
- We can divide the pathogenesis pathway of nonbacterial endocarditis into to phase:
- Initiating phase
- Immune complexes[3][4]
- circulating immune complexes and complement deposition can initiate the process.
- The example for this initiating factor in libman sacks endocarditis in lupus patients.
- Hypoxia[5][6]
- Some studies demonstrated that hypoxia may lead to tissue factor activation.
- Higher tissue factor level has an association with higher rate of endocarditis.
- Other studies implies that the rate of endocarditis is higher in smokers and patients with chronic lung disease and possibly hypoxia.
- Hypercoagulability[7][8]
- There is an association between hypercoagulable state and clotting factor abnormalities with initiation of nonbacterial thrombotic endocarditis.
- There is an association between hypercoagulable state and clotting factor abnormalities with initiation of nonbacterial thrombotic endocarditis.
- Carcinomatosis[9]
- The association between cancer and nonbacterial thrombotic endocarditis is well established.
- In most of the cases of cancer related endocarditis we have abnormal activity of tissue factor.
- Tissue factor may be secreted from promyelocytic leukaemia cells.
- Tissue factor may be expressed on the surface of adenocarcinoma cells which leads to increased expression of tissue factor by endothelial cells.
- Immune complexes[3][4]
- Verrucae formation
- Initiating phase
Genetics
Associated Conditions
Gross Pathology
Microscopic Pathology
Gross and Microscopic Pathology
The characteristic lesion of endocarditis is a vegetation. Vegetations are composed of fibrin, inflammatory cells, platelets, and microorganisms.[10] Characteristic features of endocarditis on gross pathology and histopathological analysis include:[11]
| Endocarditis Subtype | Features on Gross Pathology | Features on Histopathological Microscopic Analysis |
| Infective Endocarditis |
|
|
| Nonbacterial Thrombotic Endocarditis |
|
|
-
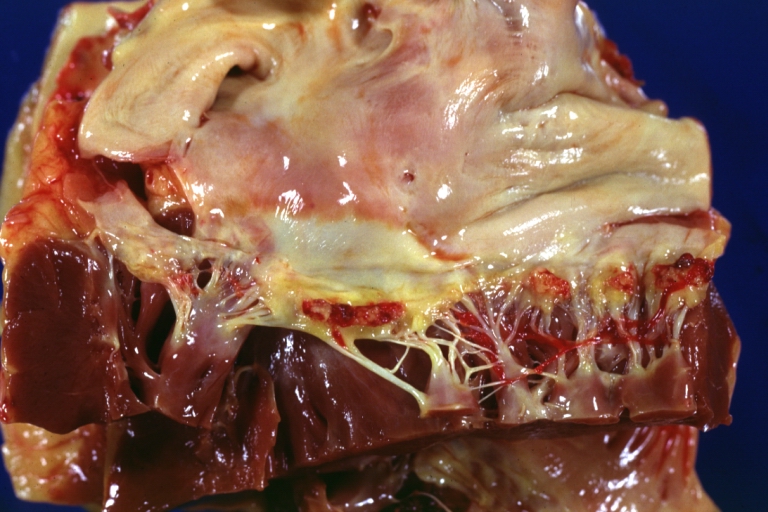
Heart; Breast intraductal papilloma metastasis. Thrombotic Nonbacterial Endocarditis (Infected): Gross mitral valve natural color vegetations well illustrated these were secondarily infected with staphylococcus case of 8 year survival breast intraductal papillary adenocarcinoma with extensive metastases. Aortic valve also involved.
-
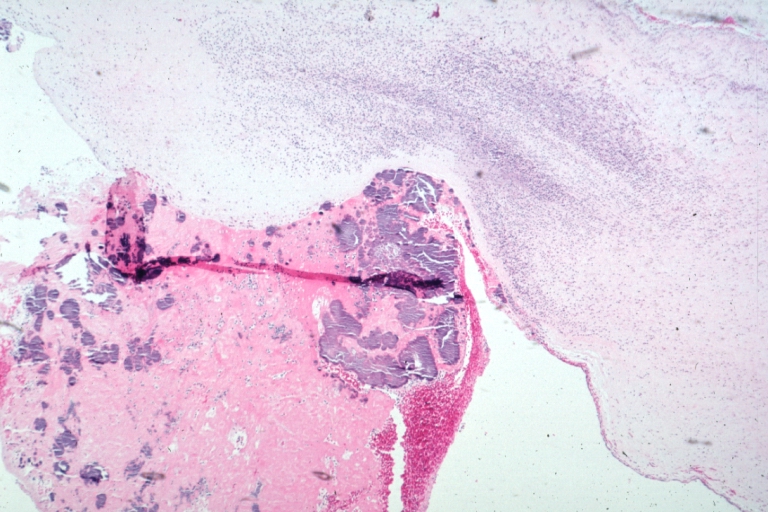
Nonbacterial Thrombotic Endocarditis Infected: Micro low mag H&E fibrin vegetation with masses of staphylococci and inflammatory cells in valve secondarily infected case 8 year survival breast papillary intraductal adenocarcinoma with extensive metastases gross is aortic valve lesions.
Videos
{{#ev:youtube|gk7cpP2ymOs}} {{#ev:youtube|BiNulEFh6rU}}
References
- ↑ Infective endocarditis. Wikipedia (2015). https://en.wikipedia.org/wiki/Infective_endocarditis#Pathogenesis Accessed on September 21, 2015
- ↑ Endocarditis. Wikipedia (2015). https://en.wikipedia.org/wiki/Endocarditis Accessed on September 21, 2015
- ↑ Ford PM, Ford SE, Lillicrap DP (April 1988). "Association of lupus anticoagulant with severe valvular heart disease in systemic lupus erythematosus". J. Rheumatol. 15 (4): 597–600. PMID 3135393.
- ↑ Williams, Ralph (1980). Immune complexes in clinical and experimental medicine. Cambridge, Mass: Harvard University Press. ISBN 978-0674444386.
- ↑ Nakanishi K, Tajima F, Nakata Y, Osada H, Ogata K, Kawai T, Torikata C, Suga T, Takishima K, Aurues T, Ikeda T (October 1998). "Tissue factor is associated with the nonbacterial thrombotic endocarditis induced by a hypobaric hypoxic environment in rats". Virchows Arch. 433 (4): 375–9. doi:10.1007/s004280050262. PMID 9808440.
- ↑ Truskinovsky AM, Hutchins GM (April 2001). "Association between nonbacterial thrombotic endocarditis and hypoxigenic pulmonary diseases". Virchows Arch. 438 (4): 357–61. doi:10.1007/s004280000372. PMID 11355169.
- ↑ MACDONALD RA, ROBBINS SL (February 1957). "The significance of nonbacterial thrombotic endocarditis: an autopsy and clinical study of 78 cases". Ann. Intern. Med. 46 (2): 255–73. doi:10.7326/0003-4819-46-2-255. PMID 13403513.
- ↑ Sack GH, Levin J, Bell WR (January 1977). "Trousseau's syndrome and other manifestations of chronic disseminated coagulopathy in patients with neoplasms: clinical, pathophysiologic, and therapeutic features". Medicine (Baltimore). 56 (1): 1–37. PMID 834136.
- ↑ Gralnick HR, Abrell E (January 1973). "Studies of the procoagulant and fibrinolytic activity of promyelocytes in acute promyelocytic leukaemia". Br. J. Haematol. 24 (1): 89–99. doi:10.1111/j.1365-2141.1973.tb05730.x. PMID 4577065.
- ↑ Mylonakis E, Calderwood SB (2001). "Infective endocarditis in adults". N Engl J Med. 345 (18): 1318–30. doi:10.1056/NEJMra010082. PMID 11794152.
- ↑ Infective Endocarditis. Libre Pathology (2015). URL=http://librepathology.org/wiki/index.php/Infective_endocarditis Accessed on September 21, 2015