Endocarditis echocardiography and ultrasound
|
Endocarditis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease |
|
Case Studies |
|
Endocarditis echocardiography and ultrasound On the Web |
|
to Hospitals Treating Endocarditis echocardiography and ultrasound |
|
Risk calculators and risk factors for Endocarditis echocardiography and ultrasound |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
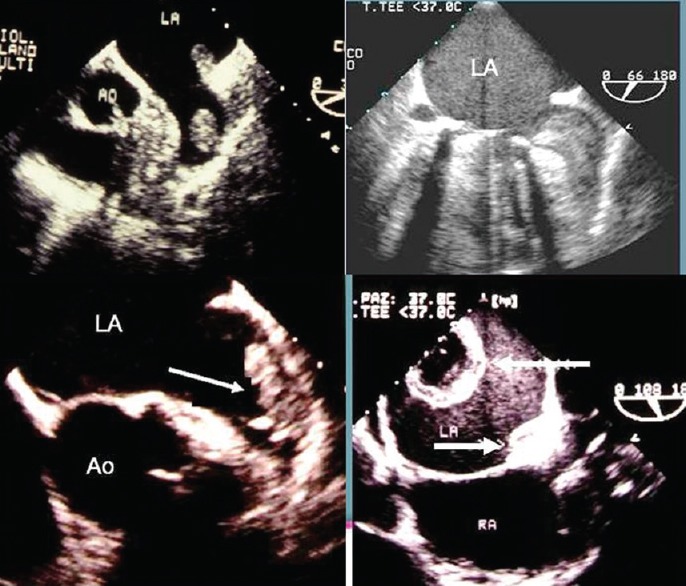
Echocardiography may be diagnostic of endocarditis. Echocardiography allows detection of microbial vegetations and the degree of valvular dysfunction. Findings on transthoracic and transesophageal echocardiogram diagnostic of endocarditis include vegetations, valvular regurgitation, pseudoaneurysms, paravalvular abscess, and fistulas. The role of electrocardiography has been addressed in clinical practice guidelines from theAmerican Heart Association, with endorsement by the Infectious Diseases Society of America, have been updated in 2015.
Echocardiography/Ultrasound
Echocardiography
The goals of echocardiography in the patient with endocarditis include the following:[1][2][3]
- Determine the presence, location and size of vegetations
- Assess the damage to the valve apparatus and determine the magnitude of regurgitation, perforation or leak
- To assess the dimensions and function of the ventricle(s)
- To identify any abscess formation
- To determine the need for surgical intervention
Echocardiographic Features in Infective Endocarditis
- Irregular echogenic mass attached to valve leaflet
- The attachment of the vegetation is on the upstream side of the valve leaflet
- There is chaotic independent movement of the mass relative to the valve
- The minimum size of a vegetation that is identifiable on transthoracic echocardiography is 3 mm and by transoesophageal echocardiography route is 2 mm.
- With treatment and time, the vegetation shrinks and can become fibrosed or calcified. It may not disappear completely.
- Large vegetations occur with fungal endocarditis or Staphylococcus aureus endocarditis.
- The hemodynamic effects are mostly due to valvular regurgitation as a result of valve destruction.
The valve and the surrounding anatomy should be carefully inspected for the following complications:
- Fistula
- Perforation
- Prosthetic dehiscence
- Aneurysm
- Vegetations
- Valve ulcers or erosions
- Rupture of chordaes
- Endocardial jet lesions
- Flail leaflets or cusps
- Abscess formation (annular and ring)
Transesophageal Echocardiography (TEE) vs. Transthoracic Echocardiography (TTE)
- In general, transthoracic echocardiography (TTE) is often adequate for the diagnosis of infective endocarditis in cases where cardiac structures-of-interest are well visualized.
- The transthoracic echocardiogram has a sensitivity and specificity of approximately 65% and 95% if the echocardiographer believes there is 'probable' or 'almost certain' evidence of endocarditis.[4][5]
Specific situations where transesophageal echocardiography (TEE) is preferred over TTE include:
- The presence of a prosthetic valve
- Poor transthoracic views
- Continuing sepsis despite adequate antibiotic therapy
- New PR prolongation
- No signs of endocarditis on transthoracic echocardiography, but high clinical suspicion
- Suspected periannular complications
- Children with complex congenital cardiac lesions
- Patients with S. Aureus caused bacteremia and pre-existing valvular abnormalities that make TTE interpretation more difficult (e.g. calcific aortic stenosis).
Video Examples
{{#ev:youtube|v6VGccGETQA}}
Other Imaging Findings
- Various radionuclide scans using, for example, gallium Ga 67–tagged white cells and indium in 111–tagged white cells, have proven to be of little use in diagnosing IE.
- Radionuclide scans of the spleen are useful to help rule out a splenic abscess, which is a cause of bacteremia that is refractory to antibiotic therapy.
Sources
- 2008 Focused Update Incorporated Into the ACC/AHA 2006 Guidelines for the Management of Patients With Valvular Heart Disease [7]
References
- ↑ Hoen B, Duval X (2013). "Clinical practice. Infective endocarditis". N Engl J Med. 368 (15): 1425–33. doi:10.1056/NEJMcp1206782. PMID 23574121.
- ↑ Baddour LM, Wilson WR, Bayer AS, Fowler VG, Tleyjeh IM, Rybak MJ; et al. (2015). "Infective Endocarditis in Adults: Diagnosis, Antimicrobial Therapy, and Management of Complications: A Scientific Statement for Healthcare Professionals From the American Heart Association". Circulation. 132 (15): 1435–86. doi:10.1161/CIR.0000000000000296. PMID 26373316.
- ↑ Endocarditis. Wikipedia (2015). URL= https://en.wikipedia.org/wiki/Endocarditis Accessed on September 21, 2015
- ↑ Shively B, Gurule F, Roldan C, Leggett J, Schiller N (1991). "Diagnostic value of transesophageal compared with transthoracic echocardiography in infective endocarditis". J Am Coll Cardiol. 18 (2): 391–7. PMID 1856406.
- ↑ Erbel R, Rohmann S, Drexler M, Mohr-Kahaly S, Gerharz C, Iversen S, Oelert H, Meyer J (1988). "Improved diagnostic value of echocardiography in patients with infective endocarditis by transoesophageal approach. A prospective study". Eur Heart J. 9 (1): 43–53. PMID 3345769.
- ↑ "The Evolving Role and Use of Echocardiography in the Evaluation of Cardiac Source of Embolism".
- ↑ Bonow RO, Carabello BA, Chatterjee K; et al. (2008). "2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons". Circulation. 118 (15): e523–661. doi:10.1161/CIRCULATIONAHA.108.190748. PMID 18820172. Unknown parameter
|month=ignored (help)