Cysticercosis overview
|
Cysticercosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Cysticercosis overview On the Web |
|
American Roentgen Ray Society Images of Cysticercosis overview |
|
Risk calculators and risk factors for Cysticercosis overview |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Ahmed Younes M.B.B.CH [2]
Overview
- Cysticercosis is an infection caused by the larval stages of the parasite Taenia solium, after a person ingests tapeworm eggs. The larvae embed in tissues such as muscle and brain, forming cysticerci (cysts).
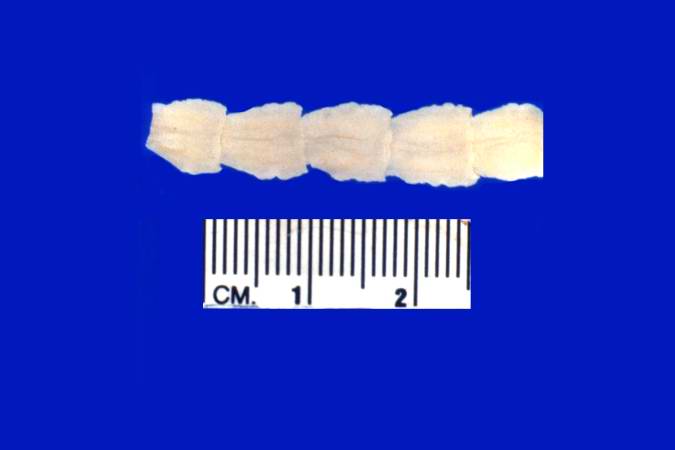
Adult Taenia Solium - © Copyright UAB and the UAB Research Foundation, 1999-2013. All rights reserved
Historical Perspective
- The earliest reference to tapeworms was found in the works of ancient Egyptians that date back to almost 2000 BC.[1].Cysticercosis is caused by the infestation of the larvae of Taenia Solium to various tissues (Brain, Muscles, eye .. etc).
Pathophysiology
- Humans develop cysticercosis by ingesting Taenia solium eggs. Following ingestion, oncospheres hatch, have access to the circulation and infect various tissues. During the viable phase, cysts do not cause marked inflammation nor symptoms. As the cysts degenerate, they lose the ability to modulate the immune response and result in an immune attack and tissue injury and edema. Eventually, the cysts either resolve or form a calcified granuloma, which is associated with seizures if it is located in the brain.
Classification
- Cysticercosis is classified according to the site of cysticerci into Neurocysticercosis and extraneural cysticercosis. Neurocysticercosis is further subdivided into Parenchymal and extra-parenchymal.
Epidemiology and Demographics
- Cysticercosis is more prevalent in underdeveloped countries in Africa, Latin America and Southeast Asia, especially in rural areas where humans are in direct contact with pigs and sanitary conditions, are not optimum.
Risk Factors
- Poor sanitary habits, contact with pigs and living in an endemic area are the main risk factors for having cysticercosis.
Screening
- Patients with cysticercosis and their household should be screened for intestinal tapeworm. High-risk persons should be screened for cysticercosis if they are to be employed as food handlers or housekeepers.
Natural History, Complications and Prognosis
- Cysticercosis is treated easily with antihelminthic drugs and even untreated patients can remain silent for long periods. Complications can develop in the intestine if the tapeworm grows enough to cause obstructions or at the sites of cysticerci when they start to degenerate and provoke the immune system.
Symptoms and Physical Examination
- Presenting symptoms differ according to the site of the cysticerci. Parenchymal neurocysticercosis causes all the symptoms and signs of space occupying lesions. Extraparenchymal neurocysticercosis causes manifestations of increased intracranial pressure if cysts are present in the subarachnoid space or in the ventricles, manifestations of spinal cord compression if present in the spinal cord or causes eye disease if cysts are present in the orbit.
Diagnostic tests
- There is no single gold standard for diagnosing cysticercosis (except for biopsy which is rarely done). Diagnosis is made by combing data from various investigation and suspecting the disease. A set of diagnostic criteria was proposed in 2001 based on a combination of epidemiological factors, clinical manifestations, laboratory and radiological investigations.
- Computerized tomography (CT) is superior to magnetic resonance imaging (MRI) for demonstrating small calcifications. However, MRI shows cysts in some locations (cerebral convexity, ventricular ependyma) better than CT, is more sensitive than CT to demonstrate surrounding edema and may show internal changes indicating the death of cysticerci.
Treatment
- Cysticercosis is generally treated with a combination of both anti-parasitic drugs and anti-inflammatory drugs. Symptomatic treatment is the mainstay therapy for neurocysticercosis. Surgical removal is sometimes necessary to treat ophthalmic cysticercosis and subcutaneous cysticercosis.
- Surgery is not the first line of treatment except in ocular cysticercosis and other certain cases of neurocysticercosis.
Primary Prevention
- Prevention against intestinal taeniasis is the main strategy for prevention of cysticercosis.
References
- ↑ Wadia, NH, Singh, G. “Taenia Solium: A Historical Note” Taenia Solium Cysticercosis: From Basic to Clinical Science CABI Publishing, 2002. 157-168.