Craniosynostosis
| Craniosynostosis | |
 | |
|---|---|
| Child with premature closure (craniosynostosis) of the lambdoid suture. Notice the swelling on the right side of the head | |
| ICD-10 | Q75.0 |
| ICD-9 | 756.0 |
| OMIM | 218500 |
| DiseasesDB | 3160 |
| MeSH | D003398 |
For patient information click here
|
WikiDoc Resources for Craniosynostosis |
|
Articles |
|---|
|
Most recent articles on Craniosynostosis Most cited articles on Craniosynostosis |
|
Media |
|
Powerpoint slides on Craniosynostosis |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Craniosynostosis at Clinical Trials.gov Trial results on Craniosynostosis Clinical Trials on Craniosynostosis at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Craniosynostosis NICE Guidance on Craniosynostosis
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Craniosynostosis Discussion groups on Craniosynostosis Patient Handouts on Craniosynostosis Directions to Hospitals Treating Craniosynostosis Risk calculators and risk factors for Craniosynostosis
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Craniosynostosis |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Craniosynostosis,[1] is a medical condition in which some or all of the sutures in the skull of an infant or child close too early, causing problems with normal brain and skull growth. It can result in craniostenosis, which is the skull deformity caused by the premature closure of the cranial sutures. Also intracranial pressure can be increased.
Normal skull development
In humans, the adult skull is normally made up of 28 bones. The flat bones making up the cranial vault are joined together by sutures: rigid articulations permitting very little movement.
At birth, the human skull is made up of 45 separate bony elements. As growth occurs, many of these bony elements gradually fuse together into solid bone (for example, the frontal bones).
The bones of the roof of the skull are initially separated by regions of dense connective tissue. At birth these regions are fibrous and moveable, necessary for birth and later growth. Larger regions of connective tissue, called fontanelles, occur where certain bony elements meet. As growth and ossification progress, the connective tissue of the fontanelles is invaded and replaced by bone. The posterior fontanelle usually closes by eight weeks, but the anterior fontanelle can remain up to eighteen months.
Classification
Primary synostosis is subdivided into syndromic (familial or hereditary) and the more common nonsyndromic (isolated and sporadic). Premature fusion of the sutures may be isolated or form part of a syndrome, including Crouzon syndrome, Apert syndrome, and Pfeiffer syndrome.
Secondary synostoses are encountered in a variety of unrelated conditions, including metabolic derangements such as hypophosphatasia and rickets, bone dysplasias] such as mucopolysaccharidoses and thanatophoric dysplasia, and effects of fetal teratogens (i.e. hydantoin). Secondary sutural closure occurs after ventriculoperitoneal shunting, when reduction in ventricular size reduces the expansile forces on the calvaria. When sutures fuse prematurely, head growth occurs along the axis of the fused suture. The altered skull shape is diagnostic.
Scaphocephaly and Dolichocephaly indicate calvarial elongation in the anteroposterior diameter.
- Results from premature sagittal synostosis.
- Most common type of synostosis, accounting for up to 50% of cases
- More common in males.
- Frequently inherited as an autosomal dominant trait.
Brachycephaly indicates abnormal calvarial widening in the transverse diameter.
- Typically arises when coronal or lambdoid synostosis limits anteroposterior growth.
- The ipsilateral frontal bone is flattened and the orbit is deformed with elevation of its superior lateral angle, resulting in the harlequin eye.
Plagiocephaly occurs with unilateral coronal synostosis or asynchronous synostoses of multiple sutures bilaterally.
- Asymmetric growth results in displacement of the sagittal suture, nasal septum, and skull base to the affected side.
Trigonocephalyoccurs with synostoses of the metopic suture.
Cloverleaf skull (kleeblattschaedel) develops when there is premature synostosis of all except the squamosal suture.
- This configuration may be seen with severe Apert or Crouzon syndrome or with thanatophoric dysplasia.
Pathophysiology
When one or more sutures fuse prematurely, skull growth can be restricted perpendicular to the suture. If multiple sutures fuse while the brain is still increasing in size, intracranial pressure can increase.
Primary craniosynostosis is believed to be a result of primary defect in the mesenchymal layer ossification in the cranial bones. Secondary craniosynostosis is a result of primary failure of brain growth.
Diagnosis
Physicians diagnose craniosynostosis through physical examination, plain x-rays, and CT scans. [2]
Syndromes
Craniosynostosis often occurs alone, however about 20% of cases are associated with syndromes. A syndrome is diagnosed by considering the presence of a variety of features, signs, and symptoms throughout the body. Genetic testing may be available to confirm the diagnosis of a specific syndrome. A family history of abnormal head shape can sometimes be found with genetic syndromes, though many syndromes are caused by new genetic mutations, and there is no family history of the disorder. [2]
The most common causes of syndromic craniosynostosis are Crouzon syndrome and Apert syndrome. However, there are over 150 syndromes associated with craniosynostosis. [2] The following table lists some of the craniosynostosis syndromes, as well as prominent additional symptoms that are found in these syndromes — this is not a comprehensive list of all symptoms that could occur within each syndrome. There is considerable overlap of symptoms between many of these syndromes, and clinical evaluation by a geneticist may be necessary to determine the most appropriate diagnosis.
| Name of syndrome | Other signs and symptoms (along with craniosynostosis; may not all be present) | OMIM reference |
|---|---|---|
| Crouzon syndrome | wide-set, bulging eyes • beaked nose • flat face | 123500 |
| Apert syndrome | fused fingers or toes • flat midface | 101200 |
| Crouzonodermoskeletal syndrome | wide-set, bulging eyes • beaked nose • flat face • dark, velvety skin folds • spine abnormalities • benign growths in the jaw | 134934 |
| Jackson-Weiss syndrome | enlarged, bent big toes • flat midface | 123150 |
| Loeys-Dietz syndrome | wide-set eyes • split uvula or cleft palate • arterial tortuosity • aneurysms | 609192 |
| Muenke syndrome | coronal synostosis • skeletal abnormalities of the hands or feet • hearing loss | 602849 |
| Pfeiffer syndrome | broad, short thumbs or big toes • webbed or fused fingers or toes | 101600 |
| Saethre-Chotzen syndrome | facial asymmetry • low frontal hairline • drooping eyelids • webbed fingers or toes • broad big toes | 101400 |
| Shprintzen-Goldberg syndrome | bulging eyes • flat face • hernias • long, thin fingers • developmental delay • mental retardation | 182212 |
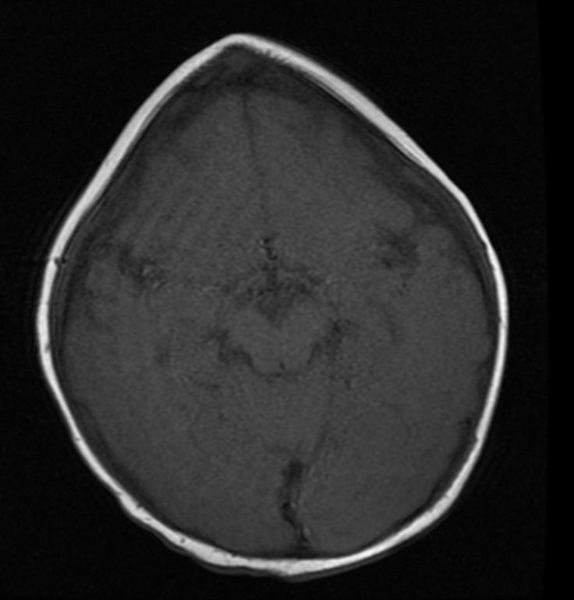
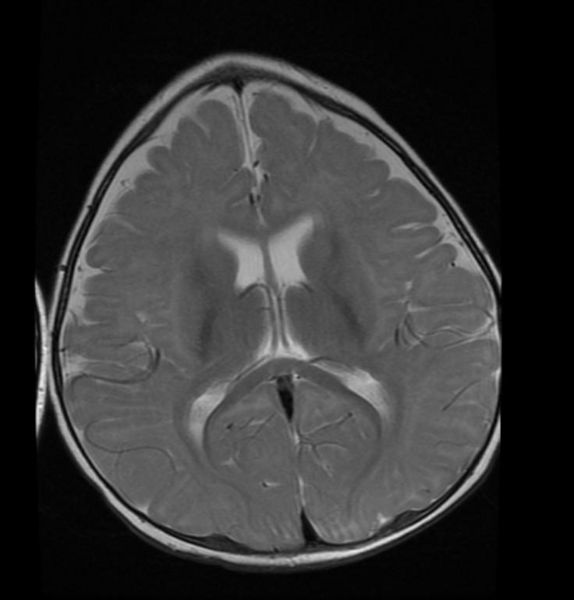
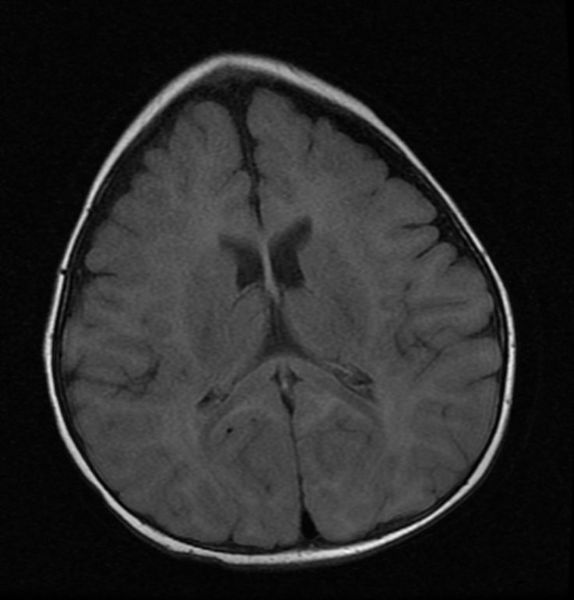
MRI images demonstrate trigonocephaly
Differential diagnosis
A separate cause of abnormal head shape is positional plagiocephaly — flattened or misshapen areas on the head that may develop due to sleeping position. While the appearance may look rather similar to craniosynostosis, the distinction is important. Positional plagiocephaly does not require surgery — treatment can be as simple as occasionally repositioning the child's head while sleeping or, in some cases, wearing a cranial band to mold the skull. [2]

Treatment
Surgery is typically used to separate the fused sutures of the skull as well as to reshape the skull. To treat the cosmetic troubles, a combination of orthodontic and orthognathic surgery can be used to relieve some of the midface deficiency.
Typical surgery begins with a zigzag incision from ear to ear across the top of the head. The scar left by this type of incision makes the hair look more natural than that left by a straight incision would. Leroy clips are typically used to curtail bleeding, as cauterization would not result in an aesthetically pleasing result upon healing. Once the scalp is peeled back, pilot holes are drilled through the skull. These pilot holes are then connected, separating the skull into several pieces. Once reshaped, these pieces are placed back on the head (typically in an altered configuration) and held together by a combination of dissolving sutures, plates, and screws. These plates and screws are typically composed of a copolymer comprised of polyglycolic and polylactic acid and will break down into water and carbon dioxide within a year. Demineralized bone matrix or bone morphogenetic proteins are often used to fill gaps left by the expanded skull, encouraging the body to grow new bone in a process called intramembranous ossification. Once the hemostatic scalp clips are removed, sutures are again used to close the incision.
Newer approaches include minimally invasive endoscopic assisted removal of the closed suture followed by treatment with custom made molding helmets. These surgeries are associated with significantly less blood loss, swelling, hospital length of stay and pain. The results have been excellent in the majority of patients treated this way. Endoscopic surgery, however, is indicated only for very young infants(< 6 months of age). Older children require the more extensive surgery described above.
Epidemiology
In the United States, the incidence of craniosynostosis is estimated to be 1 in 2000–3000 live births.
See also
- Cephalic disorder
- Positional plagiocephaly (flattened head syndrome)
External links
- Headlines Support Group — British based support group for Craniosynostosis
- Craniosynostosis — comprehensive overview (American Family Physician)
- Single Suture Craniosynostoses (The Craniofacial Center in Dallas, Texas)
- Cranio Kids — craniosynostosis support
- An adult survivor's perspective
- Photo Gallery Results of less invasive craniosynostosis procedure performed at University Health System, San Antonio, TX
- Cranio Support Web Page - Midwest Craniosynostosis story and support web page
References
- ↑ Silva, Sandra (1999-06-07). "Cloverleaf skull or kleeblattschadel". TheFetus.net. MacroMedia. Retrieved 2007-02-03. Unknown parameter
|coauthors=ignored (help) - ↑ 2.0 2.1 2.2 2.3
Kabbani H (2004 Jun 15). "Craniosynostosis". American Family Physician. 69 (12): 2863–70. PMID 15222651. Unknown parameter
|coauthors=ignored (help); Check date values in:|date=(help)
de:Kraniosynostose nl:Craniosynostose Template:Jb1 Template:WH Template:WS