|
|
| (12 intermediate revisions by 2 users not shown) |
| Line 1: |
Line 1: |
| | __NOTOC__ |
| {{Infobox Disease | | | {{Infobox Disease | |
| Name = Cerebral hypoxia | | | Name = Cerebral hypoxia | |
| Line 7: |
Line 8: |
| {{CMG}} | | {{CMG}} |
|
| |
|
| | '''For patient information, click [[Cerebral hypoxia (patient information)|here]].''' |
|
| |
|
| | {{SK}} Hypoxic encephalopathy; anoxic encephalopathy |
|
| |
|
| :''This article is about "cerebral hypoxia". For other uses of the term "hypoxia", see [[hypoxia]].''
| | ==[[Cerebral hypoxia overview|Overview]]== |
|
| |
|
| ==Diagnostic Findings== | | ==[[Cerebral hypoxia historical perspective|Historical Perspective]]== |
|
| |
|
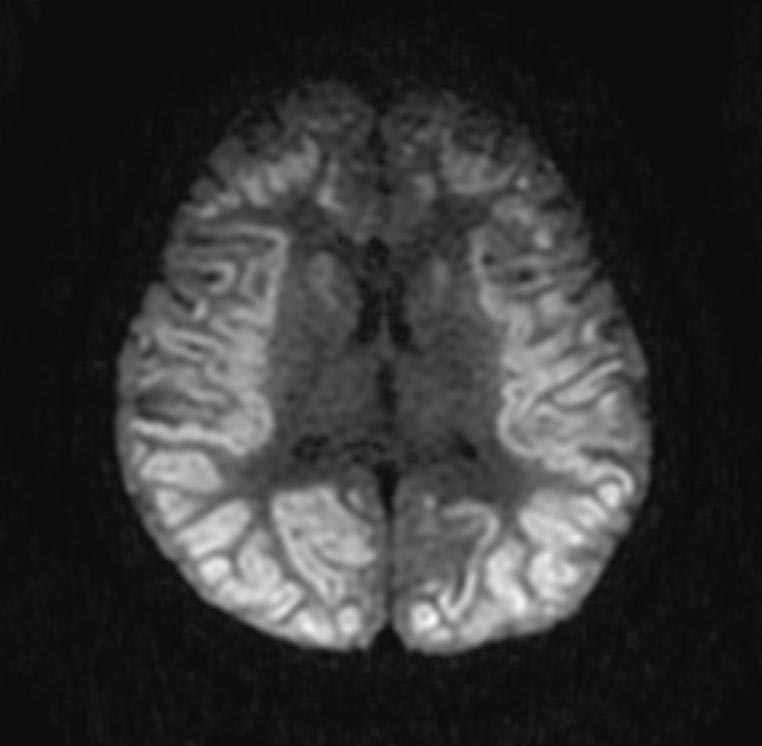
| *Diffuse loss of gray/white differentiation
| | ==[[Cerebral hypoxia classification|Classification]]== |
| *Diffuse sulcal effacement
| |
|
| |
|
| '''Patient #1: '''
| | ==[[Cerebral hypoxia pathophysiology|Pathophysiology]]== |
|
| |
|
| [http://www.radswiki.net Images courtesy of RadsWiki] | | ==[[Cerebral hypoxia causes|Causes]]== |
|
| |
|
| <gallery>
| | ==[[Cerebral hypoxia differential diagnosis|Differentiating Cerebral hypoxia from other Diseases]]== |
| Image:Anoxic-brain-injury-001.jpg
| |
| Image:Anoxic-brain-injury-002.jpg
| |
| </gallery>
| |
|
| |
|
| <gallery>
| | ==[[Cerebral hypoxia risk factors|Risk Factors]]== |
| Image:Anoxic-brain-injury-003.jpg
| |
| Image:Anoxic-brain-injury-004.jpg
| |
| </gallery>
| |
|
| |
|
| '''Patient #2: '''
| | ==[[Cerebral hypoxia natural history, complications and prognosis|Natural History, Complications and Prognosis]]== |
|
| |
|
| [http://www.radswiki.net Images courtesy of RadsWiki]
| | ==Diagnosis== |
|
| |
|
| <gallery>
| | [[Cerebral hypoxia history and symptoms|History and Symptoms]] | [[Cerebral hypoxia physical examination|Physical Examination]] | [[Cerebral hypoxia laboratory findings|Laboratory Findings]] | [[Cerebral hypoxia electrocardiogram|EKG]] | [[Cerebral hypoxia CT|CT]] | [[Cerebral hypoxia MRI|MRI]] | [[Cerebral hypoxia echocardiography or ultrasound|Echocardiography or Ultrasound]] | [[Cerebral hypoxia other imaging findings|Other Imaging Findings]] | [[Cerebral hypoxia other diagnostic studies|Other Diagnostic Studies]] |
| Image:Diffuse-hypoxic-ischemia-001.jpg|DWI
| |
| Image:Diffuse-hypoxic-ischemia-002.jpg|DWI
| |
| </gallery>
| |
|
| |
|
| <gallery>
| | ==Treatment== |
| Image:Diffuse-hypoxic-ischemia-003.jpg|DWI
| |
| Image:Diffuse-hypoxic-ischemia-004.jpg|DWI
| |
| </gallery>
| |
|
| |
|
| <gallery>
| | [[Cerebral hypoxia medical therapy|Medical Therapy]] | [[Cerebral hypoxia primary prevention|Primary Prevention]] | [[Cerebral hypoxia secondary prevention|Secondary Prevention]] | [[Cerebral hypoxia cost-effectiveness of therapy|Cost-Effectiveness of Therapy]] | [[Cerebral hypoxia future or investigational therapies|Future or Investigational Therapies]] |
| Image:Diffuse-hypoxic-ischemia-005.jpg|FLAIR
| |
| Image:Diffuse-hypoxic-ischemia-006.jpg|FLAIR
| |
| Image:Diffuse-hypoxic-ischemia-007.jpg|T1 with GAD
| |
| </gallery>
| |
|
| |
|
| == Treatment == | | ==Case Studies== |
| The first goal of treatment is to restore oxygen to the brain. The method of restoration depends on the cause of the hypoxia.<ref>{{cite web | url = http://neurology.health-cares.net/cerebral-hypoxia.php | title = Cerebral hypoxia | accessdate = 2007-04-13 | publisher = Health-cares.net}}</ref><!--is this a reliable source?--> For mild to moderate cases of hypoxia, removal of the cause of hypoxia may be sufficient. Inhaled oxygen may also be provided. In severe cases treatment may also involve life support and damage control measures.
| | [[Cerebral hypoxia case study one|Case #1]] |
|
| |
|
| A deep coma will interfere with body’s breathing reflexes even after the initial cause of hypoxia has been dealt with. [[Mechanical ventilation]] may be required. Additionally severe cerebral hypoxia causes an elevated heart rate. In extreme cases the heart may tire and stop pumping. [[CPR]], defibrilation, [[epinephrine]], and [[atropine]] may all be tried in an effort to get the heart to resume pumping.<ref name="MIEMSS"/>
| | ==Related Chapters== |
| | |
| Severe cerebral hypoxia can also cause [[seizures]]. Seizures put the patient at risk of self injury. If convulsions are sufficiently severe medical professionals may not be able to provide medical treatment. Various [[anti-convulsant]] drugs may need to be administered before treatment can continue.
| |
| | |
| Brain damage can occur both during and after oxygen deprivation. During oxygen deprivation, cells die due to an increasing acidity in the brain tissue ([[acidosis]]). Additionally, during the period of oxygen deprivation, materials that can easily create [[free radicals]] build up. When oxygen enters the tissue these materials interact with oxygen to create high levels of oxidants. Oxidants interfere with the normal brain chemistry and cause further damage. This is called [[reperfusion injury]].
| |
| | |
| Techniques for preventing damage to brain cells are an area of on-going research. Controlled [[hypothermia]], anti-oxidant drugs, control of [[blood glucose]] levels, and hemodilution (thinning of the blood) coupled with drug-induced hypertension are some treatment techniques currently under investigation.<ref name="Richmond">Richmond TS (May 1997). "Cerebral Resuscitation after Global Brain Ischemia". ''AACN Clinical Issues'' '''8''' (2). Retrieved on 2007-04-13. [http://www.aacn.org/AACN/jrnlci.nsf/0/a522e8311772eca188256576007821ab?OpenDocument Free full text] at the American Association of Critical-Care Nurses website.</ref>
| |
| | |
| In severe cases it is extremely important to act quickly. Brain cells are very sensitive to reduced oxygen levels. Once deprived of oxygen they will begin to die off within five minutes.<ref name="Richmond"/>
| |
| | |
| == Prognosis ==
| |
| | |
| Mild and moderate cerebral hypoxia generally has no impact beyond the episode of hypoxia. Severe cerebral hypoxia is another matter. Outcome will depend on the success of damage control measures, the amount of brain tissue deprived of oxygen, and the speed with which oxygen was restored to the brain.
| |
|
| |
| If cerebral hypoxia was localized to a specific part of the brain, brain damage will be localized to that region. The long term effects will depend on the purpose of that portion of the brain. Damage to the Broca and [[Wernicke]]’s areas of the brain (left side) typically causes problems with speech and language. Damage to the right side of the brain may interfere with the ability to express emotions or interpret what one sees. Damage on either side can cause paralysis of the opposite side of the body.
| |
| | |
| The effects of certain kinds of severe generalized hypoxias may take time to develop. For example, the long term effects of serious carbon monoxide poisoning usually may take several weeks to appear. Recent research suggests this may be due to an autoimmune response caused by CO induced changes in the myelin sheath surrounding neurons.<ref>{{cite news | url = http://www.sciencedaily.com/releases/2004/09/040906083815.htm | title = Long-term Effects Of Carbon Monoxide Poisoning Are An Autoimmune Reaction | author = University Of Pennsylvania Medical Center | date = September 6, 2004 | accessdate = 2007-04-13 | publisher = ScienceDaily}}</ref>
| |
| | |
| If hypoxia results in coma, the length of unconsciousness is often used as an indication of long term damage. In some cases coma can give the brain an opportunity to heal and regenerate,<ref>{{cite news | url = http://www.newscientist.com/article.ns?id=dn9474&feedId=brain_rss20 | title = 'Rewired brain' revives patient after 19 years | last = Phillips | first = Helen | date = July 3, 2006 | accessdate = 2007-04-13 | publisher = New Scientist}}</ref> but, in general, the longer a coma continues the greater the likelihood that the person will remain in a vegetative state until death.<ref name="NINDS"/> Even if the patient wakes up, brain damage is likely to be significant enough to prevent a return to normal functioning.
| |
| | |
| The effects of long term comas are not limited to the comatose person. Long term coma can have significant impact on their families.<ref>{{cite web | url = http://www.mayoclinic.com/health/coma/DS00724/DSECTION=10 | title = Coma: Coping skills | author = Mayo Clinic staff | date = May 17, 2006 | accessdate = 2007-04-13 | publisher = Mayo Clinic}}</ref> Families of coma victims often have idealized images of the outcome based on Hollywood movie depictions of coma.<ref>Wijdicks EFM, Wijdicks CA (2006). "The portrayal of coma in contemporary motion pictures". ''Neurology'' '''66''' (9): 1300–1303. PMID 16682658.</ref> Adjusting to the realities of ventilators, feeding tubes, bedsores and muscle wasting may be difficult.<ref>Konig P ''et al'' (1992). "Psychological counseling of the family of patients with craniocerebral injuries (psychological family counseling of severely ill patients)". ''Zentralbl Neurochir'' '''53''' (2): 78–84. PMID 1636327.</ref> Treatment decision often involve complex ethical choices and can strain family dynamics.<ref>Montgomery V ''et al'' (2002). "The effect of severe traumatic brain injury on the family". ''J Trauma'' '''52''' (6): 1121–4. PMID 12045640.</ref>
| |
| | |
| ==See also==
| |
|
| |
|
| * [[Altitude sickness]] | | * [[Altitude sickness]] |
| * [[Deep water blackout]] | | * [[Deep water blackout]] |
| * [[Physical trauma]] | | * [[Physical trauma]] |
| * [[Hypoxia (medical)]] | | * [[Hypoxia]] |
| * [[Choking game]] | | * [[Choking game]] |
| * Space exposure
| |
|
| |
|
| ==References==
| | |
| {{Reflist|2}}
| |
|
| |
|
| {{CNS diseases of the nervous system}} | | {{CNS diseases of the nervous system}} |