Candida vulvovaginitis pathophysiology: Difference between revisions
Dima Nimri (talk | contribs) |
m (Bot: Removing from Primary care) |
||
| (17 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{ | {{Candida vulvovaginitis}} | ||
{{CMG}}; {{AE}}{{DN}} | {{CMG}}; {{AE}}{{DN}}, {{AKI}} | ||
==Overview== | ==Overview== | ||
Several virulence factors of [[Candida]] are implicated in [[vulvovaginitis]], but the process of transition from asymptomatic vaginal colonization to symptomatic [[vulvovaginitis]] is poorly understood. There may be genetic factors associated with [[Candida]] [[vulvovaginitis]], as infection runs in families in many cases and is more common in African-American women. | |||
==Pathophysiology== | ==Pathophysiology== | ||
===Vaginal Defensive mechanisms aganist Candida=== | |||
====Innate Mechanisms==== | |||
{| class="wikitable" | |||
!Defense | |||
!Mechanism of protection | |||
!Evidence of protection | |||
|- | |||
|Vaginal [[epithelial cells]] | |||
| | |||
*[[In vitro]] inhibition of [[Candida]] growth<ref name="pmid16239581">{{cite journal| author=Barousse MM, Espinosa T, Dunlap K, Fidel PL| title=Vaginal epithelial cell anti-Candida albicans activity is associated with protection against symptomatic vaginal candidiasis. | journal=Infect Immun | year= 2005 | volume= 73 | issue= 11 | pages= 7765-7 | pmid=16239581 | doi=10.1128/IAI.73.11.7765-7767.2005 | pmc=1273905 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16239581 }}</ref> | |||
| | |||
*Protective role [[in vivo]] unknown | |||
*Patients with recurrent [[candida]] infections have decreased anti-Candida activity | |||
|- | |||
|Mannose-binding lectin | |||
| | |||
*[[Epithelial cell]] associated [[protein]] which binds to [[Candida]] surface mannan.<ref name="pmid18715406" /> | |||
*Inhibits [[Candida]] growth by activating [[complement]]<ref name="pmid15243942">{{cite journal| author=Ip WK, Lau YL| title=Role of mannose-binding lectin in the innate defense against Candida albicans: enhancement of complement activation, but lack of opsonic function, in [[phagocytosis]] by human dendritic cells. | journal=J Infect Dis | year= 2004 | volume= 190 | issue= 3 | pages= 632-40 | pmid=15243942 | doi=10.1086/422397 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15243942 }}</ref> | |||
*Activity is genetically determined | |||
| | |||
*Decreased expression can increase the susceptibility for [[vaginal colonization]] of [[candida]] and leading to [[vaginitis]] | |||
|- | |||
|Activated [[lactoferrin]]<ref name="pmid15603095">{{cite journal| author=Naidu AS, Chen J, Martinez C, Tulpinski J, Pal BK, Fowler RS| title=Activated lactoferrin's ability to inhibit Candida growth and block yeast adhesion to the vaginal epithelial monolayer. | journal=J Reprod Med | year= 2004 | volume= 49 | issue= 11 | pages= 859-66 | pmid=15603095 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15603095 }}</ref> | |||
| | |||
*Fungistatic and fungicidal activity | |||
| | |||
*Role in protection aganist infection is not clear | |||
|- | |||
|Vaginal [[bacterial flora]] | |||
| | |||
*[[Lactobacillus]] species compete for nutrients. | |||
*[[Bacteriocins]] and [[hydrogen peroxide]] inhibit yeast growth/[[germination]] | |||
| | |||
*Role in protection aganist vaginitis still unclear | |||
|- | |||
|Phagocytic systems/polymononuclear [[leukocytes]], [[mononuclear cells]], [[complement]] | |||
| | |||
*Mainly found in [[lamina propria]] in experimental vaginitis, help in reducing the [[yeast]] load and its invasion by [[phagocytosis]] and intracellular killing<ref name="pmid340470">{{cite journal| author=Diamond RD, Krzesicki R, Jao W| title=Damage to pseudohyphal forms of Candida albicans by neutrophils in the absence of serum in vitro. | journal=J Clin Invest | year= 1978 | volume= 61 | issue= 2 | pages= 349-59 | pmid=340470 | doi=10.1172/JCI108945 | pmc=372545 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=340470 }}</ref> | |||
*[[Nitric oxide]] has anti-Candida activity | |||
| | |||
*Role in protection still unclear | |||
|} | |||
====Adaptive Mechanisms==== | |||
{| class="wikitable" | |||
!Defense | |||
!Mechanism | |||
!Role in Protection | |||
|- | |||
|[[Immunoglobulin]] mediated [[immunity]] | |||
|Systemic [[IgM]], [[IgG]], and local [[IgA]] antibodies are produced in response to the infection<ref name="pmid4556009">{{cite journal| author=Waldman RH, Cruz JM, Rowe DS| title=Immunoglobulin levels and antibody to Candida albicans in human cervicovaginal secretions. | journal=Clin Exp Immunol | year= 1972 | volume= 10 | issue= 3 | pages= 427-34 | pmid=4556009 | doi= | pmc=1713147 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=4556009 }}</ref> | |||
| | |||
*Protective role not proven. | |||
*Elevated [[titres]] of vaginal anti-Candida [[IgG]], [[IgA]] are detected in women with recurrent vaginitis | |||
*Persistent symptoms could be attributed to anti-Candida [[IgE]]<ref name="pmid8809464">{{cite journal| author=Fidel PL, Sobel JD| title=Immunopathogenesis of recurrent vulvovaginal candidiasis. | journal=Clin Microbiol Rev | year= 1996 | volume= 9 | issue= 3 | pages= 335-48 | pmid=8809464 | doi= | pmc=172897 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8809464 }}</ref> | |||
|- | |||
|[[Cell Mediated Immunity]] | |||
| | |||
[[Interleukin 4]] (Th2) inhibits anti-Candida activity of [[nitric oxide]] and protective pro-inflammatory Th1 [[cytokines]].<ref name="pmid15735412">{{cite journal| author=Fidel PL| title=Immunity in vaginal candidiasis. | journal=Curr Opin Infect Dis | year= 2005 | volume= 18 | issue= 2 | pages= 107-11 | pmid=15735412 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15735412 }}</ref> | |||
| | |||
*Role in protection from [[vulvovaginitis]] is still not clear | |||
*It is still a hypothesis<ref name="pmid15102806">{{cite journal| author=Fidel PL, Barousse M, Espinosa T, Ficarra M, Sturtevant J, Martin DH et al.| title=An intravaginal live Candida challenge in humans leads to new hypotheses for the immunopathogenesis of vulvovaginal candidiasis. | journal=Infect Immun | year= 2004 | volume= 72 | issue= 5 | pages= 2939-46 | pmid=15102806 | doi= | pmc=387876 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15102806 }}</ref> | |||
*Patients with recurrent infection have undetectable Th2 [[cytokines]]. | |||
|} | |||
===Candida Virulence Factors=== | |||
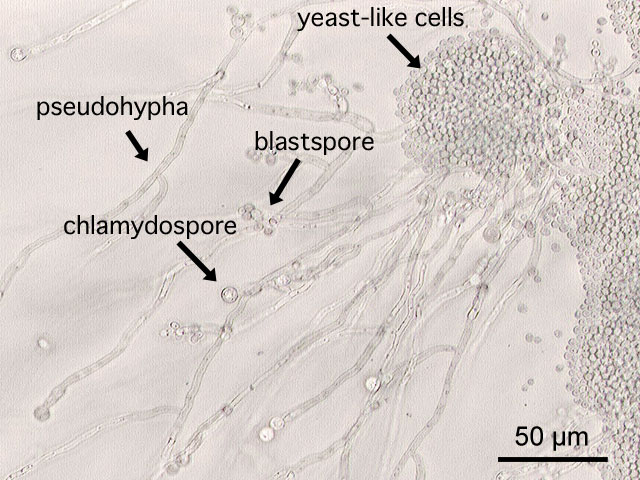
*[[C. albicans]] exists as [[blastospores]], [[germ tubes]], [[pseudomycelia]], [[true mycelia]] and [[chlamydospores]] on special [[culture]] media. [[C. glabrata]] exists exclusively in [[blastospores]]. | |||
*All strains of [[Candida]] species possess a [[yeast]] surface [[mannoprotein]] which helps in adhering to [[epithelial cells]] of the [[vagina]].<ref name="pmid17560449">{{cite journal |vauthors=Sobel JD |title=Vulvovaginal candidosis |journal=Lancet |volume=369 |issue=9577 |pages=1961–71 |year=2007 |pmid=17560449 |doi=10.1016/S0140-6736(07)60917-9 |url=}}</ref><ref name="pmid3895958">{{cite journal |vauthors=Sobel JD |title=Epidemiology and pathogenesis of recurrent vulvovaginal candidiasis |journal=Am. J. Obstet. Gynecol. |volume=152 |issue=7 Pt 2 |pages=924–35 |year=1985 |pmid=3895958 |doi= |url=}}</ref> | |||
*[[Germination]] of the spores helps in colonizing the vagina.<ref name="pmid6327527">{{cite journal| author=Sobel JD, Muller G, Buckley HR| title=Critical role of germ tube formation in the pathogenesis of candidal vaginitis. | journal=Infect Immun | year= 1984 | volume= 44 | issue= 3 | pages= 576-80 | pmid=6327527 | doi= | pmc=263631 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=6327527 }} </ref> | |||
*Proteolytic enzymes, toxins and [[phospholipase]] destroy the [[proteins]] that normally impair [[fungal]] invasion, enhancing the ability of [[Candida]] to colonize the [[vagina]].<ref name="pmid17560449">{{cite journal |vauthors=Sobel JD |title=Vulvovaginal candidosis |journal=Lancet |volume=369 |issue=9577 |pages=1961–71 |year=2007 |pmid=17560449 |doi=10.1016/S0140-6736(07)60917-9 |url=}}</ref><ref name="pmid3895958">{{cite journal |vauthors=Sobel JD |title=Epidemiology and pathogenesis of recurrent vulvovaginal candidiasis |journal=Am. J. Obstet. Gynecol. |volume=152 |issue=7 Pt 2 |pages=924–35 |year=1985 |pmid=3895958 |doi= |url=}}</ref><ref name="pmid2688924">{{cite journal |vauthors=Sobel JD |title=Pathogenesis of Candida vulvovaginitis |journal=Curr Top Med Mycol |volume=3 |issue= |pages=86–108 |year=1989 |pmid=2688924 |doi= |url=}}</ref><ref name="pmid12761103">{{cite journal| author=Schaller M, Bein M, Korting HC, Baur S, Hamm G, Monod M et al.| title=The secreted aspartyl proteinases Sap1 and Sap2 cause tissue damage in an in vitro model of vaginal candidiasis based on reconstituted human vaginal epithelium. | journal=Infect Immun | year= 2003 | volume= 71 | issue= 6 | pages= 3227-34 | pmid=12761103 | doi= | pmc=155757 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12761103 }}</ref> | |||
*[[Phenotypic switching]] of [[Candida]] is described in patients with recurrent vaginitis.<ref name="pmid3284370">{{cite journal| author=Soll DR| title=High-frequency switching in Candida albicans and its relations to vaginal candidiasis. | journal=Am J Obstet Gynecol | year= 1988 | volume= 158 | issue= 4 | pages= 997-1001 | pmid=3284370 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3284370 }}</ref> | |||
*[[C. albicans]] can form [[biofilm]]s on the [[intrauterine devices]] or sponges, causing disease recurrence.<ref name="pmid25935553">{{cite journal| author=Muzny CA, Schwebke JR| title=Biofilms: An Underappreciated Mechanism of Treatment Failure and Recurrence in Vaginal Infections. | journal=Clin Infect Dis | year= 2015 | volume= 61 | issue= 4 | pages= 601-6 | pmid=25935553 | doi=10.1093/cid/civ353 | pmc=4607736 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25935553 }}</ref> | |||
===Pathogenesis=== | ===Pathogenesis=== | ||
* | *[[Candida (genus)|Candida]] vulvovaginitis is a microbial disease and not all patients with detectable pathogen are symptomatic. Multiple [[risk factors]] and the imbalance in the protective vaginal defenses predispose patients to develop active disease. | ||
* | *[[Candida]] vaginal infections are more common in the reproductive age group because of the high concentration of [[estrogen]] as it increases the amount of [[glycogen]] in the [[vagina]] providing a carbon source for [[Candida]] organisms to [[colonize]]. It also increases the adherence of [[Candida]] to the [[vaginal epithelial cells]].<ref name="pmid11592551">{{cite journal| author=Dennerstein GJ, Ellis DH| title=Oestrogen, glycogen and vaginal candidiasis. | journal=Aust N Z J Obstet Gynaecol | year= 2001 | volume= 41 | issue= 3 | pages= 326-8 | pmid=11592551 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11592551 }}</ref> | ||
*The most common source of the infection is from the [[perianal]] area. Other less common source is [[sexual transmission]] and persistence of organisms in the [[vagina]] after treatment which is responsible for recurrence.<ref name="pmid333134">{{cite journal| author=Miles MR, Olsen L, Rogers A| title=Recurrent vaginal candidiasis. Importance of an intestinal reservoir. | journal=JAMA | year= 1977 | volume= 238 | issue= 17 | pages= 1836-7 | pmid=333134 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=333134 }}</ref> | |||
*The initial step of infection is [[colonization]] and symptoms appear with the invasion of the [[blastospores]] or [[pseudohyphae]] of the [[vaginal wall]].<ref name="pmid9880475">{{cite journal| author=Fidel PL, Vazquez JA, Sobel JD| title=Candida glabrata: review of epidemiology, pathogenesis, and clinical disease with comparison to C. albicans. | journal=Clin Microbiol Rev | year= 1999 | volume= 12 | issue= 1 | pages= 80-96 | pmid=9880475 | doi= | pmc=88907 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9880475 }}</ref> | |||
*The understanding of the transition from asymptomatic vaginal colonization with [[Candida]] to symptomatic [[vulvovaginitis]] is not clear.<ref name="pmid3895958">{{cite journal |vauthors=Sobel JD |title=Epidemiology and pathogenesis of recurrent vulvovaginal candidiasis |journal=Am. J. Obstet. Gynecol. |volume=152 |issue=7 Pt 2 |pages=924–35 |year=1985 |pmid=3895958 |doi= |url=}}</ref><ref name="pmid2688924">{{cite journal |vauthors=Sobel JD |title=Pathogenesis of Candida vulvovaginitis |journal=Curr Top Med Mycol |volume=3 |issue= |pages=86–108 |year=1989 |pmid=2688924 |doi= |url=}}</ref> | *The understanding of the transition from asymptomatic vaginal colonization with [[Candida]] to symptomatic [[vulvovaginitis]] is not clear.<ref name="pmid3895958">{{cite journal |vauthors=Sobel JD |title=Epidemiology and pathogenesis of recurrent vulvovaginal candidiasis |journal=Am. J. Obstet. Gynecol. |volume=152 |issue=7 Pt 2 |pages=924–35 |year=1985 |pmid=3895958 |doi= |url=}}</ref><ref name="pmid2688924">{{cite journal |vauthors=Sobel JD |title=Pathogenesis of Candida vulvovaginitis |journal=Curr Top Med Mycol |volume=3 |issue= |pages=86–108 |year=1989 |pmid=2688924 |doi= |url=}}</ref> | ||
===Genetics=== | ===Genetics=== | ||
*Few genetic factors are thought to be involved in patients with recurrent [[Candida]] [[vulvovaginitis]].<ref name="pmid12964847">{{cite journal| author=Calderon L, Williams R, Martinez M, Clemons KV, Stevens DA| title=Genetic susceptibility to vaginal candidiasis. | journal=Med Mycol | year= 2003 | volume= 41 | issue= 2 | pages= 143-7 | pmid=12964847 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12964847 }}</ref> | |||
*Supporting evidence is that [[Candida]] [[vaginitis]] is common in African-American women, runs in families and its association in patients with [[ABO]]-Lewis non-secretor phenotype (a rare [[blood group]]). | |||
*In addition, women with recurrent [[Candida]] [[vulvovaginitis]] were found to have decreased concentrations of [[mannose binding lectin]] (MBL), hence, the variant (MBL) gene is thought to be a contributing factor in the development of [[Candida]] [[vulvovaginitis]].<ref name="pmid17560449">{{cite journal |vauthors=Sobel JD |title=Vulvovaginal candidosis |journal=Lancet |volume=369 |issue=9577 |pages=1961–71 |year=2007 |pmid=17560449 |doi=10.1016/S0140-6736(07)60917-9 |url=}}</ref><ref name="pmid16256117">{{cite journal |vauthors=Liu F, Liao Q, Liu Z |title=Mannose-binding lectin and vulvovaginal candidiasis |journal=Int J Gynaecol Obstet |volume=92 |issue=1 |pages=43–7 |year=2006 |pmid=16256117 |doi=10.1016/j.ijgo.2005.08.024 |url=}}</ref><ref name="pmid18715406">{{cite journal |vauthors=Donders GG, Babula O, Bellen G, Linhares IM, Witkin SS |title=Mannose-binding lectin gene polymorphism and resistance to therapy in women with recurrent vulvovaginal candidiasis |journal=BJOG |volume=115 |issue=10 |pages=1225–31 |year=2008 |pmid=18715406 |doi=10.1111/j.1471-0528.2008.01830.x |url=}}</ref> | |||
===Gross Pathology=== | ===Gross Pathology=== | ||
On speculum examination typical curdy white discharge is present. | |||
<gallery> | |||
[http://www.peir.net Images courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology] | [http://www.peir.net Images courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology] | ||
Image:speculum_vagina.jpg|left|thumb|350px|This photograph is a speculum examination of the vagina with Candida infection and the typical thick, curdy vaginal discharge. - By Mikael Häggström - Own work, CC0, https://commons.wikimedia.org/w/index.php?curid=35323300 | |||
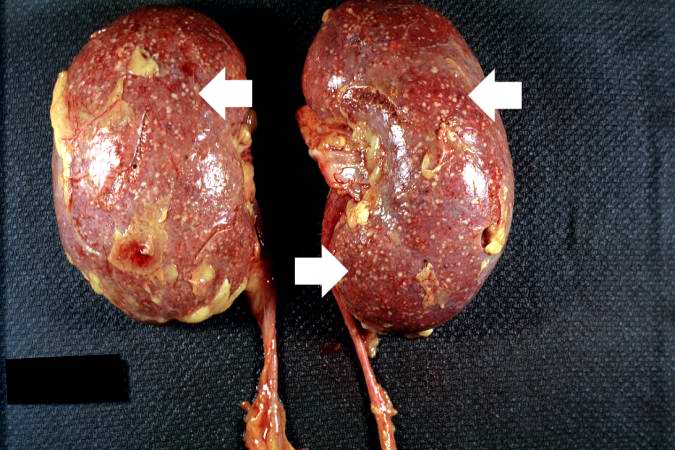
Image:Renal candidiasis 001.jpg|left|thumb|350px|This autopsy photograph of the kidneys demonstrates the multifocal punctate lesions visible on the serosal surface (arrows). Don't confuse these small yellow punctate lesions with the fat that is adherent to the renal capsule. - © Copyright UAB and the UAB Research Foundation, 1999-2013. All rights reserved | |||
<br clear="left"/> | <br clear="left"/> | ||
Image:Renal candidiasis 002.jpeg|left|thumb|350px|This photograph of the cut surface of these kidneys shows that these multifocal punctate lesions are primarily in the cortex (arrows). - © Copyright UAB and the UAB Research Foundation, 1999-2013. All rights reserved | |||
<br clear="left"/> | <br clear="left"/> | ||
</gallery> | |||
===Microscopic Pathology=== | ===Microscopic Pathology=== | ||
Microscopic examination of the wet mount with 10% KOH or saline demonstrates hyphae, pseudohyphae and blastospores. | |||
<gallery> | |||
Image:Calbicans.jpg|left|thumb|350px|This is a a microscopic image of Candida albicans, grown on cornmeal agar medium. - By Y tambe - Y tambe's file, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=233284 | |||
<br clear="left"/> | |||
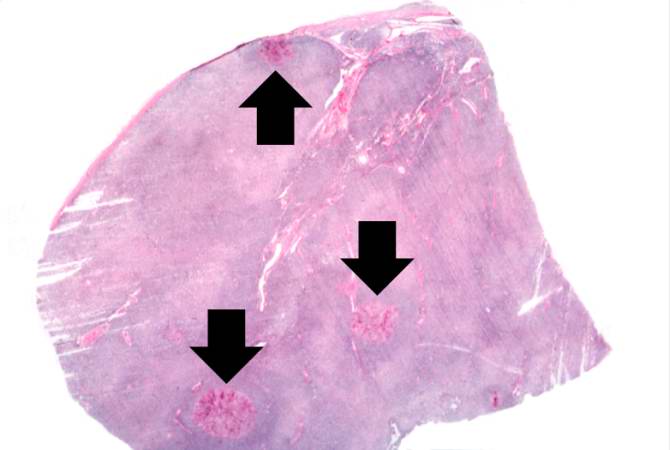
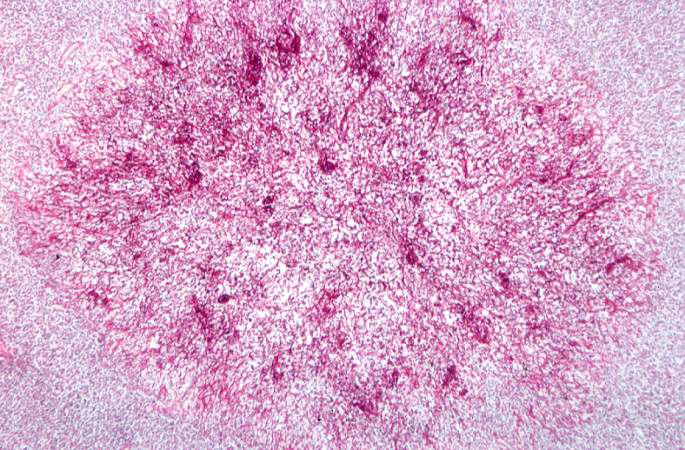
Image:Renal candidiasis 003.jpeg|left|thumb|350px|This is a low-power photomicrograph of lymph node with three prominent areas of Candida colonies (arrows). Even at this low magnification, the purple-staining yeast and pseudohyphae can be easily seen. This section was stained with Periodic Acid-Schiff Hematoxylin (PASH), which stains the cell wall of fungi to make them more easily visible. - © Copyright UAB and the UAB Research Foundation, 1999-2013. All rights reserved | |||
<br clear="left"/> | <br clear="left"/> | ||
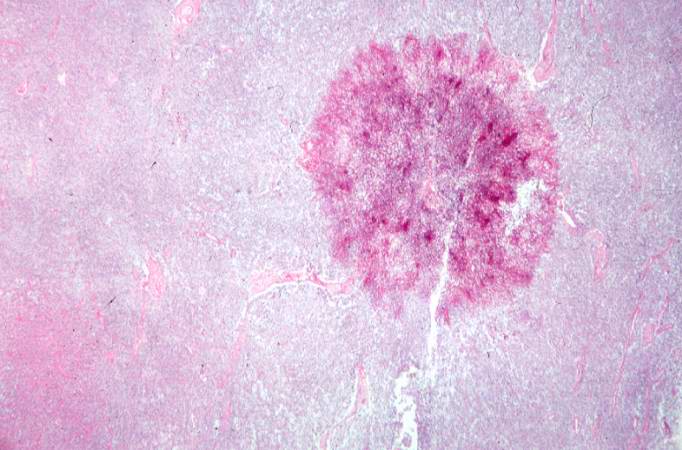
Image:Renal candidiasis 004.jpeg|left|thumb|350px|This is a low-power photomicrograph of one of the Candida colonies from this lymph node. The chains of yeast which are termed "pseudohyphae" are apparent at this magnification. - © Copyright UAB and the UAB Research Foundation, 1999-2013. All rights reserved | |||
<br clear="left"/> | <br clear="left"/> | ||
Image:Renal candidiasis 005.jpeg|left|thumb|350px|This higher-power photomicrograph shows the yeasts and pseudohyphae in this focus of Candida organisms. - © Copyright UAB and the UAB Research Foundation, 1999-2013. All rights reserved | |||
<br clear="left"/> | <br clear="left"/> | ||
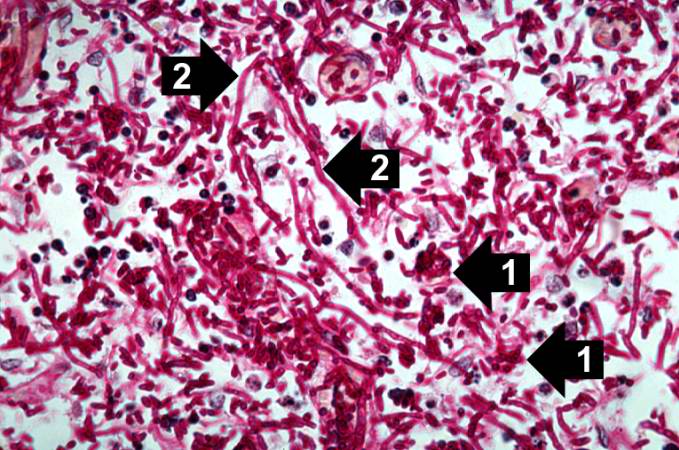
Image:Renal candidiasis 006.jpeg|left|thumb|350px|This high-power photomicrograph shows the yeasts (1) and pseudohyphae (2). - © Copyright UAB and the UAB Research Foundation, 1999-2013. All rights reserved | |||
<br clear="left"/> | <br clear="left"/> | ||
</gallery> | |||
< | |||
===Associated Conditions=== | ===Associated Conditions=== | ||
*[[Candida]] [[vulvovaginitis]] may be associated with other pathogens that cause [[vulvovaginitis]]. These include ''Trichomonas vaginalis'' and ''Gardnerella vaginalis''. The association may be a mixed infection, where 2 or more pathogens are symptomatic, or a co-infection, in which there are 2 or more pathogens but some are not symptomatic.<ref name="pmid23354954">{{cite journal |vauthors=Sobel JD, Subramanian C, Foxman B, Fairfax M, Gygax SE |title=Mixed vaginitis-more than coinfection and with therapeutic implications |journal=Curr Infect Dis Rep |volume=15 |issue=2 |pages=104–8 |year=2013 |pmid=23354954 |doi=10.1007/s11908-013-0325-5 |url=}}</ref><ref name="pmid15026404">{{cite journal |vauthors=Anderson MR, Klink K, Cohrssen A |title=Evaluation of vaginal complaints |journal=JAMA |volume=291 |issue=11 |pages=1368–79 |year=2004 |pmid=15026404 |doi=10.1001/jama.291.11.1368 |url=}}</ref> | *[[Candida]] [[vulvovaginitis]] may be associated with other pathogens that cause [[vulvovaginitis]]. These include ''Trichomonas vaginalis'' and ''Gardnerella vaginalis''. The association may be a mixed infection, where 2 or more pathogens are symptomatic, or a co-infection, in which there are 2 or more pathogens but some are not symptomatic.<ref name="pmid23354954">{{cite journal |vauthors=Sobel JD, Subramanian C, Foxman B, Fairfax M, Gygax SE |title=Mixed vaginitis-more than coinfection and with therapeutic implications |journal=Curr Infect Dis Rep |volume=15 |issue=2 |pages=104–8 |year=2013 |pmid=23354954 |doi=10.1007/s11908-013-0325-5 |url=}}</ref><ref name="pmid15026404">{{cite journal |vauthors=Anderson MR, Klink K, Cohrssen A |title=Evaluation of vaginal complaints |journal=JAMA |volume=291 |issue=11 |pages=1368–79 |year=2004 |pmid=15026404 |doi=10.1001/jama.291.11.1368 |url=}}</ref> | ||
| Line 47: | Line 132: | ||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WS}} | {{WS}} | ||
[[Category:Disease]] | |||
[[Category:Up-To-Date]] | |||
[[Category:Gynecology]] | |||
[[Category:Obstetrics]] | |||
Latest revision as of 20:47, 29 July 2020
|
Candida vulvovaginitis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Candida vulvovaginitis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Candida vulvovaginitis pathophysiology |
|
Risk calculators and risk factors for Candida vulvovaginitis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Dima Nimri, M.D. [2], Aravind Kuchkuntla, M.B.B.S[3]
Overview
Several virulence factors of Candida are implicated in vulvovaginitis, but the process of transition from asymptomatic vaginal colonization to symptomatic vulvovaginitis is poorly understood. There may be genetic factors associated with Candida vulvovaginitis, as infection runs in families in many cases and is more common in African-American women.
Pathophysiology
Vaginal Defensive mechanisms aganist Candida
Innate Mechanisms
| Defense | Mechanism of protection | Evidence of protection |
|---|---|---|
| Vaginal epithelial cells | ||
| Mannose-binding lectin |
|
|
| Activated lactoferrin[4] |
|
|
| Vaginal bacterial flora |
|
|
| Phagocytic systems/polymononuclear leukocytes, mononuclear cells, complement |
|
|
Adaptive Mechanisms
| Defense | Mechanism | Role in Protection |
|---|---|---|
| Immunoglobulin mediated immunity | Systemic IgM, IgG, and local IgA antibodies are produced in response to the infection[6] | |
| Cell Mediated Immunity |
Interleukin 4 (Th2) inhibits anti-Candida activity of nitric oxide and protective pro-inflammatory Th1 cytokines.[8] |
|
Candida Virulence Factors
- C. albicans exists as blastospores, germ tubes, pseudomycelia, true mycelia and chlamydospores on special culture media. C. glabrata exists exclusively in blastospores.
- All strains of Candida species possess a yeast surface mannoprotein which helps in adhering to epithelial cells of the vagina.[10][11]
- Germination of the spores helps in colonizing the vagina.[12]
- Proteolytic enzymes, toxins and phospholipase destroy the proteins that normally impair fungal invasion, enhancing the ability of Candida to colonize the vagina.[10][11][13][14]
- Phenotypic switching of Candida is described in patients with recurrent vaginitis.[15]
- C. albicans can form biofilms on the intrauterine devices or sponges, causing disease recurrence.[16]
Pathogenesis
- Candida vulvovaginitis is a microbial disease and not all patients with detectable pathogen are symptomatic. Multiple risk factors and the imbalance in the protective vaginal defenses predispose patients to develop active disease.
- Candida vaginal infections are more common in the reproductive age group because of the high concentration of estrogen as it increases the amount of glycogen in the vagina providing a carbon source for Candida organisms to colonize. It also increases the adherence of Candida to the vaginal epithelial cells.[17]
- The most common source of the infection is from the perianal area. Other less common source is sexual transmission and persistence of organisms in the vagina after treatment which is responsible for recurrence.[18]
- The initial step of infection is colonization and symptoms appear with the invasion of the blastospores or pseudohyphae of the vaginal wall.[19]
- The understanding of the transition from asymptomatic vaginal colonization with Candida to symptomatic vulvovaginitis is not clear.[11][13]
Genetics
- Few genetic factors are thought to be involved in patients with recurrent Candida vulvovaginitis.[20]
- Supporting evidence is that Candida vaginitis is common in African-American women, runs in families and its association in patients with ABO-Lewis non-secretor phenotype (a rare blood group).
- In addition, women with recurrent Candida vulvovaginitis were found to have decreased concentrations of mannose binding lectin (MBL), hence, the variant (MBL) gene is thought to be a contributing factor in the development of Candida vulvovaginitis.[10][21][2]
Gross Pathology
On speculum examination typical curdy white discharge is present.
-
This photograph is a speculum examination of the vagina with Candida infection and the typical thick, curdy vaginal discharge. - By Mikael Häggström - Own work, CC0, https://commons.wikimedia.org/w/index.php?curid=35323300
-
This autopsy photograph of the kidneys demonstrates the multifocal punctate lesions visible on the serosal surface (arrows). Don't confuse these small yellow punctate lesions with the fat that is adherent to the renal capsule. - © Copyright UAB and the UAB Research Foundation, 1999-2013. All rights reserved
-
This photograph of the cut surface of these kidneys shows that these multifocal punctate lesions are primarily in the cortex (arrows). - © Copyright UAB and the UAB Research Foundation, 1999-2013. All rights reserved
Microscopic Pathology
Microscopic examination of the wet mount with 10% KOH or saline demonstrates hyphae, pseudohyphae and blastospores.
-
This is a a microscopic image of Candida albicans, grown on cornmeal agar medium. - By Y tambe - Y tambe's file, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=233284
-
This is a low-power photomicrograph of lymph node with three prominent areas of Candida colonies (arrows). Even at this low magnification, the purple-staining yeast and pseudohyphae can be easily seen. This section was stained with Periodic Acid-Schiff Hematoxylin (PASH), which stains the cell wall of fungi to make them more easily visible. - © Copyright UAB and the UAB Research Foundation, 1999-2013. All rights reserved
-
This is a low-power photomicrograph of one of the Candida colonies from this lymph node. The chains of yeast which are termed "pseudohyphae" are apparent at this magnification. - © Copyright UAB and the UAB Research Foundation, 1999-2013. All rights reserved
-
This higher-power photomicrograph shows the yeasts and pseudohyphae in this focus of Candida organisms. - © Copyright UAB and the UAB Research Foundation, 1999-2013. All rights reserved
-
This high-power photomicrograph shows the yeasts (1) and pseudohyphae (2). - © Copyright UAB and the UAB Research Foundation, 1999-2013. All rights reserved
Associated Conditions
- Candida vulvovaginitis may be associated with other pathogens that cause vulvovaginitis. These include Trichomonas vaginalis and Gardnerella vaginalis. The association may be a mixed infection, where 2 or more pathogens are symptomatic, or a co-infection, in which there are 2 or more pathogens but some are not symptomatic.[22][23]
References
- ↑ Barousse MM, Espinosa T, Dunlap K, Fidel PL (2005). "Vaginal epithelial cell anti-Candida albicans activity is associated with protection against symptomatic vaginal candidiasis". Infect Immun. 73 (11): 7765–7. doi:10.1128/IAI.73.11.7765-7767.2005. PMC 1273905. PMID 16239581.
- ↑ 2.0 2.1 Donders GG, Babula O, Bellen G, Linhares IM, Witkin SS (2008). "Mannose-binding lectin gene polymorphism and resistance to therapy in women with recurrent vulvovaginal candidiasis". BJOG. 115 (10): 1225–31. doi:10.1111/j.1471-0528.2008.01830.x. PMID 18715406.
- ↑ Ip WK, Lau YL (2004). "Role of mannose-binding lectin in the innate defense against Candida albicans: enhancement of complement activation, but lack of opsonic function, in [[phagocytosis]] by human dendritic cells". J Infect Dis. 190 (3): 632–40. doi:10.1086/422397. PMID 15243942. URL–wikilink conflict (help)
- ↑ Naidu AS, Chen J, Martinez C, Tulpinski J, Pal BK, Fowler RS (2004). "Activated lactoferrin's ability to inhibit Candida growth and block yeast adhesion to the vaginal epithelial monolayer". J Reprod Med. 49 (11): 859–66. PMID 15603095.
- ↑ Diamond RD, Krzesicki R, Jao W (1978). "Damage to pseudohyphal forms of Candida albicans by neutrophils in the absence of serum in vitro". J Clin Invest. 61 (2): 349–59. doi:10.1172/JCI108945. PMC 372545. PMID 340470.
- ↑ Waldman RH, Cruz JM, Rowe DS (1972). "Immunoglobulin levels and antibody to Candida albicans in human cervicovaginal secretions". Clin Exp Immunol. 10 (3): 427–34. PMC 1713147. PMID 4556009.
- ↑ Fidel PL, Sobel JD (1996). "Immunopathogenesis of recurrent vulvovaginal candidiasis". Clin Microbiol Rev. 9 (3): 335–48. PMC 172897. PMID 8809464.
- ↑ Fidel PL (2005). "Immunity in vaginal candidiasis". Curr Opin Infect Dis. 18 (2): 107–11. PMID 15735412.
- ↑ Fidel PL, Barousse M, Espinosa T, Ficarra M, Sturtevant J, Martin DH; et al. (2004). "An intravaginal live Candida challenge in humans leads to new hypotheses for the immunopathogenesis of vulvovaginal candidiasis". Infect Immun. 72 (5): 2939–46. PMC 387876. PMID 15102806.
- ↑ 10.0 10.1 10.2 Sobel JD (2007). "Vulvovaginal candidosis". Lancet. 369 (9577): 1961–71. doi:10.1016/S0140-6736(07)60917-9. PMID 17560449.
- ↑ 11.0 11.1 11.2 Sobel JD (1985). "Epidemiology and pathogenesis of recurrent vulvovaginal candidiasis". Am. J. Obstet. Gynecol. 152 (7 Pt 2): 924–35. PMID 3895958.
- ↑ Sobel JD, Muller G, Buckley HR (1984). "Critical role of germ tube formation in the pathogenesis of candidal vaginitis". Infect Immun. 44 (3): 576–80. PMC 263631. PMID 6327527.
- ↑ 13.0 13.1 Sobel JD (1989). "Pathogenesis of Candida vulvovaginitis". Curr Top Med Mycol. 3: 86–108. PMID 2688924.
- ↑ Schaller M, Bein M, Korting HC, Baur S, Hamm G, Monod M; et al. (2003). "The secreted aspartyl proteinases Sap1 and Sap2 cause tissue damage in an in vitro model of vaginal candidiasis based on reconstituted human vaginal epithelium". Infect Immun. 71 (6): 3227–34. PMC 155757. PMID 12761103.
- ↑ Soll DR (1988). "High-frequency switching in Candida albicans and its relations to vaginal candidiasis". Am J Obstet Gynecol. 158 (4): 997–1001. PMID 3284370.
- ↑ Muzny CA, Schwebke JR (2015). "Biofilms: An Underappreciated Mechanism of Treatment Failure and Recurrence in Vaginal Infections". Clin Infect Dis. 61 (4): 601–6. doi:10.1093/cid/civ353. PMC 4607736. PMID 25935553.
- ↑ Dennerstein GJ, Ellis DH (2001). "Oestrogen, glycogen and vaginal candidiasis". Aust N Z J Obstet Gynaecol. 41 (3): 326–8. PMID 11592551.
- ↑ Miles MR, Olsen L, Rogers A (1977). "Recurrent vaginal candidiasis. Importance of an intestinal reservoir". JAMA. 238 (17): 1836–7. PMID 333134.
- ↑ Fidel PL, Vazquez JA, Sobel JD (1999). "Candida glabrata: review of epidemiology, pathogenesis, and clinical disease with comparison to C. albicans". Clin Microbiol Rev. 12 (1): 80–96. PMC 88907. PMID 9880475.
- ↑ Calderon L, Williams R, Martinez M, Clemons KV, Stevens DA (2003). "Genetic susceptibility to vaginal candidiasis". Med Mycol. 41 (2): 143–7. PMID 12964847.
- ↑ Liu F, Liao Q, Liu Z (2006). "Mannose-binding lectin and vulvovaginal candidiasis". Int J Gynaecol Obstet. 92 (1): 43–7. doi:10.1016/j.ijgo.2005.08.024. PMID 16256117.
- ↑ Sobel JD, Subramanian C, Foxman B, Fairfax M, Gygax SE (2013). "Mixed vaginitis-more than coinfection and with therapeutic implications". Curr Infect Dis Rep. 15 (2): 104–8. doi:10.1007/s11908-013-0325-5. PMID 23354954.
- ↑ Anderson MR, Klink K, Cohrssen A (2004). "Evaluation of vaginal complaints". JAMA. 291 (11): 1368–79. doi:10.1001/jama.291.11.1368. PMID 15026404.