Aneurysmal bone cyst
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Rohan A. Bhimani, M.B.B.S., D.N.B., M.Ch.[2]; Cafer Zorkun, M.D., Ph.D. [3]
Overview
Historical Perspective
- In 1942, Jaffe and Lichtenstein first described aneurysmal bone cyst.[1][2]
- In 1940, Ewing propoosed that aneurysmal bone cyst was caused by increased venous pressure.
- In 1956, Cruz and Coley also supported Ewing's hypothesis.
- In 1956, Barnes hypothesized that aneurysmal bone cyst was due to an abnormal response to injury.
- In 1956, Otterdoom after a thorough pathological study, concluded that aneurysmal bone cyst was an angioma of bone.
Classification
- Aneurysmal bone cyst(ABC) can be classified based on imaging findings and on mechanism of origin.
Mechanism of Origin
Based on mechanism of origin, aneurysmal bone cyst can be classified into:[3][4]
Primary Aneurysmal Bone Cyst(ABC)
- When ABC arises de novo, it is called primary ABC.
- About 70% of ABC's are primary in origin.
Secondary Aneurysmal Bone Cyst(ABC)
- When ABC coexist with other bone lesions, it is termed as secondary ABC's.
- About 30% of ABC's are secondary in origin.
- Commonly associated bone lesions include:
- Unicameral bone cyst
- Nonossifying fibromas
- Osteoblastoma
- Giant cell tumor
- Enchondroma
- Chondroblastoma
- Fibrous dysplasia
- Chondromyxoid fibroma
- Non ossifying fibroma
Enneking (MSTS) Staging System
- The Enneking surgical staging system (also known as the MSTS system) for benign musculoskeletal tumors based on radiographic characteristics of the tumor host margin.[5]
- It is widely accepted and routinely used classification.
| Stages | Description |
|---|---|
| 1 | Latent: Well demarcated borders |
| 2 | Active: Indistinct borders |
| 3 | Aggressive: Indistinct borders |
Pathophysiology
- The exact pathogenesis of aneurysmal bone cyst is not fully understood.[6][7]
- Various theories have been proposed concerning the pathogenesis of aneurysmal bone cyst:
- Local alteration in hemodynamics resulting in markedly increased venous pressure and development of a dilated vascular bed within the involved bone.[8][9]
- Primary ABCs demonstrate a t(16;17)(q22;p13) fusion of the TRE17/CDH11-USP6 oncogene leading to increased cellular cadherin-11 activity which arrests osteoblastic maturation in a more primitive state.[10][11][12]
- ABCs usually present in the long bones such as the humerus, femur, tibia; and fibula.
- About 25% of ABC's are seen in posterior element of spine.
- ABC's typically occur in the metaphysis of the long bones.
Causes
- The true causes of aneurysmal bone cyst(ABC) are not known.
- Commonly proposed theories are as follows:
- ABCs may be caused by a reaction secondary to another bony lesions such as giant cell tumor, chondroblastoma, fibrous dysplasia, osteosarocma; and chondrosarcoma.
- ABCs may arise de novo.
- ABCs may arise secondary to previous trauma.
Differentiating ((Page name)) from Other Diseases
[Disease name] must be differentiated from other diseases that cause [clinical feature 1], [clinical feature 2], and [clinical feature 3], such as [differential dx1], [differential dx2], and [differential dx3].
OR
[Disease name] must be differentiated from [[differential dx1], [differential dx2], and [differential dx3].
Epidemiology and Demographics
- ABC accounts for 1% to 2% of all primary bone tumors.[13]
- The incidence of aneurysmal bone cyst is approximately 0.14 per 100,000 individuals worldwide.[13]
- Adolescents and children are most affected by aneurysmal bone cyst.
- The age distribution of aneurysaml bone cyst is between 1.5-25 years.[14][15]
- The mean age of the patients with aneurysmal bone cyst is 16 years.[16]
- Women are more commonly affected than men, with a 1:0.84 ratio.[17]
- There is no racial predilection to aneurysmal bone cyst.
Risk Factors
There are no established risk factors for aneurysmal bone cyst.
Screening
There is insufficient evidence to recommend routine screening for aneurysmal bone cyst.
Natural History, Complications, and Prognosis
- Common complications of aneurysmal bone cyst include:[18][19]
- Pathological fracture
- Premature epiphyseal closure
- Limb-length discrepancy
- Angular deformity
- Malignant transformations to form malignant osteosarcoma.
- Prognosis is generally excellent for aneurysmal bone cyst.
- Factors that influence the outcome of the aneurysmal bone cyst include:
- Young age
- Open growth plates
- Metaphyseal location
Diagnosis
Diagnostic Study of Choice
 |
- Biopsy is the diagnostic study of choice for the diagnosis of aneurysmal bone cyst.
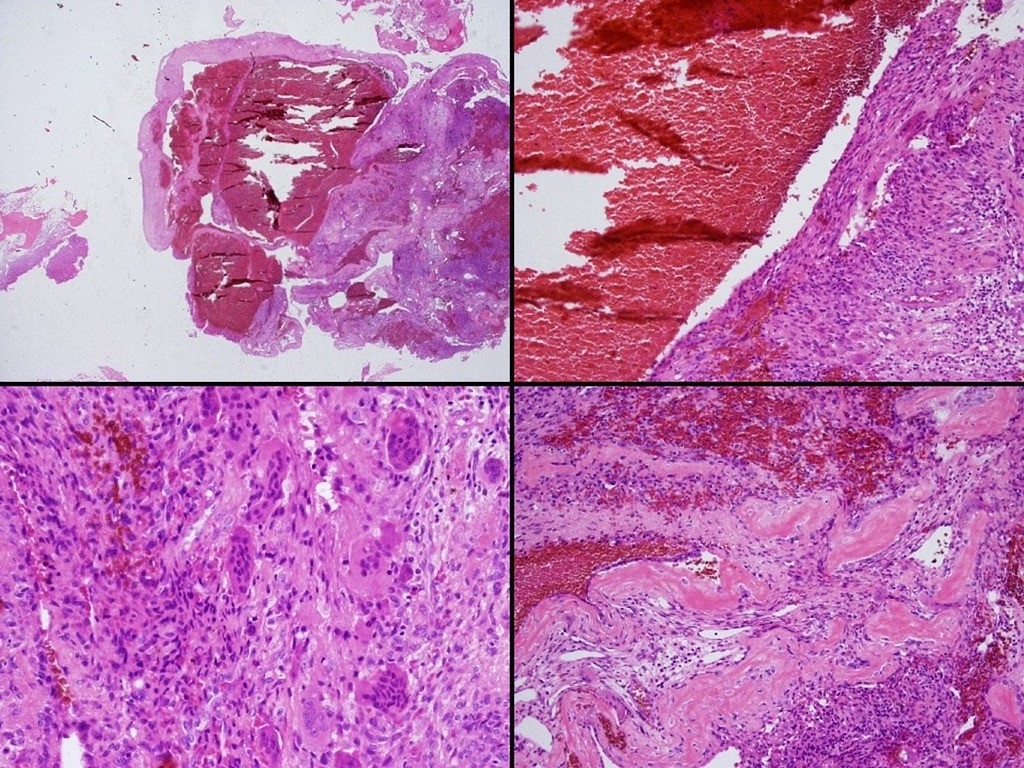
- Gross appearance of aneurysmal bone cyst include:
- Blood-soaked sponge.
- A thin subperiosteal shell of new bone surrounds the structure
- Cystic blood-filled cavities.
- The tissue within shows brownish intertwining septa.
- The stroma contains proliferative fibroblasts, spindle cells, areas of osteoid formation, and an uneven distribution of multinucleated giant cells that tend to surround the fluid-filled cavities in a pigs at the trough formation.
- HIstological appearance includes:
- Cavernous space.
- Blood-filled spaces without endothelial lining.
- Cavity lining with numerous benign giant cells and spindle cells with thin strands of woven bone present.
History and Symptoms
- The majority of patients with osteoblastoma have a positive history of:
- Pain,
- Swelling
- Pathological fracture
Neurologic conditions occur often due to compression of either the spinal cord or nerve roots, and lead to: Paralysis Spinal stiffness
Physical Examination
Patients with [disease name] usually appear [general appearance]. Physical examination of patients with [disease name] is usually remarkable for [finding 1], [finding 2], and [finding 3].
OR
Common physical examination findings of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
The presence of [finding(s)] on physical examination is diagnostic of [disease name].
OR
The presence of [finding(s)] on physical examination is highly suggestive of [disease name].
Laboratory Findings
An elevated/reduced concentration of serum/blood/urinary/CSF/other [lab test] is diagnostic of [disease name].
OR
Laboratory findings consistent with the diagnosis of [disease name] include [abnormal test 1], [abnormal test 2], and [abnormal test 3].
OR
[Test] is usually normal among patients with [disease name].
OR
Some patients with [disease name] may have elevated/reduced concentration of [test], which is usually suggestive of [progression/complication].
OR
There are no diagnostic laboratory findings associated with [disease name].
Electrocardiogram
There are no ECG findings associated with [disease name].
OR
An ECG may be helpful in the diagnosis of [disease name]. Findings on an ECG suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
X-ray
There are no x-ray findings associated with [disease name].
OR
An x-ray may be helpful in the diagnosis of [disease name]. Findings on an x-ray suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no x-ray findings associated with [disease name]. However, an x-ray may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
Echocardiography or Ultrasound
There are no echocardiography/ultrasound findings associated with [disease name].
OR
Echocardiography/ultrasound may be helpful in the diagnosis of [disease name]. Findings on an echocardiography/ultrasound suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no echocardiography/ultrasound findings associated with [disease name]. However, an echocardiography/ultrasound may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
CT scan
There are no CT scan findings associated with [disease name].
OR
[Location] CT scan may be helpful in the diagnosis of [disease name]. Findings on CT scan suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no CT scan findings associated with [disease name]. However, a CT scan may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
MRI
There are no MRI findings associated with [disease name].
OR
[Location] MRI may be helpful in the diagnosis of [disease name]. Findings on MRI suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no MRI findings associated with [disease name]. However, a MRI may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
Other Imaging Findings
There are no other imaging findings associated with [disease name].
OR
[Imaging modality] may be helpful in the diagnosis of [disease name]. Findings on an [imaging modality] suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
Other Diagnostic Studies
There are no other diagnostic studies associated with [disease name].
OR
[Diagnostic study] may be helpful in the diagnosis of [disease name]. Findings suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
Other diagnostic studies for [disease name] include [diagnostic study 1], which demonstrates [finding 1], [finding 2], and [finding 3], and [diagnostic study 2], which demonstrates [finding 1], [finding 2], and [finding 3].
Treatment
Medical Therapy
There is no treatment for [disease name]; the mainstay of therapy is supportive care.
OR
Supportive therapy for [disease name] includes [therapy 1], [therapy 2], and [therapy 3].
OR
The majority of cases of [disease name] are self-limited and require only supportive care.
OR
[Disease name] is a medical emergency and requires prompt treatment.
OR
The mainstay of treatment for [disease name] is [therapy].
OR The optimal therapy for [malignancy name] depends on the stage at diagnosis.
OR
[Therapy] is recommended among all patients who develop [disease name].
OR
Pharmacologic medical therapy is recommended among patients with [disease subclass 1], [disease subclass 2], and [disease subclass 3].
OR
Pharmacologic medical therapies for [disease name] include (either) [therapy 1], [therapy 2], and/or [therapy 3].
OR
Empiric therapy for [disease name] depends on [disease factor 1] and [disease factor 2].
OR
Patients with [disease subclass 1] are treated with [therapy 1], whereas patients with [disease subclass 2] are treated with [therapy 2].
Surgery
Surgical intervention is not recommended for the management of [disease name].
OR
Surgery is not the first-line treatment option for patients with [disease name]. Surgery is usually reserved for patients with either [indication 1], [indication 2], and [indication 3]
OR
The mainstay of treatment for [disease name] is medical therapy. Surgery is usually reserved for patients with either [indication 1], [indication 2], and/or [indication 3].
OR
The feasibility of surgery depends on the stage of [malignancy] at diagnosis.
OR
Surgery is the mainstay of treatment for [disease or malignancy].
Primary Prevention
There are no established measures for the primary prevention of [disease name].
OR
There are no available vaccines against [disease name].
OR
Effective measures for the primary prevention of [disease name] include [measure1], [measure2], and [measure3].
OR
[Vaccine name] vaccine is recommended for [patient population] to prevent [disease name]. Other primary prevention strategies include [strategy 1], [strategy 2], and [strategy 3].
Secondary Prevention
There are no established measures for the secondary prevention of [disease name].
OR
Effective measures for the secondary prevention of [disease name] include [strategy 1], [strategy 2], and [strategy 3].
References
- ↑ Mendenhall WM, Zlotecki RA, Gibbs CP, Reith JD, Scarborough MT, Mendenhall NP (2006). "Aneurysmal bone cyst". Am J Clin Oncol. 29 (3): 311–5. doi:10.1097/01.coc.0000204403.13451.52. PMID 16755186.
- ↑ GODFREY LW, GRESHAM GA (1959). "The natural history of aneurysmal bone cyst". Proc R Soc Med. 52: 900–5. PMC 1870818. PMID 13850355.
- ↑ Feigenberg SJ, Marcus RB, Zlotecki RA, Scarborough MT, Berrey BH, Enneking WF (2001). "Megavoltage radiotherapy for aneurysmal bone cysts". Int J Radiat Oncol Biol Phys. 49 (5): 1243–7. PMID 11286830.
- ↑ Lin PP, Brown C, Raymond AK, Deavers MT, Yasko AW (2008). "Aneurysmal bone cysts recur at juxtaphyseal locations in skeletally immature patients". Clin Orthop Relat Res. 466 (3): 722–8. doi:10.1007/s11999-007-0080-8. PMC 2505199. PMID 18202898.
- ↑ Jawad MU, Scully SP (2010). "In brief: classifications in brief: enneking classification: benign and malignant tumors of the musculoskeletal system". Clin Orthop Relat Res. 468 (7): 2000–2. doi:10.1007/s11999-010-1315-7. PMC 2882012. PMID 20333492.
- ↑ Peabody, Terrance (2014). Orthopaedic oncology : primary and metastatic tumors of the skeletal system. Cham: Springer. ISBN 9783319073224.
- ↑ Cottalorda J, Bourelle S (2007). "Modern concepts of primary aneurysmal bone cyst". Arch Orthop Trauma Surg. 127 (2): 105–14. doi:10.1007/s00402-006-0223-5. PMID 16937137.
- ↑ LICHTENSTEIN L (1953). "Aneurysmal bone cyst; further observations". Cancer. 6 (6): 1228–37. PMID 13106840.
- ↑ Szendroi M, Arató G, Ezzati A, Hüttl K, Szavcsur P (1998). "Aneurysmal bone cyst: its pathogenesis based on angiographic, immunohistochemical and electron microscopic studies". Pathol Oncol Res. 4 (4): 277–81. PMID 9887358.
- ↑ Panoutsakopoulos G, Pandis N, Kyriazoglou I, Gustafson P, Mertens F, Mandahl N (1999). "Recurrent t(16;17)(q22;p13) in aneurysmal bone cysts". Genes Chromosomes Cancer. 26 (3): 265–6. PMID 10502326.
- ↑ Oliveira AM, Perez-Atayde AR, Dal Cin P, Gebhardt MC, Chen CJ, Neff JR; et al. (2005). "Aneurysmal bone cyst variant translocations upregulate USP6 transcription by promoter swapping with the ZNF9, COL1A1, TRAP150, and OMD genes". Oncogene. 24 (21): 3419–26. doi:10.1038/sj.onc.1208506. PMID 15735689.
- ↑ Dal Cin P, Kozakewich HP, Goumnerova L, Mankin HJ, Rosenberg AE, Fletcher JA (2000). "Variant translocations involving 16q22 and 17p13 in solid variant and extraosseous forms of aneurysmal bone cyst". Genes Chromosomes Cancer. 28 (2): 233–4. PMID 10825009.
- ↑ 13.0 13.1 Leithner A, Windhager R, Lang S, Haas OA, Kainberger F, Kotz R (1999). "Aneurysmal bone cyst. A population based epidemiologic study and literature review". Clin Orthop Relat Res (363): 176–9. PMID 10379320.
- ↑ Mohan R, Sreekumaran GT (2016). "Secondary Aneurysmal Bone Cyst of the Scapula Treated by CT Guided Percutaneous Polidocanol Injection - A Case Report". J Clin Diagn Res. 10 (12): RD04–RD06. doi:10.7860/JCDR/2016/23561.9096. PMC 5296532. PMID 28208959.
- ↑ Biesecker JL, Marcove RC, Huvos AG, Miké V (1970). "Aneurysmal bone cysts. A clinicopathologic study of 66 cases". Cancer. 26 (3): 615–25. PMID 5458269.
- ↑ Ruiter DJ, van Rijssel TG, van der Velde EA (1977). "Aneurysmal bone cysts: a clinicopathological study of 105 cases". Cancer. 39 (5): 2231–9. PMID 265751.
- ↑ Vergel De Dios AM, Bond JR, Shives TC, McLeod RA, Unni KK (1992). "Aneurysmal bone cyst. A clinicopathologic study of 238 cases". Cancer. 69 (12): 2921–31. PMID 1591685.
- ↑ Gibbs CP, Hefele MC, Peabody TD, Montag AG, Aithal V, Simon MA (1999). "Aneurysmal bone cyst of the extremities. Factors related to local recurrence after curettage with a high-speed burr". J Bone Joint Surg Am. 81 (12): 1671–8. PMID 10608377.
- ↑ Papagelopoulos PJ, Currier BL, Shaughnessy WJ, Sim FH, Ebsersold MJ, Bond JR; et al. (1998). "Aneurysmal bone cyst of the spine. Management and outcome". Spine (Phila Pa 1976). 23 (5): 621–8. PMID 9530795.