Aneurysmal bone cyst: Difference between revisions
Farima Kahe (talk | contribs) |
|||
| (21 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{SI}} | |||
{{CMG}}; {{AE}} {{Rohan | {{CMG}}; {{AE}} {{Rohan}} | ||
==Overview== | ==Overview== | ||
[[Aneurysmal disease|Aneurysmal]] bone cyst (ABC) accounts for 1% to 2% of all primary bone tumors. The incidence of [[Aneurysmal disease|aneurysmal]] bone cyst is approximately 0.14 per 100,000 individuals worldwide. Adolescents and children are most affected by aneurysmal bone cyst. The age distribution of [[Aneurysmal disease|aneurysmal]] [[Simple bone cyst|bone cyst]] is between 1.5-25 years. The mean age of the patients with [[Aneurysmal disease|aneurysmal]] bone cyst is 16 years. Women are more commonly affected than men, with a 1:0.84 ratio. In 1942, Jaffe and Lichtenstein first described [[Aneurysmal disease|aneurysmal]] bone cyst. [[Aneurysmal disease|Aneurysmal]] bone cyst can be classified based on mechanism of origin into primary and secondary. The true causes of [[Aneurysmal disease|aneurysmal]] bone cyst are not known. ABCs usually present in the long bones such as the [[humerus]], [[femur]], [[tibia]] and [[fibula]]. About 25% of ABC's are seen in posterior element of spine. ABC's typically occur in the [[metaphysis]] of the long bones. The hallmark of ABC is Pain, swelling and [[pathological]] [[fracture]]. The mainstay of treatment for ABC is surgery in form of [[curettage]] and [[bone grafting]]. | |||
==Historical Perspective== | ==Historical Perspective== | ||
*In 1942, Jaffe and Lichtenstein first described aneurysmal bone cyst.<ref name="pmid16755186">{{cite journal| author=Mendenhall WM, Zlotecki RA, Gibbs CP, Reith JD, Scarborough MT, Mendenhall NP| title=Aneurysmal bone cyst. | journal=Am J Clin Oncol | year= 2006 | volume= 29 | issue= 3 | pages= 311-5 | pmid=16755186 | doi=10.1097/01.coc.0000204403.13451.52 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16755186 }} </ref><ref name="pmid13850355">{{cite journal| author=GODFREY LW, GRESHAM GA| title=The natural history of aneurysmal bone cyst. | journal=Proc R Soc Med | year= 1959 | volume= 52 | issue= | pages= 900-5 | pmid=13850355 | doi= | pmc=1870818 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=13850355 }} </ref> | *In 1942, Jaffe and Lichtenstein first described [[Aneurysmal disease|aneurysmal]] [[Simple bone cyst|bone cyst]].<ref name="pmid16755186">{{cite journal| author=Mendenhall WM, Zlotecki RA, Gibbs CP, Reith JD, Scarborough MT, Mendenhall NP| title=Aneurysmal bone cyst. | journal=Am J Clin Oncol | year= 2006 | volume= 29 | issue= 3 | pages= 311-5 | pmid=16755186 | doi=10.1097/01.coc.0000204403.13451.52 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16755186 }} </ref><ref name="pmid13850355">{{cite journal| author=GODFREY LW, GRESHAM GA| title=The natural history of aneurysmal bone cyst. | journal=Proc R Soc Med | year= 1959 | volume= 52 | issue= | pages= 900-5 | pmid=13850355 | doi= | pmc=1870818 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=13850355 }} </ref> | ||
*In 1940, Ewing propoosed that aneurysmal bone cyst was caused by increased venous pressure. | *In 1940, Ewing propoosed that [[Aneurysmal disease|aneurysmal]] [[Unicameral bone cyst|bone cyst]] was caused by increased [[venous]] pressure. | ||
*In 1956, Cruz and Coley also supported Ewing's hypothesis. | *In 1956, Cruz and Coley also supported Ewing's hypothesis. | ||
*In 1956, Barnes hypothesized that aneurysmal bone cyst was due to an abnormal response to injury. | *In 1956, Barnes hypothesized that aneurysmal bone cyst was due to an abnormal response to injury. | ||
*In 1956, Otterdoom after a thorough pathological study, concluded that aneurysmal bone cyst was an angioma of bone. | *In 1956, Otterdoom after a thorough pathological study, concluded that [[Aneurysmal disease|aneurysmal]] bone cyst was an [[angioma]] of bone. | ||
==Classification== | ==Classification== | ||
*Aneurysmal bone cyst(ABC) can be classified based on imaging findings and on mechanism of origin. | *[[Aneurysmal disease|Aneurysmal]] [[Simple bone cyst|bone cyst]](ABC) can be classified based on imaging findings and on mechanism of origin. | ||
===Mechanism of Origin=== | ===Mechanism of Origin=== | ||
Based on mechanism of origin, aneurysmal bone cyst can be classified into:<ref name="pmid11286830">{{cite journal| author=Feigenberg SJ, Marcus RB, Zlotecki RA, Scarborough MT, Berrey BH, Enneking WF| title=Megavoltage radiotherapy for aneurysmal bone cysts. | journal=Int J Radiat Oncol Biol Phys | year= 2001 | volume= 49 | issue= 5 | pages= 1243-7 | pmid=11286830 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11286830 }} </ref><ref name="pmid18202898">{{cite journal| author=Lin PP, Brown C, Raymond AK, Deavers MT, Yasko AW| title=Aneurysmal bone cysts recur at juxtaphyseal locations in skeletally immature patients. | journal=Clin Orthop Relat Res | year= 2008 | volume= 466 | issue= 3 | pages= 722-8 | pmid=18202898 | doi=10.1007/s11999-007-0080-8 | pmc=2505199 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18202898 }} </ref> | Based on mechanism of origin, [[Aneurysmal disease|aneurysmal]] bone cyst can be classified into:<ref name="pmid11286830">{{cite journal| author=Feigenberg SJ, Marcus RB, Zlotecki RA, Scarborough MT, Berrey BH, Enneking WF| title=Megavoltage radiotherapy for aneurysmal bone cysts. | journal=Int J Radiat Oncol Biol Phys | year= 2001 | volume= 49 | issue= 5 | pages= 1243-7 | pmid=11286830 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11286830 }} </ref><ref name="pmid18202898">{{cite journal| author=Lin PP, Brown C, Raymond AK, Deavers MT, Yasko AW| title=Aneurysmal bone cysts recur at juxtaphyseal locations in skeletally immature patients. | journal=Clin Orthop Relat Res | year= 2008 | volume= 466 | issue= 3 | pages= 722-8 | pmid=18202898 | doi=10.1007/s11999-007-0080-8 | pmc=2505199 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18202898 }} </ref> | ||
===Primary Aneurysmal Bone Cyst(ABC)=== | ===Primary Aneurysmal Bone Cyst(ABC)=== | ||
| Line 27: | Line 27: | ||
*About 30% of ABC's are secondary in origin. | *About 30% of ABC's are secondary in origin. | ||
*Commonly associated bone lesions include: | *Commonly associated bone lesions include: | ||
**Unicameral bone cyst | **[[Unicameral bone cyst]] | ||
** | **[[Osteoblastoma]] | ||
**[[Giant cell tumor]] | |||
**Giant cell tumor | **[[Enchondroma]] | ||
**Enchondroma | **[[Chondroblastoma]] | ||
**Chondroblastoma | **[[Fibrous dysplasia]] | ||
**Fibrous dysplasia | **[[Chondromyxoid fibroma]] | ||
**Chondromyxoid fibroma | **[[Nonossifying fibroma]] | ||
** | |||
===Enneking (MSTS) Staging System=== | ===Enneking (MSTS) Staging System=== | ||
*The Enneking surgical staging system (also known as the MSTS system) for benign [[Musculoskeletal system|musculoskeletal]] [[Tumor|tumors]] based on [[radiographic]] characteristics of the [[tumor]] host margin.<ref name="pmid20333492">{{cite journal| author=Jawad MU, Scully SP| title=In brief: classifications in brief: enneking classification: benign and malignant tumors of the musculoskeletal system. | journal=Clin Orthop Relat Res | year= 2010 | volume= 468 | issue= 7 | pages= 2000-2 | pmid=20333492 | doi=10.1007/s11999-010-1315-7 | pmc=2882012 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20333492 }} </ref> | *The Enneking surgical staging system (also known as the MSTS system) for benign [[Musculoskeletal system|musculoskeletal]] [[Tumor|tumors]] based on [[radiographic]] characteristics of the [[tumor]] host margin.<ref name="pmid20333492">{{cite journal| author=Jawad MU, Scully SP| title=In brief: classifications in brief: enneking classification: benign and malignant tumors of the musculoskeletal system. | journal=Clin Orthop Relat Res | year= 2010 | volume= 468 | issue= 7 | pages= 2000-2 | pmid=20333492 | doi=10.1007/s11999-010-1315-7 | pmc=2882012 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20333492 }} </ref> | ||
*It is widely accepted and routinely used classification. | *It is widely accepted and routinely used [[classification]]. | ||
{| style="border: 0px; font-size: 90%; margin: 3px; width: 1000px" align="center" | {| style="border: 0px; font-size: 90%; margin: 3px; width: 1000px" align="center" | ||
| Line 61: | Line 60: | ||
*Various theories have been proposed concerning the pathogenesis of aneurysmal bone cyst: | *Various theories have been proposed concerning the pathogenesis of aneurysmal bone cyst: | ||
**Local alteration in hemodynamics resulting in markedly increased venous pressure and development of a dilated vascular bed within the involved bone.<ref name="pmid13106840">{{cite journal| author=LICHTENSTEIN L| title=Aneurysmal bone cyst; further observations. | journal=Cancer | year= 1953 | volume= 6 | issue= 6 | pages= 1228-37 | pmid=13106840 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=13106840 }} </ref><ref name="pmid9887358">{{cite journal| author=Szendroi M, Arató G, Ezzati A, Hüttl K, Szavcsur P| title=Aneurysmal bone cyst: its pathogenesis based on angiographic, immunohistochemical and electron microscopic studies. | journal=Pathol Oncol Res | year= 1998 | volume= 4 | issue= 4 | pages= 277-81 | pmid=9887358 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9887358 }} </ref> | **Local alteration in hemodynamics resulting in markedly increased venous pressure and development of a dilated vascular bed within the involved bone.<ref name="pmid13106840">{{cite journal| author=LICHTENSTEIN L| title=Aneurysmal bone cyst; further observations. | journal=Cancer | year= 1953 | volume= 6 | issue= 6 | pages= 1228-37 | pmid=13106840 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=13106840 }} </ref><ref name="pmid9887358">{{cite journal| author=Szendroi M, Arató G, Ezzati A, Hüttl K, Szavcsur P| title=Aneurysmal bone cyst: its pathogenesis based on angiographic, immunohistochemical and electron microscopic studies. | journal=Pathol Oncol Res | year= 1998 | volume= 4 | issue= 4 | pages= 277-81 | pmid=9887358 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9887358 }} </ref> | ||
**Primary ABCs demonstrate a t(16;17)(q22;p13) fusion of the TRE17/CDH11-USP6 oncogene leading to increased cellular cadherin-11 activity which arrests osteoblastic maturation in a more primitive state.<ref name="pmid10502326">{{cite journal| author=Panoutsakopoulos G, Pandis N, Kyriazoglou I, Gustafson P, Mertens F, Mandahl N| title=Recurrent t(16;17)(q22;p13) in aneurysmal bone cysts. | journal=Genes Chromosomes Cancer | year= 1999 | volume= 26 | issue= 3 | pages= 265-6 | pmid=10502326 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10502326 }} </ref><ref name="pmid15735689">{{cite journal| author=Oliveira AM, Perez-Atayde AR, Dal Cin P, Gebhardt MC, Chen CJ, Neff JR et al.| title=Aneurysmal bone cyst variant translocations upregulate USP6 transcription by promoter swapping with the ZNF9, COL1A1, TRAP150, and OMD genes. | journal=Oncogene | year= 2005 | volume= 24 | issue= 21 | pages= 3419-26 | pmid=15735689 | doi=10.1038/sj.onc.1208506 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15735689 }} </ref><ref name="pmid10825009">{{cite journal| author=Dal Cin P, Kozakewich HP, Goumnerova L, Mankin HJ, Rosenberg AE, Fletcher JA| title=Variant translocations involving 16q22 and 17p13 in solid variant and extraosseous forms of aneurysmal bone cyst. | journal=Genes Chromosomes Cancer | year= 2000 | volume= 28 | issue= 2 | pages= 233-4 | pmid=10825009 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10825009 }} </ref> | **Primary ABCs demonstrate a t(16;17)(q22;p13) fusion of the TRE17/CDH11-USP6 oncogene leading to increased cellular cadherin-11 activity which arrests osteoblastic [[maturation]] in a more primitive state.<ref name="pmid10502326">{{cite journal| author=Panoutsakopoulos G, Pandis N, Kyriazoglou I, Gustafson P, Mertens F, Mandahl N| title=Recurrent t(16;17)(q22;p13) in aneurysmal bone cysts. | journal=Genes Chromosomes Cancer | year= 1999 | volume= 26 | issue= 3 | pages= 265-6 | pmid=10502326 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10502326 }} </ref><ref name="pmid15735689">{{cite journal| author=Oliveira AM, Perez-Atayde AR, Dal Cin P, Gebhardt MC, Chen CJ, Neff JR et al.| title=Aneurysmal bone cyst variant translocations upregulate USP6 transcription by promoter swapping with the ZNF9, COL1A1, TRAP150, and OMD genes. | journal=Oncogene | year= 2005 | volume= 24 | issue= 21 | pages= 3419-26 | pmid=15735689 | doi=10.1038/sj.onc.1208506 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15735689 }} </ref><ref name="pmid10825009">{{cite journal| author=Dal Cin P, Kozakewich HP, Goumnerova L, Mankin HJ, Rosenberg AE, Fletcher JA| title=Variant translocations involving 16q22 and 17p13 in solid variant and extraosseous forms of aneurysmal bone cyst. | journal=Genes Chromosomes Cancer | year= 2000 | volume= 28 | issue= 2 | pages= 233-4 | pmid=10825009 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10825009 }} </ref> | ||
*ABCs usually present in the long bones such as the humerus, femur, tibia; and fibula. | *ABCs usually present in the long bones such as the humerus, femur, tibia; and fibula. | ||
*About 25% of ABC's are seen in posterior element of spine. | *About 25% of ABC's are seen in posterior element of spine. | ||
*ABC's typically occur in the metaphysis of the long bones. | *ABC's typically occur in the [[metaphysis]] of the long bones. | ||
==Causes== | ==Causes== | ||
*The true causes of aneurysmal bone cyst(ABC) are not known. | *The true causes of [[Aneurysmal disease|aneurysmal]] [[Simple bone cyst|bone cyst]](ABC) are not known. | ||
*Commonly proposed theories are as follows: | *Commonly proposed theories are as follows: | ||
**ABCs may be caused by a reaction secondary to another bony lesions such as giant cell tumor, chondroblastoma, fibrous dysplasia, | **ABCs may be caused by a reaction secondary to another bony lesions such as giant cell tumor, [[chondroblastoma]], [[fibrous dysplasia]], [[osteosarcoma]] and [[chondrosarcoma]]. | ||
**ABCs may arise de novo. | **ABCs may arise de novo. | ||
**ABCs may arise secondary to previous trauma. | **ABCs may arise secondary to previous [[trauma]]. | ||
==Differentiating | ==Differentiating Aneurysmal Bone Cyst from Other Diseases== | ||
Aneurysmal bone cyst must be differentiated from following bone disorders: | Aneurysmal bone cyst must be differentiated from following bone disorders: | ||
{| | {| | ||
! | ! style="background:#4479BA; color: #FFFFFF;" align="center" + |Disease | ||
! | ! style="background:#4479BA; color: #FFFFFF;" align="center" + |'''Bubbly lytic lesion on x-ray''' | ||
! | ! style="background:#4479BA; color: #FFFFFF;" align="center" + |'''Lakes of Blood on histology''' | ||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Diagnosis | |||
! | ! style="background:#4479BA; color: #FFFFFF;" align="center" + |Treatment is curretage and bone grafting | ||
|- | |- | ||
! | ! style="background:#DCDCDC;" align="center" + |Aneurysmal bone cyst | ||
| | | style="background:#F5F5F5;" align="center" + | + | ||
| | | style="background:#F5F5F5;" align="center" + | + | ||
| | | style="background:#F5F5F5;" align="center" + |[[Radiology]] and [[biopsy]] | ||
| | | style="background:#F5F5F5;" align="center" + | + | ||
|- | |- | ||
! | ! style="background:#DCDCDC;" align="center" + |Unicameral bone cyst | ||
| | | style="background:#F5F5F5;" align="center" + | + | ||
| | | style="background:#F5F5F5;" align="center" + | - | ||
| style="background:#F5F5F5;" align="center" + |[[Radiology]] and [[biopsy]] | |||
| | | style="background:#F5F5F5;" align="center" + | - | ||
|- | |- | ||
! | ! style="background:#DCDCDC;" align="center" + |Non ossifying fibroma | ||
| | | style="background:#F5F5F5;" align="center" + | + | ||
| style="background:#F5F5F5;" align="center" + | - | |||
| | | style="background:#F5F5F5;" align="center" + |[[Radiology]] and [[biopsy]] | ||
| | | style="background:#F5F5F5;" align="center" + | - | ||
|- | |- | ||
! | ! style="background:#DCDCDC;" align="center" + |Giant cell tumor | ||
| | | style="background:#F5F5F5;" align="center" + | - | ||
| | | style="background:#F5F5F5;" align="center" + | - | ||
| | | style="background:#F5F5F5;" align="center" + |[[Radiology]] and [[Biopsy]] | ||
| | | style="background:#F5F5F5;" align="center" + | + | ||
|- | |- | ||
! | ! style="background:#DCDCDC;" align="center" + |Chondroblastoma | ||
| style="background:#F5F5F5;" align="center" + | - | |||
| | | style="background:#F5F5F5;" align="center" + | - | ||
| | | style="background:#F5F5F5;" align="center" + |[[Biopsy]] | ||
| | | style="background:#F5F5F5;" align="center" + | + | ||
|- | |- | ||
! | ! style="background:#DCDCDC;" align="center" + |Chondromyxoid Fibroma | ||
| | | style="background:#F5F5F5;" align="center" + | - | ||
| | | style="background:#F5F5F5;" align="center" + | - | ||
| | | style="background:#F5F5F5;" align="center" + |[[Radiology]] and [[biopsy]] | ||
| | | style="background:#F5F5F5;" align="center" + | + | ||
|- | |- | ||
! | ! style="background:#DCDCDC;" align="center" + |Osteoblastoma | ||
| style="background:#F5F5F5;" align="center" + | - | |||
| | | style="background:#F5F5F5;" align="center" + | - | ||
| | | style="background:#F5F5F5;" align="center" + |[[Radiology]] and [[biopsy]] | ||
| | | style="background:#F5F5F5;" align="center" + | + | ||
|- | |- | ||
! | ! style="background:#DCDCDC;" align="center" + |Telangiectatic osteosarcoma | ||
| style="background:#F5F5F5;" align="center" + | - | |||
| | | style="background:#F5F5F5;" align="center" + | + | ||
| style="background:#F5F5F5;" align="center" + |[[Radiology]] and [[biopsy]] | |||
| | | style="background:#F5F5F5;" align="center" + | - | ||
|} | |} | ||
==Epidemiology and Demographics== | ==Epidemiology and Demographics== | ||
*ABC accounts for 1% to 2% of all primary bone tumors.<ref name="pmid10379320">{{cite journal| author=Leithner A, Windhager R, Lang S, Haas OA, Kainberger F, Kotz R| title=Aneurysmal bone cyst. A population based epidemiologic study and literature review. | journal=Clin Orthop Relat Res | year= 1999 | volume= | issue= 363 | pages= 176-9 | pmid=10379320 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10379320 }} </ref> | *ABC accounts for 1% to 2% of all primary [[bone tumors]].<ref name="pmid10379320">{{cite journal| author=Leithner A, Windhager R, Lang S, Haas OA, Kainberger F, Kotz R| title=Aneurysmal bone cyst. A population based epidemiologic study and literature review. | journal=Clin Orthop Relat Res | year= 1999 | volume= | issue= 363 | pages= 176-9 | pmid=10379320 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10379320 }} </ref> | ||
*The incidence of aneurysmal bone cyst is approximately 0.14 per 100,000 individuals worldwide.<ref name="pmid10379320">{{cite journal| author=Leithner A, Windhager R, Lang S, Haas OA, Kainberger F, Kotz R| title=Aneurysmal bone cyst. A population based epidemiologic study and literature review. | journal=Clin Orthop Relat Res | year= 1999 | volume= | issue= 363 | pages= 176-9 | pmid=10379320 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10379320 }} </ref> | *The incidence of [[Aneurysmal Disease|aneurysmal]] [[Simple bone cyst|bone cyst]] is approximately 0.14 per 100,000 individuals worldwide.<ref name="pmid10379320">{{cite journal| author=Leithner A, Windhager R, Lang S, Haas OA, Kainberger F, Kotz R| title=Aneurysmal bone cyst. A population based epidemiologic study and literature review. | journal=Clin Orthop Relat Res | year= 1999 | volume= | issue= 363 | pages= 176-9 | pmid=10379320 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10379320 }} </ref> | ||
*Adolescents and children are most affected by | *Adolescents and children are most affected by [[Aneurysmal Disease|aneurysma]]<nowiki/>l [[Simple bone cyst|bone cyst]]. | ||
*The age distribution of | *The age distribution of [[Aneurysmal Disease|aneurysmal]] [[Simple bone cyst|bone cyst]] is between 1.5-25 years.<ref name="pmid28208959">{{cite journal| author=Mohan R, Sreekumaran GT| title=Secondary Aneurysmal Bone Cyst of the Scapula Treated by CT Guided Percutaneous Polidocanol Injection - A Case Report. | journal=J Clin Diagn Res | year= 2016 | volume= 10 | issue= 12 | pages= RD04-RD06 | pmid=28208959 | doi=10.7860/JCDR/2016/23561.9096 | pmc=5296532 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28208959 }} </ref><ref name="pmid5458269">{{cite journal| author=Biesecker JL, Marcove RC, Huvos AG, Miké V| title=Aneurysmal bone cysts. A clinicopathologic study of 66 cases. | journal=Cancer | year= 1970 | volume= 26 | issue= 3 | pages= 615-25 | pmid=5458269 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=5458269 }} </ref> | ||
*The mean age of the patients with aneurysmal bone cyst is 16 years.<ref name="pmid265751">{{cite journal| author=Ruiter DJ, van Rijssel TG, van der Velde EA| title=Aneurysmal bone cysts: a clinicopathological study of 105 cases. | journal=Cancer | year= 1977 | volume= 39 | issue= 5 | pages= 2231-9 | pmid=265751 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=265751 }} </ref> | *The mean age of the patients with [[Aneurysmal Disease|aneurysmal]] [[Simple bone cyst|bone cyst]] is 16 years.<ref name="pmid265751">{{cite journal| author=Ruiter DJ, van Rijssel TG, van der Velde EA| title=Aneurysmal bone cysts: a clinicopathological study of 105 cases. | journal=Cancer | year= 1977 | volume= 39 | issue= 5 | pages= 2231-9 | pmid=265751 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=265751 }} </ref> | ||
*Women are more commonly affected than men, with a 1:0.84 ratio.<ref name="pmid1591685">{{cite journal| author=Vergel De Dios AM, Bond JR, Shives TC, McLeod RA, Unni KK| title=Aneurysmal bone cyst. A clinicopathologic study of 238 cases. | journal=Cancer | year= 1992 | volume= 69 | issue= 12 | pages= 2921-31 | pmid=1591685 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1591685 }} </ref> | *Women are more commonly affected than men, with a 1:0.84 ratio.<ref name="pmid1591685">{{cite journal| author=Vergel De Dios AM, Bond JR, Shives TC, McLeod RA, Unni KK| title=Aneurysmal bone cyst. A clinicopathologic study of 238 cases. | journal=Cancer | year= 1992 | volume= 69 | issue= 12 | pages= 2921-31 | pmid=1591685 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1591685 }} </ref> | ||
*There is no racial predilection to aneurysmal bone cyst. | *There is no racial predilection to [[Aneurysmal disease|aneurysmal]] [[Simple bone cyst|bone cyst]]. | ||
==Risk Factors== | ==Risk Factors== | ||
There are no established risk factors for aneurysmal bone cyst. | There are no established risk factors for [[Aneurysmal disease|aneurysmal]] [[Simple bone cyst|bone cyst]]. | ||
==Screening== | ==Screening== | ||
| Line 147: | Line 146: | ||
==Natural History, Complications, and Prognosis== | ==Natural History, Complications, and Prognosis== | ||
*Common complications of aneurysmal bone cyst include:<ref name="pmid10608377">{{cite journal| author=Gibbs CP, Hefele MC, Peabody TD, Montag AG, Aithal V, Simon MA| title=Aneurysmal bone cyst of the extremities. Factors related to local recurrence after curettage with a high-speed burr. | journal=J Bone Joint Surg Am | year= 1999 | volume= 81 | issue= 12 | pages= 1671-8 | pmid=10608377 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10608377 }} </ref><ref name="pmid9530795">{{cite journal| author=Papagelopoulos PJ, Currier BL, Shaughnessy WJ, Sim FH, Ebsersold MJ, Bond JR et al.| title=Aneurysmal bone cyst of the spine. Management and outcome. | journal=Spine (Phila Pa 1976) | year= 1998 | volume= 23 | issue= 5 | pages= 621-8 | pmid=9530795 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9530795 }} </ref> | *Common complications of [[Aneurysmal disease|aneurysmal]] [[Simple bone cyst|bone cyst]] include:<ref name="pmid10608377">{{cite journal| author=Gibbs CP, Hefele MC, Peabody TD, Montag AG, Aithal V, Simon MA| title=Aneurysmal bone cyst of the extremities. Factors related to local recurrence after curettage with a high-speed burr. | journal=J Bone Joint Surg Am | year= 1999 | volume= 81 | issue= 12 | pages= 1671-8 | pmid=10608377 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10608377 }} </ref><ref name="pmid9530795">{{cite journal| author=Papagelopoulos PJ, Currier BL, Shaughnessy WJ, Sim FH, Ebsersold MJ, Bond JR et al.| title=Aneurysmal bone cyst of the spine. Management and outcome. | journal=Spine (Phila Pa 1976) | year= 1998 | volume= 23 | issue= 5 | pages= 621-8 | pmid=9530795 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9530795 }} </ref> | ||
**Pathological fracture | **[[Pathological]] [[fracture]] | ||
**Premature epiphyseal closure | **Premature [[epiphyseal]] closure | ||
***Limb-length discrepancy | ***Limb-length discrepancy | ||
***Angular deformity | ***Angular deformity | ||
**Malignant transformations to form malignant osteosarcoma. | **[[Malignant]] transformations to form [[malignant]] [[osteosarcoma]]. | ||
*Prognosis is generally excellent for aneurysmal bone cyst. | *Prognosis is generally excellent for [[Aneurysmal Disease|aneurysmal]] [[Simple bone cyst|bone cyst]]. | ||
*Factors that influence the outcome of the aneurysmal bone cyst include: | *Factors that influence the outcome of the [[Aneurysmal Disease|aneurysmal]] [[Simple bone cyst|bone cyst]] include: | ||
**Young age | **Young age | ||
**Open growth | **Open [[growth plate]]<nowiki/>s | ||
**Metaphyseal location | **[[Metaphyseal]] location | ||
==Diagnosis== | ==Diagnosis== | ||
| Line 166: | Line 165: | ||
|} | |} | ||
*Biopsy is the diagnostic study of choice for the diagnosis of | *[[Biopsy punch|Biopsy]] is the diagnostic study of choice for the diagnosis of [[Aneurysmal disease|aneurysma]]<nowiki/>l bone cyst.<ref name="pmid12619099">{{cite journal| author=Yamamoto T, Nagira K, Akisue T, Marui T, Hitora T, Kawamoto T et al.| title=Fine-needle aspiration biopsy of solid aneurysmal bone cyst in the humerus. | journal=Diagn Cytopathol | year= 2003 | volume= 28 | issue= 3 | pages= 159-62 | pmid=12619099 | doi=10.1002/dc.10248 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12619099 }} </ref><ref name="pmid2835141">{{cite journal| author=Martinez V, Sissons HA| title=Aneurysmal bone cyst. A review of 123 cases including primary lesions and those secondary to other bone pathology. | journal=Cancer | year= 1988 | volume= 61 | issue= 11 | pages= 2291-304 | pmid=2835141 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2835141 }} </ref> | ||
*Gross appearance of aneurysmal bone cyst include: | *Gross appearance of [[Aneurysmal Disease|aneurysmal]] [[Simple bone cyst|bone cyst]] include: | ||
**Blood-soaked sponge. | **Blood-soaked sponge. | ||
**A thin subperiosteal shell of new bone surrounds the structure | **A thin [[subperiosteal]] shell of new bone surrounds the structure | ||
**Cystic blood-filled cavities. | **[[Cystic]] blood-filled cavities. | ||
**The tissue within shows brownish intertwining septa. | **The tissue within shows brownish intertwining [[septa]]. | ||
**The stroma contains proliferative fibroblasts, spindle cells, areas of osteoid formation, and an uneven distribution of multinucleated giant cells that tend to surround the fluid-filled cavities in a pigs at the trough formation. | **The [[stroma]] contains proliferative [[fibroblasts]], [[spindle cells]], areas of [[osteoid]] formation, and an uneven distribution of [[multinucleated]] [[giant cells]] that tend to surround the fluid-filled cavities in a pigs at the trough formation. | ||
*HIstological appearance includes: | *HIstological appearance includes: | ||
**Cavernous space | **[[Cavernous]] space | ||
**Blood-filled spaces without endothelial lining | **Blood-filled spaces without [[endothelial]] lining | ||
**Cavity lining with numerous benign giant cells and spindle cells with thin strands of woven bone present | **Cavity lining with numerous benign [[giant cells]] and spindle cells with thin strands of woven bone present | ||
===History and Symptoms=== | ===History and Symptoms=== | ||
*The majority of patients with | *The majority of patients with [[Aneurysmal disease|aneurysmal]] [[Simple bone cyst|bone cyst]] have a positive history of: | ||
**Pain | **Pain | ||
**Swelling | **[[Swelling]] | ||
**Pathological fracture | **[[Pathological]] [[fracture]] | ||
Neurologic conditions occur often due to compression of either the spinal cord or nerve | **[[Neurologic]] conditions occur often due to compression of either the [[spinal cord]] or [[nerve root]]<nowiki/>s, and may lead to [[paralysis]] and spinal stiffness | ||
===Physical Examination=== | ===Physical Examination=== | ||
*Common physical examination findings of aneurysmal bone cyst include: | {| align="right" | ||
**Deformity | | | ||
[[File:X ray aneurysmal-bone-cyst.jpg|200px|thumb|X-ray showing aneurysmal bone cyst of left proximal femur.[https://radiopaedia.org/cases/aneurysmal-bone-cyst-12?lang=us Source: Case courtesy of Dr Lawrence Chia Wei Oh, Radiopaedia.org, rID: 28998]]] | |||
|} | |||
*Common physical examination findings of [[Aneurysmal Disease|aneurysmal]] bone cyst include: | |||
**[[Deformity]] | |||
**Decreased range of motion, weakness, or stiffness | **Decreased range of motion, weakness, or stiffness | ||
**Torticollis | **[[Torticollis (patient information)|Torticollis]] | ||
**Occasionally, bruit over the affected area | **Occasionally, [[bruit]] over the affected area | ||
**Warmth over the affected area | **Warmth over the affected area | ||
===Laboratory Findings=== | ===Laboratory Findings=== | ||
There are no diagnostic laboratory findings associated with aneurysmal bone cyst. | There are no diagnostic laboratory findings associated with [[Aneurysmal disease|aneurysmal]] bone cyst. | ||
===Electrocardiogram=== | ===Electrocardiogram=== | ||
There are no ECG findings associated with aneurysmal bone cyst. | There are no [[ECG]] findings associated with [[Aneurysmal disease|aneurysmal]] bone cyst. | ||
===X-ray=== | ===X-ray=== | ||
*An x-ray may be helpful in the diagnosis of aneurysmal bone cyst. | *An [[x-ray]] may be helpful in the diagnosis of [[Aneurysmal disease|aneurysmal]] bone cyst. | ||
*Findings on an x-ray suggestive of aneurysmal bone cyst include include:<ref name="pmid5656741">{{cite journal| author=Nobler MP, Higinbotham NL, Phillips RF| title=The cure of aneurysmal bone cyst. Irradiation superior to surgery in an analysis of 33 cases. | journal=Radiology | year= 1968 | volume= 90 | issue= 6 | pages= 1185-92 | pmid=5656741 | doi=10.1148/90.6.1185 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=5656741 }} </ref> | *Findings on an [[x-ray]] suggestive of [[Aneurysmal disease|aneurysmal]] bone cyst include include:<ref name="pmid5656741">{{cite journal| author=Nobler MP, Higinbotham NL, Phillips RF| title=The cure of aneurysmal bone cyst. Irradiation superior to surgery in an analysis of 33 cases. | journal=Radiology | year= 1968 | volume= 90 | issue= 6 | pages= 1185-92 | pmid=5656741 | doi=10.1148/90.6.1185 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=5656741 }} </ref> | ||
**Expansile, eccentric and lytic lesion with bony septae giving it a soap bubble appearance. | **Expansile, eccentric and lytic lesion with bony septae giving it a soap bubble appearance. | ||
**Involves the metaphyseal area of the bone | **Involves the [[Metaphysis|metaphyseal]] area of the bone | ||
**Thin rim of periosteal new bone surrounding lesion | **Thin rim of [[Periosteal chondroma|periosteal]] new bone surrounding lesion | ||
**No matrix mineralization | **No [[matrix]] [[mineralization]] | ||
{| align="right" | |||
| | |||
[[File:CT scan aneurysmal-bone-cyst.jpg|200px|thumb|CT scan showing aneurysmal bone cyst of posterior element of spine.[https://radiopaedia.org/cases/aneurysmal-bone-cyst-t11?lang=us Source: Case courtesy of RMH Neuropathology, Radiopaedia.org, rID: 29294]]] | |||
|} | |||
*Radiologically aneurysmal bone cyst can be stratified into 4 phases:<ref name="pmid5764977">{{cite journal| author=Dabska M, Buraczewski J| title=Aneurysmal bone cyst. Pathology, clinical course and radiologic appearances. | journal=Cancer | year= 1969 | volume= 23 | issue= 2 | pages= 371-89 | pmid=5764977 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=5764977 }} </ref> | *Radiologically aneurysmal bone cyst can be stratified into 4 phases:<ref name="pmid5764977">{{cite journal| author=Dabska M, Buraczewski J| title=Aneurysmal bone cyst. Pathology, clinical course and radiologic appearances. | journal=Cancer | year= 1969 | volume= 23 | issue= 2 | pages= 371-89 | pmid=5764977 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=5764977 }} </ref> | ||
**Initial phase 1 – Small, lytic lesion without evidence of lifting off of the periosteum. | **Initial phase 1 – Small, lytic lesion without evidence of lifting off of the [[periosteum]]. | ||
**Phase 2 - Rapidly enlarging demonstrating a characteristic blowout appearance. | **Phase 2 - Rapidly enlarging demonstrating a characteristic blowout appearance. | ||
**Phase 3 - Growth slows or stops after some sort of intervention. | **Phase 3 - Growth slows or stops after some sort of intervention. | ||
| Line 215: | Line 220: | ||
===Echocardiography or Ultrasound=== | ===Echocardiography or Ultrasound=== | ||
There are no echocardiography/ultrasound findings associated with aneurysmal bone cyst. | There are no [[echocardiography]]/[[ultrasound]] findings associated with aneurysmal bone cyst. | ||
===CT scan=== | ===CT scan=== | ||
*CT scan confirms the x-ray findings.<ref name="pmid2160676">{{cite journal| author=Tsai JC, Dalinka MK, Fallon MD, Zlatkin MB, Kressel HY| title=Fluid-fluid level: a nonspecific finding in tumors of bone and soft tissue. | journal=Radiology | year= 1990 | volume= 175 | issue= 3 | pages= 779-82 | pmid=2160676 | doi=10.1148/radiology.175.3.2160676 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2160676 }} </ref> | *[[CT scan]] confirms the x-ray findings.<ref name="pmid2160676">{{cite journal| author=Tsai JC, Dalinka MK, Fallon MD, Zlatkin MB, Kressel HY| title=Fluid-fluid level: a nonspecific finding in tumors of bone and soft tissue. | journal=Radiology | year= 1990 | volume= 175 | issue= 3 | pages= 779-82 | pmid=2160676 | doi=10.1148/radiology.175.3.2160676 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2160676 }} </ref> | ||
*In addition, | *In addition, CT demonstrates internal septation such as [[Calcification|calcified]] rim, giving an eggshell appearance, which may be completely or partially intact. | ||
*Fluid-fluid levels can also be seen. | *Fluid-fluid levels can also be seen. | ||
===MRI=== | ===MRI=== | ||
*Magnetic resonance imaging (MRI) are similar to those from CT scan.<ref name="pmid24244797">{{cite journal| author=Boubbou M, Atarraf K, Chater L, Afifi A, Tizniti S| title=Aneurysmal bone cyst primary--about eight pediatric cases: radiological aspects and review of the literature. | journal=Pan Afr Med J | year= 2013 | volume= 15 | issue= | pages= 111 | pmid=24244797 | doi=10.11604/pamj.2013.15.111.2117 | pmc=3828064 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24244797 }} </ref> | *[[Magnetic resonance imaging]] (MRI) are similar to those from [[CT scan]].<ref name="pmid24244797">{{cite journal| author=Boubbou M, Atarraf K, Chater L, Afifi A, Tizniti S| title=Aneurysmal bone cyst primary--about eight pediatric cases: radiological aspects and review of the literature. | journal=Pan Afr Med J | year= 2013 | volume= 15 | issue= | pages= 111 | pmid=24244797 | doi=10.11604/pamj.2013.15.111.2117 | pmc=3828064 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24244797 }} </ref> | ||
*However, MRI can more specifically reveal blood within the lesion as well as extension into the soft tissues. | *However, [[MRI]] can more specifically reveal blood within the lesion as well as extension into the soft tissues. | ||
{| align="right" | |||
| | |||
[[File:MRI aneurysmal-bone-cyst.jpg|200px|thumb|MRI showing aneurysmal bone cyst of left proximal femur.[https://radiopaedia.org/cases/aneurysmal-bone-cyst-12?lang=us Source: Case courtesy of Dr Lawrence Chia Wei Oh, Radiopaedia.org, rID: 28998]]] | |||
|} | |||
===Other Imaging Findings=== | ===Other Imaging Findings=== | ||
===Bone Scan=== | ===Bone Scan=== | ||
*Increased uptake is observed around the lesion of aneurysmal bone cyst. | *Increased uptake is observed around the lesion of [[Aneurysmal disease|aneurysmal]] bone cyst. | ||
*Findings often demonstrate a halo effect of increased radionuclide uptake surrounding an area of little uptake. | *Findings often demonstrate a halo effect of increased radionuclide uptake surrounding an area of little uptake. | ||
===Other Diagnostic Studies=== | ===Other Diagnostic Studies=== | ||
===Angiography=== | ===Angiography=== | ||
*Angiography demonstrates a hypervascular area around the aneurysmal bone cyst. | *[[Angiography]] demonstrates a hypervascular area around the [[Aneurysmal Disease|aneurysmal]] bone cyst. | ||
*An intense diffuse area of persistent contrast accumulation may be visualized without main afferent or efferent vessels observed. | *An intense diffuse area of persistent contrast accumulation may be visualized without main afferent or efferent [[vessels]] observed. | ||
*It can be helpful to plan selective arterial embolization as the primary treatment or as a preoperative method to help control intraoperative blood loss. | *It can be helpful to plan selective [[arterial]] [[embolization]] as the primary treatment or as a preoperative method to help control intraoperative [[blood loss]]. | ||
==Treatment== | ==Treatment== | ||
===Medical Therapy=== | ===Medical Therapy=== | ||
There is no treatment for aneurysmal bone cyst | There is no treatment for [[Aneurysmal disease|aneurysmal]] bone cyst, the mainstay of therapy is [[surgery]]. | ||
===Surgery=== | ===Surgery=== | ||
*Surgery is the mainstay of treatment for aneurysmal bone cyst.<ref name="pmid10608377">{{cite journal| author=Gibbs CP, Hefele MC, Peabody TD, Montag AG, Aithal V, Simon MA| title=Aneurysmal bone cyst of the extremities. Factors related to local recurrence after curettage with a high-speed burr. | journal=J Bone Joint Surg Am | year= 1999 | volume= 81 | issue= 12 | pages= 1671-8 | pmid=10608377 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10608377 }} </ref><ref name="pmid9137195">{{cite journal| author=Ozaki T, Hillmann A, Lindner N, Winkelmann W| title=Cementation of primary aneurysmal bone cysts. | journal=Clin Orthop Relat Res | year= 1997 | volume= | issue= 337 | pages= 240-8 | pmid=9137195 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9137195 }} </ref><ref name="pmid24532435">{{cite journal| author=Reddy KI, Sinnaeve F, Gaston CL, Grimer RJ, Carter SR| title=Aneurysmal bone cysts: do simple treatments work? | journal=Clin Orthop Relat Res | year= 2014 | volume= 472 | issue= 6 | pages= 1901-10 | pmid=24532435 | doi=10.1007/s11999-014-3513-1 | pmc=4016447 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24532435 }} </ref> | *Surgery is the mainstay of treatment for [[Aneurysmal disease|aneurysmal]] bone cyst.<ref name="pmid10608377">{{cite journal| author=Gibbs CP, Hefele MC, Peabody TD, Montag AG, Aithal V, Simon MA| title=Aneurysmal bone cyst of the extremities. Factors related to local recurrence after curettage with a high-speed burr. | journal=J Bone Joint Surg Am | year= 1999 | volume= 81 | issue= 12 | pages= 1671-8 | pmid=10608377 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10608377 }} </ref><ref name="pmid9137195">{{cite journal| author=Ozaki T, Hillmann A, Lindner N, Winkelmann W| title=Cementation of primary aneurysmal bone cysts. | journal=Clin Orthop Relat Res | year= 1997 | volume= | issue= 337 | pages= 240-8 | pmid=9137195 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9137195 }} </ref><ref name="pmid24532435">{{cite journal| author=Reddy KI, Sinnaeve F, Gaston CL, Grimer RJ, Carter SR| title=Aneurysmal bone cysts: do simple treatments work? | journal=Clin Orthop Relat Res | year= 2014 | volume= 472 | issue= 6 | pages= 1901-10 | pmid=24532435 | doi=10.1007/s11999-014-3513-1 | pmc=4016447 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24532435 }} </ref> | ||
===Aggressive curettage with adjuvant and bone grafting=== | ===Aggressive curettage with adjuvant and bone grafting=== | ||
| Line 251: | Line 261: | ||
'''Technique''' | '''Technique''' | ||
*Possible adjuvants | *Possible adjuvants | ||
**Phenol | **[[Phenol]] | ||
**Argon beam | **Argon beam | ||
**Liquid nitrogen | **[[Liquid nitrogen]] | ||
'''Recurrence''' | '''Recurrence''' | ||
*Local recurrence in up to 25% and more common in children with open | *Local recurrence in up to 25% and more common in children with open ephyses. | ||
===Primary Prevention=== | ===Primary Prevention=== | ||
There are no established measures for the primary prevention of aneurysmal bone cyst. | There are no established measures for the [[primary prevention]] of [[Aneurysmal disease|aneurysmal]] bone cyst. | ||
===Secondary Prevention=== | ===Secondary Prevention=== | ||
There are no established measures for the secondary prevention of aneurysmal bone cyst. | There are no established measures for the [[secondary prevention]] of [[Aneurysmal disease|aneurysmal]] bone cyst. | ||
==References== | ==References== | ||
Latest revision as of 18:00, 10 April 2019
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Rohan A. Bhimani, M.B.B.S., D.N.B., M.Ch.[2]
Overview
Aneurysmal bone cyst (ABC) accounts for 1% to 2% of all primary bone tumors. The incidence of aneurysmal bone cyst is approximately 0.14 per 100,000 individuals worldwide. Adolescents and children are most affected by aneurysmal bone cyst. The age distribution of aneurysmal bone cyst is between 1.5-25 years. The mean age of the patients with aneurysmal bone cyst is 16 years. Women are more commonly affected than men, with a 1:0.84 ratio. In 1942, Jaffe and Lichtenstein first described aneurysmal bone cyst. Aneurysmal bone cyst can be classified based on mechanism of origin into primary and secondary. The true causes of aneurysmal bone cyst are not known. ABCs usually present in the long bones such as the humerus, femur, tibia and fibula. About 25% of ABC's are seen in posterior element of spine. ABC's typically occur in the metaphysis of the long bones. The hallmark of ABC is Pain, swelling and pathological fracture. The mainstay of treatment for ABC is surgery in form of curettage and bone grafting.
Historical Perspective
- In 1942, Jaffe and Lichtenstein first described aneurysmal bone cyst.[1][2]
- In 1940, Ewing propoosed that aneurysmal bone cyst was caused by increased venous pressure.
- In 1956, Cruz and Coley also supported Ewing's hypothesis.
- In 1956, Barnes hypothesized that aneurysmal bone cyst was due to an abnormal response to injury.
- In 1956, Otterdoom after a thorough pathological study, concluded that aneurysmal bone cyst was an angioma of bone.
Classification
- Aneurysmal bone cyst(ABC) can be classified based on imaging findings and on mechanism of origin.
Mechanism of Origin
Based on mechanism of origin, aneurysmal bone cyst can be classified into:[3][4]
Primary Aneurysmal Bone Cyst(ABC)
- When ABC arises de novo, it is called primary ABC.
- About 70% of ABC's are primary in origin.
Secondary Aneurysmal Bone Cyst(ABC)
- When ABC coexist with other bone lesions, it is termed as secondary ABC's.
- About 30% of ABC's are secondary in origin.
- Commonly associated bone lesions include:
Enneking (MSTS) Staging System
- The Enneking surgical staging system (also known as the MSTS system) for benign musculoskeletal tumors based on radiographic characteristics of the tumor host margin.[5]
- It is widely accepted and routinely used classification.
| Stages | Description |
|---|---|
| 1 | Latent: Well demarcated borders |
| 2 | Active: Indistinct borders |
| 3 | Aggressive: Indistinct borders |
Pathophysiology
- The exact pathogenesis of aneurysmal bone cyst is not fully understood.[6][7]
- Various theories have been proposed concerning the pathogenesis of aneurysmal bone cyst:
- Local alteration in hemodynamics resulting in markedly increased venous pressure and development of a dilated vascular bed within the involved bone.[8][9]
- Primary ABCs demonstrate a t(16;17)(q22;p13) fusion of the TRE17/CDH11-USP6 oncogene leading to increased cellular cadherin-11 activity which arrests osteoblastic maturation in a more primitive state.[10][11][12]
- ABCs usually present in the long bones such as the humerus, femur, tibia; and fibula.
- About 25% of ABC's are seen in posterior element of spine.
- ABC's typically occur in the metaphysis of the long bones.
Causes
- The true causes of aneurysmal bone cyst(ABC) are not known.
- Commonly proposed theories are as follows:
- ABCs may be caused by a reaction secondary to another bony lesions such as giant cell tumor, chondroblastoma, fibrous dysplasia, osteosarcoma and chondrosarcoma.
- ABCs may arise de novo.
- ABCs may arise secondary to previous trauma.
Differentiating Aneurysmal Bone Cyst from Other Diseases
Aneurysmal bone cyst must be differentiated from following bone disorders:
| Disease | Bubbly lytic lesion on x-ray | Lakes of Blood on histology | Diagnosis | Treatment is curretage and bone grafting |
|---|---|---|---|---|
| Aneurysmal bone cyst | + | + | Radiology and biopsy | + |
| Unicameral bone cyst | + | - | Radiology and biopsy | - |
| Non ossifying fibroma | + | - | Radiology and biopsy | - |
| Giant cell tumor | - | - | Radiology and Biopsy | + |
| Chondroblastoma | - | - | Biopsy | + |
| Chondromyxoid Fibroma | - | - | Radiology and biopsy | + |
| Osteoblastoma | - | - | Radiology and biopsy | + |
| Telangiectatic osteosarcoma | - | + | Radiology and biopsy | - |
Epidemiology and Demographics
- ABC accounts for 1% to 2% of all primary bone tumors.[13]
- The incidence of aneurysmal bone cyst is approximately 0.14 per 100,000 individuals worldwide.[13]
- Adolescents and children are most affected by aneurysmal bone cyst.
- The age distribution of aneurysmal bone cyst is between 1.5-25 years.[14][15]
- The mean age of the patients with aneurysmal bone cyst is 16 years.[16]
- Women are more commonly affected than men, with a 1:0.84 ratio.[17]
- There is no racial predilection to aneurysmal bone cyst.
Risk Factors
There are no established risk factors for aneurysmal bone cyst.
Screening
There is insufficient evidence to recommend routine screening for aneurysmal bone cyst.
Natural History, Complications, and Prognosis
- Common complications of aneurysmal bone cyst include:[18][19]
- Pathological fracture
- Premature epiphyseal closure
- Limb-length discrepancy
- Angular deformity
- Malignant transformations to form malignant osteosarcoma.
- Prognosis is generally excellent for aneurysmal bone cyst.
- Factors that influence the outcome of the aneurysmal bone cyst include:
- Young age
- Open growth plates
- Metaphyseal location
Diagnosis
Diagnostic Study of Choice
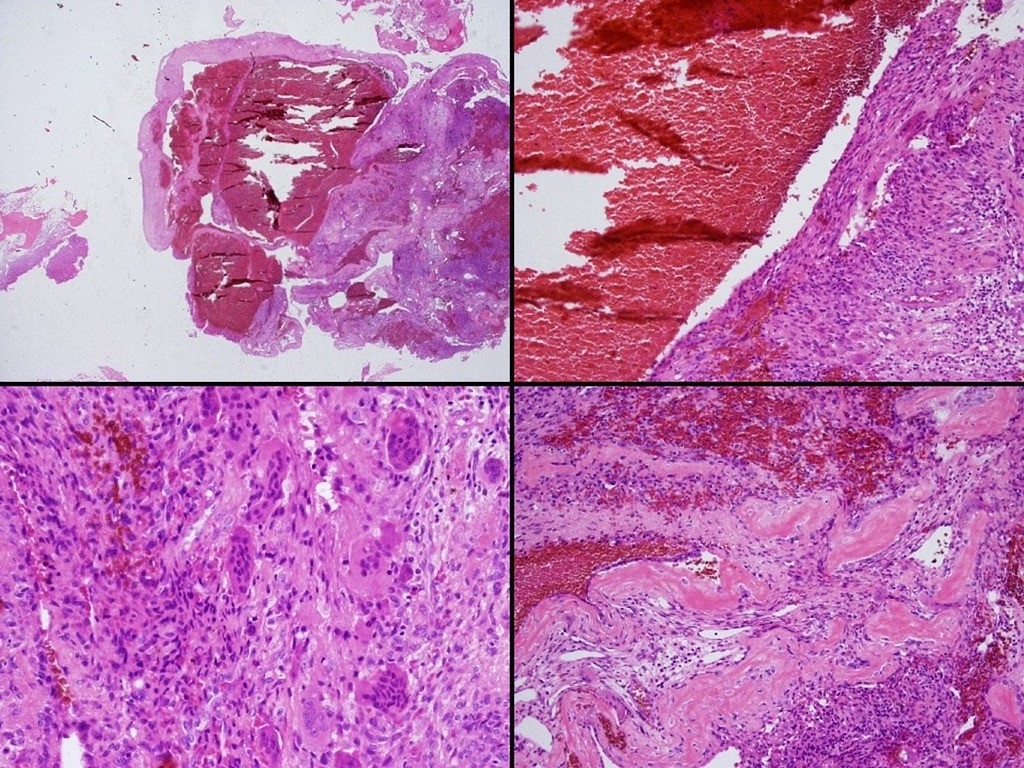 |
- Biopsy is the diagnostic study of choice for the diagnosis of aneurysmal bone cyst.[20][21]
- Gross appearance of aneurysmal bone cyst include:
- Blood-soaked sponge.
- A thin subperiosteal shell of new bone surrounds the structure
- Cystic blood-filled cavities.
- The tissue within shows brownish intertwining septa.
- The stroma contains proliferative fibroblasts, spindle cells, areas of osteoid formation, and an uneven distribution of multinucleated giant cells that tend to surround the fluid-filled cavities in a pigs at the trough formation.
- HIstological appearance includes:
- Cavernous space
- Blood-filled spaces without endothelial lining
- Cavity lining with numerous benign giant cells and spindle cells with thin strands of woven bone present
History and Symptoms
- The majority of patients with aneurysmal bone cyst have a positive history of:
- Pain
- Swelling
- Pathological fracture
- Neurologic conditions occur often due to compression of either the spinal cord or nerve roots, and may lead to paralysis and spinal stiffness
Physical Examination
 |
- Common physical examination findings of aneurysmal bone cyst include:
- Deformity
- Decreased range of motion, weakness, or stiffness
- Torticollis
- Occasionally, bruit over the affected area
- Warmth over the affected area
Laboratory Findings
There are no diagnostic laboratory findings associated with aneurysmal bone cyst.
Electrocardiogram
There are no ECG findings associated with aneurysmal bone cyst.
X-ray
- An x-ray may be helpful in the diagnosis of aneurysmal bone cyst.
- Findings on an x-ray suggestive of aneurysmal bone cyst include include:[22]
- Expansile, eccentric and lytic lesion with bony septae giving it a soap bubble appearance.
- Involves the metaphyseal area of the bone
- Thin rim of periosteal new bone surrounding lesion
- No matrix mineralization
 |
- Radiologically aneurysmal bone cyst can be stratified into 4 phases:[23]
- Initial phase 1 – Small, lytic lesion without evidence of lifting off of the periosteum.
- Phase 2 - Rapidly enlarging demonstrating a characteristic blowout appearance.
- Phase 3 - Growth slows or stops after some sort of intervention.
- Phase 4 - Healing with progressive ossification and calcification of the cavity.
Echocardiography or Ultrasound
There are no echocardiography/ultrasound findings associated with aneurysmal bone cyst.
CT scan
- CT scan confirms the x-ray findings.[24]
- In addition, CT demonstrates internal septation such as calcified rim, giving an eggshell appearance, which may be completely or partially intact.
- Fluid-fluid levels can also be seen.
MRI
- Magnetic resonance imaging (MRI) are similar to those from CT scan.[25]
- However, MRI can more specifically reveal blood within the lesion as well as extension into the soft tissues.
 |
Other Imaging Findings
Bone Scan
- Increased uptake is observed around the lesion of aneurysmal bone cyst.
- Findings often demonstrate a halo effect of increased radionuclide uptake surrounding an area of little uptake.
Other Diagnostic Studies
Angiography
- Angiography demonstrates a hypervascular area around the aneurysmal bone cyst.
- An intense diffuse area of persistent contrast accumulation may be visualized without main afferent or efferent vessels observed.
- It can be helpful to plan selective arterial embolization as the primary treatment or as a preoperative method to help control intraoperative blood loss.
Treatment
Medical Therapy
There is no treatment for aneurysmal bone cyst, the mainstay of therapy is surgery.
Surgery
- Surgery is the mainstay of treatment for aneurysmal bone cyst.[18][26][27]
Aggressive curettage with adjuvant and bone grafting
Indications
- Symptomatic aneurysmal bone cyst without acute fracture
Technique
- Possible adjuvants
- Phenol
- Argon beam
- Liquid nitrogen
Recurrence
- Local recurrence in up to 25% and more common in children with open ephyses.
Primary Prevention
There are no established measures for the primary prevention of aneurysmal bone cyst.
Secondary Prevention
There are no established measures for the secondary prevention of aneurysmal bone cyst.
References
- ↑ Mendenhall WM, Zlotecki RA, Gibbs CP, Reith JD, Scarborough MT, Mendenhall NP (2006). "Aneurysmal bone cyst". Am J Clin Oncol. 29 (3): 311–5. doi:10.1097/01.coc.0000204403.13451.52. PMID 16755186.
- ↑ GODFREY LW, GRESHAM GA (1959). "The natural history of aneurysmal bone cyst". Proc R Soc Med. 52: 900–5. PMC 1870818. PMID 13850355.
- ↑ Feigenberg SJ, Marcus RB, Zlotecki RA, Scarborough MT, Berrey BH, Enneking WF (2001). "Megavoltage radiotherapy for aneurysmal bone cysts". Int J Radiat Oncol Biol Phys. 49 (5): 1243–7. PMID 11286830.
- ↑ Lin PP, Brown C, Raymond AK, Deavers MT, Yasko AW (2008). "Aneurysmal bone cysts recur at juxtaphyseal locations in skeletally immature patients". Clin Orthop Relat Res. 466 (3): 722–8. doi:10.1007/s11999-007-0080-8. PMC 2505199. PMID 18202898.
- ↑ Jawad MU, Scully SP (2010). "In brief: classifications in brief: enneking classification: benign and malignant tumors of the musculoskeletal system". Clin Orthop Relat Res. 468 (7): 2000–2. doi:10.1007/s11999-010-1315-7. PMC 2882012. PMID 20333492.
- ↑ Peabody, Terrance (2014). Orthopaedic oncology : primary and metastatic tumors of the skeletal system. Cham: Springer. ISBN 9783319073224.
- ↑ Cottalorda J, Bourelle S (2007). "Modern concepts of primary aneurysmal bone cyst". Arch Orthop Trauma Surg. 127 (2): 105–14. doi:10.1007/s00402-006-0223-5. PMID 16937137.
- ↑ LICHTENSTEIN L (1953). "Aneurysmal bone cyst; further observations". Cancer. 6 (6): 1228–37. PMID 13106840.
- ↑ Szendroi M, Arató G, Ezzati A, Hüttl K, Szavcsur P (1998). "Aneurysmal bone cyst: its pathogenesis based on angiographic, immunohistochemical and electron microscopic studies". Pathol Oncol Res. 4 (4): 277–81. PMID 9887358.
- ↑ Panoutsakopoulos G, Pandis N, Kyriazoglou I, Gustafson P, Mertens F, Mandahl N (1999). "Recurrent t(16;17)(q22;p13) in aneurysmal bone cysts". Genes Chromosomes Cancer. 26 (3): 265–6. PMID 10502326.
- ↑ Oliveira AM, Perez-Atayde AR, Dal Cin P, Gebhardt MC, Chen CJ, Neff JR; et al. (2005). "Aneurysmal bone cyst variant translocations upregulate USP6 transcription by promoter swapping with the ZNF9, COL1A1, TRAP150, and OMD genes". Oncogene. 24 (21): 3419–26. doi:10.1038/sj.onc.1208506. PMID 15735689.
- ↑ Dal Cin P, Kozakewich HP, Goumnerova L, Mankin HJ, Rosenberg AE, Fletcher JA (2000). "Variant translocations involving 16q22 and 17p13 in solid variant and extraosseous forms of aneurysmal bone cyst". Genes Chromosomes Cancer. 28 (2): 233–4. PMID 10825009.
- ↑ 13.0 13.1 Leithner A, Windhager R, Lang S, Haas OA, Kainberger F, Kotz R (1999). "Aneurysmal bone cyst. A population based epidemiologic study and literature review". Clin Orthop Relat Res (363): 176–9. PMID 10379320.
- ↑ Mohan R, Sreekumaran GT (2016). "Secondary Aneurysmal Bone Cyst of the Scapula Treated by CT Guided Percutaneous Polidocanol Injection - A Case Report". J Clin Diagn Res. 10 (12): RD04–RD06. doi:10.7860/JCDR/2016/23561.9096. PMC 5296532. PMID 28208959.
- ↑ Biesecker JL, Marcove RC, Huvos AG, Miké V (1970). "Aneurysmal bone cysts. A clinicopathologic study of 66 cases". Cancer. 26 (3): 615–25. PMID 5458269.
- ↑ Ruiter DJ, van Rijssel TG, van der Velde EA (1977). "Aneurysmal bone cysts: a clinicopathological study of 105 cases". Cancer. 39 (5): 2231–9. PMID 265751.
- ↑ Vergel De Dios AM, Bond JR, Shives TC, McLeod RA, Unni KK (1992). "Aneurysmal bone cyst. A clinicopathologic study of 238 cases". Cancer. 69 (12): 2921–31. PMID 1591685.
- ↑ 18.0 18.1 Gibbs CP, Hefele MC, Peabody TD, Montag AG, Aithal V, Simon MA (1999). "Aneurysmal bone cyst of the extremities. Factors related to local recurrence after curettage with a high-speed burr". J Bone Joint Surg Am. 81 (12): 1671–8. PMID 10608377.
- ↑ Papagelopoulos PJ, Currier BL, Shaughnessy WJ, Sim FH, Ebsersold MJ, Bond JR; et al. (1998). "Aneurysmal bone cyst of the spine. Management and outcome". Spine (Phila Pa 1976). 23 (5): 621–8. PMID 9530795.
- ↑ Yamamoto T, Nagira K, Akisue T, Marui T, Hitora T, Kawamoto T; et al. (2003). "Fine-needle aspiration biopsy of solid aneurysmal bone cyst in the humerus". Diagn Cytopathol. 28 (3): 159–62. doi:10.1002/dc.10248. PMID 12619099.
- ↑ Martinez V, Sissons HA (1988). "Aneurysmal bone cyst. A review of 123 cases including primary lesions and those secondary to other bone pathology". Cancer. 61 (11): 2291–304. PMID 2835141.
- ↑ Nobler MP, Higinbotham NL, Phillips RF (1968). "The cure of aneurysmal bone cyst. Irradiation superior to surgery in an analysis of 33 cases". Radiology. 90 (6): 1185–92. doi:10.1148/90.6.1185. PMID 5656741.
- ↑ Dabska M, Buraczewski J (1969). "Aneurysmal bone cyst. Pathology, clinical course and radiologic appearances". Cancer. 23 (2): 371–89. PMID 5764977.
- ↑ Tsai JC, Dalinka MK, Fallon MD, Zlatkin MB, Kressel HY (1990). "Fluid-fluid level: a nonspecific finding in tumors of bone and soft tissue". Radiology. 175 (3): 779–82. doi:10.1148/radiology.175.3.2160676. PMID 2160676.
- ↑ Boubbou M, Atarraf K, Chater L, Afifi A, Tizniti S (2013). "Aneurysmal bone cyst primary--about eight pediatric cases: radiological aspects and review of the literature". Pan Afr Med J. 15: 111. doi:10.11604/pamj.2013.15.111.2117. PMC 3828064. PMID 24244797.
- ↑ Ozaki T, Hillmann A, Lindner N, Winkelmann W (1997). "Cementation of primary aneurysmal bone cysts". Clin Orthop Relat Res (337): 240–8. PMID 9137195.
- ↑ Reddy KI, Sinnaeve F, Gaston CL, Grimer RJ, Carter SR (2014). "Aneurysmal bone cysts: do simple treatments work?". Clin Orthop Relat Res. 472 (6): 1901–10. doi:10.1007/s11999-014-3513-1. PMC 4016447. PMID 24532435.