Wide complex tachycardia overview
|
Wide complex tachycardia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Wide complex tachycardia overview On the Web |
|
American Roentgen Ray Society Images of Wide complex tachycardia overview |
|
Risk calculators and risk factors for Wide complex tachycardia overview |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Wide complex tachycardia is defined as a cardiac rhythm of more than 100 beats per minute with a QRS duration of 120 milliseconds or more. It is critical to differentiate whether the wide complex tachycardia is of ventricular origin and is ventricular tachycardia, or if it is of supraventricular origin with aberrant conduction (SVT with aberrancy). Differentiating between these two cause of the wide complex tachycardia is critical because the treatment options are quite different for VT versus SVT with aberrancy.
Causes
Wide complex tachycardia will be due to VT in 80% of cases if there is a history of myocardial infarction (MI). Only 7% of patients with SVT will have had a prior myocardial infarction (MI). Wide complex tachycardia will be due to VT in 98% of cases if there's a history of structural heart disease.
Differential Diagnosis of Wide Complex Tachycardia
EKG Findings Suggestive of VT
History of Ischemic Heart Disease
A history of ischemic heart disease or structural heart disease suggests VT. Wide complex tachycardia will be due to VT in 80% of cases if there is a history of myocardial infarction (MI). Only 7% of patients with SVT will have had a prior myocardial infarction (MI). Wide complex tachycardia will be due to VT in 98% of cases if there's a history of structural heart disease.
The Presence of AV Dissociation
Although AV dissociation is highly suggestive of VT, it may also be seen in junctional tachycardias with retrograde block.
Example: Shown below is a wide complex tachycardia. AV dissociation is present as shown by the varying morphology highlighted by the red arrows. LBBB configuration. Absence of RS in the chest leads. The diagnosis is VT.
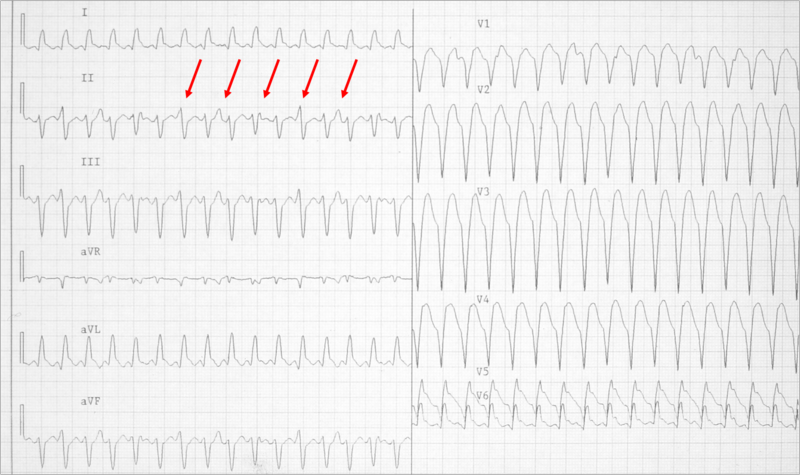
Example: Shown below is a wide complex tachycardia. AV dissociation is present as shown by the varying morphology highlighted by the red arrows. LBBB configuration. Absence of RS in the chest leads. The diagnosis is VT.

Duration of the QRS Complex
- A wide complex tachycardia with a RBBB morphology and a QRS > 0.14, or a LBBB morphology with a QRS > 0.16 suggests VT.
Morphology of the QRS Complexes
- The finding of a positive or negative QRS complex in all precordial leads is in favor of ventricular tachycardia.
- A monophasic or biphasic RBBB QRS complex in V1. But none of their patients with SVT had a preexisting RBBB. Therefore, this finding is of limited importance (A Wellens criterion).
- 80 to 85% of aberrant beats have a RBBB pattern, but ectopic beats that arise from the LV have a similar morphology.
- LBBB with a rightward axis
- LBBB with the following QRS morphology:
- R wave in V1 or V2 > 0.03 second
- Any Q wave in V6
- Onset of the QRS to nadir of the S wave in V1 > 0.06 seconds
- Notching of the S wave in V1 or V2
| Morphological criteria | ||
|---|---|---|
| LBBB pattern | ||
| Initial R more than 40 ms? | Yes ≥ VT |  |
| Slurred or notched downwards leg of S wave in leads V1 or V2? | Yes ≥ VT | |
| Beginning of Q to nadir QS > 60 ms in V1 or V2? | Yes ≥ VT | LR > 50:1 |
| Q or QS in V6? | Yes ≥ VT | LR > 50:1 |
 | ||
| RBBB pattern | ||
| Monofasic R or qR in V1? | Yes ≥ VT | |
| R taller than R' (rabbit-ear sign)? | Yes ≥ VT | LR > 50:1 |
| rS in V6? | Yes ≥ VT | LR > 50:1 |
Morphology of Premature Beats During Sinus Rhythm
- If premature ventricular contractions (PVCs) are present on a prior tracing, and if the morphology of the wide complex tachycardia is the same, then it is likely to be ventricular tachycardia.
- Previous EKG may show a preexisting intraventricular conduction delay (IVCD) which would favor SVT with abberancy.
- If there are premature atrial contractions (PAC)s with aberrant conduction, then the origin of the wide complex tachycardia may be supraventricular.
- Example: Shown below is a wide complex tachycardia. There is no AV dissociation. A RBBB morphology is present. The wide complex tachycardia resembles sinus rhythm from the same patient. The diagnosis in this patient is SVT with RBBB:

- Shown below is the ECG from the same patient as above in sinus rhythm. The QRS complex is very similiar to that during the wide complex tachycardia:

The QRS Axis
- A "northwest axis" with a QRS axis in the RUQ between -90 and +180 degrees favors ventricular tachycardia.
- The image below illustrates the "Northwest axis"also known as "Extreme Right Axis" or "No Man's Land":

Capture Beats
- Rare, but one of the strongest pieces of evidence in favor of VT.
- SVT with aberrancy rarely follows a beat with a short cycle length.
Fusion Beats
- Fusion beats are rare, but strongly suggests VT.

Vagal Manuevers
- VT is generally not affected by vagal stimulation.
- May terminate reentrant arrhythmias
Atrial Pacing
- A pacing wire is placed in the RA and the atrium is stimulated at a rate faster than the tachycardia.
- If ventricular capture occurs and the QRS is normal in duration, then one can exclude the possibility of aberrant conduction.
Onset of the Tachycardia
- Diagnosis of SVT made if the episode is initiated by a premature P wave.
- If the paroxysm begins with a QRS then the tachycardia may be either ventricular or junctional in origin.
- If the first QRS of the tachycardia is preceded by a sinus p wave with a PR interval shorter than that of the conducted sinus beats, the tachycardia is ventricular.
His Bundle Recording
- In SVT, each QRS is preceded by a His bundle potential.
- In VT there is no preceding His deflection.
- The retrograde His deflection is usually obscured by the much larger QRS complex.
Regularity of the Rhythm
Regular
- VT (slight irregularity of RR)
- SVT with aberrancy: Sinus, atrial tachycardia (AT), or flutter
- Antidromic atrioventricular reentrant tachycardia (AVRT)
Irregular
- The first 50 beats of VT can be irregular
- SVT with aberrancy: Atrial fibrillation, multifocal atrial tachycardia (MAT)
- Atrial fibrillation with bypass tract usch as WPW is a dangerous cause of a very rapid irregular rhythm as the atrial rate is conducted rapidly over the bypass tract. Shown below is the tracing of a patient with atrial fibrillation conducting down the bypass tract in WPW. Note that the rate is extremely rapid, and the rhythm is irregularly irregular. It is critical that this rhythm be recognized to avoid the administration of agents that would further accelerate conduction down the accessory pathway in this patient with WPW which could cause degeneration into ventricular fibrillation. The best treatment for this patient is Pronestyl 15 mg/kg load over 30 minutes then 2-6 mg/min gtt or DC cardioversion:

- The mechanism of SVT with aberrancy is usually concealed retrograde conduction. The ventricular beat penetrates the right branch (RB) or left branch (LB). When the next supraventricular activation front occurs that bundle is refractory and if conduction can occur, it will proceed down the other bundle. Since the RB has a longer refractory period than the LB, a right bundle branch block (RBBB) morphology is more common.
- Other mechanisms of “rate related aberrancy” are preexisting bundle branch block (BBB), physiologic (phase 3) aberration and use dependent aberration secondary to medication. In physiologic aberration, the stimulus comes to the His-Purkinje system before it has fully recovered from the previous stimulus. The ensuing activation is either blocked or conducts slowly. Again, the RB is the one more at risk. Most commonly seen at the onset of paroxysmal supraventricular tachycardia (PSVT), but can become sustained.
- In use-dependent aberration, a patient on and anti-arrhythmic (especially class Ic agents) will have a progressive decrement in ventricular conduction rate the more it is stimulated. During faster heart rates, less time is available for the drug to dissociate from the receptor and an increased number of receptors are blocked.
The R Wave Peak Time
In 2010 Joseph Brugada et al. published a new criterion to differentiate VT from SVT in wide complex tachycardias: the R wave peak time (RWPT) in Lead II.[1] To aplly the criteria, the duration of onset of the QRS to the first change in polarity (either nadir Q or peak R) is measured in lead II as shown below. If the RWPT is ≥ 50ms the likelihood of a VT very high (positive likelihood ratio 34.8). This criterion was successful in their own population of 163 selected patients and is awaiting prospective testing in a larger trial.
Example: As shown below, an R-wave to Peak Time (RWPT) of ≥ 50ms in lead II strongly suggests VT:

References
- ↑ Pava LF, Perafán P, Badiel M, Arango JJ, Mont L, Morillo CA, Brugada J (2010). "R-wave peak time at DII: a new criterion for differentiating between wide complex QRS tachycardias". Heart Rhythm : the Official Journal of the Heart Rhythm Society. 7 (7): 922–6. doi:10.1016/j.hrthm.2010.03.001. PMID 20215043. Retrieved 2012-10-13. Unknown parameter
|month=ignored (help)